Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
To understand metastatic disease in the abdomen and pelvis, one must appreciate the remarkable complexity of the peritoneum. By definition, the serosal peritoneum is a membrane that covers the lining of the abdominal and pelvic cavity and reflects over the viscera to form ligaments, mesenteries, and omenta. These reflections structurally support the organs and are conduits for the blood vessels, lymphatics, and nerves.
The network of connections formed by the peritoneal reflections serves to provide continuity between the abdominal walls and the organs therein and bridges the retroperitoneum with the peritoneum. These connections serve a physiologic role, but also can act as a pathway for the spread of disease. These processes include inflammation, infection, trauma, and, importantly, tumor.
Primary tumors of the peritoneum are rare. Metastasis is more common. Patients present with vague and nonspecific symptoms. Therefore, imaging plays a key role in the diagnosis of peritoneal disease. Because of the spaces and compartments formed by the peritoneal reflections, there are predictable patterns of disease spread. Common tumors that spread and metastasize to the peritoneum include stomach, colon, ovarian, and pancreatic cancer and lymphoma.
Peritoneal disease could not be assessed in a direct manner radiographically before the advent of cross-sectional imaging. With improving technologies such as multidetector row computed tomography (CT), positron emission tomography/computed tomography (PET/CT), magnetic resonance imaging (MRI), and ultrasound, peritoneal metastasis can now be readily evaluated.
To fully understand the peritoneum, a basic understanding of its embryologic development is necessary. The embryologic development of the peritoneum is complex. Briefly, the primitive gut is suspended within the peritoneal cavity by a dorsal and ventral primitive mesentery, which divides the peritoneum into a right and a left cavity. Unlike the ventral mesentery, the dorsal mesentery does not stop its attachment at the stomach, but continues to connect the primitive gut to the posterior abdominal wall inferiorly.
The liver develops within the ventral mesentery. The pancreas and spleen develop within the dorsal mesentery. The ventral mesentery anterior to the liver and attaching it to the anterior abdominal wall later becomes the falciform ligament, containing the umbilical vessels. The ventral mesentery between the liver and the stomach will develop into the gastrohepatic and hepatoduodenal ligaments.
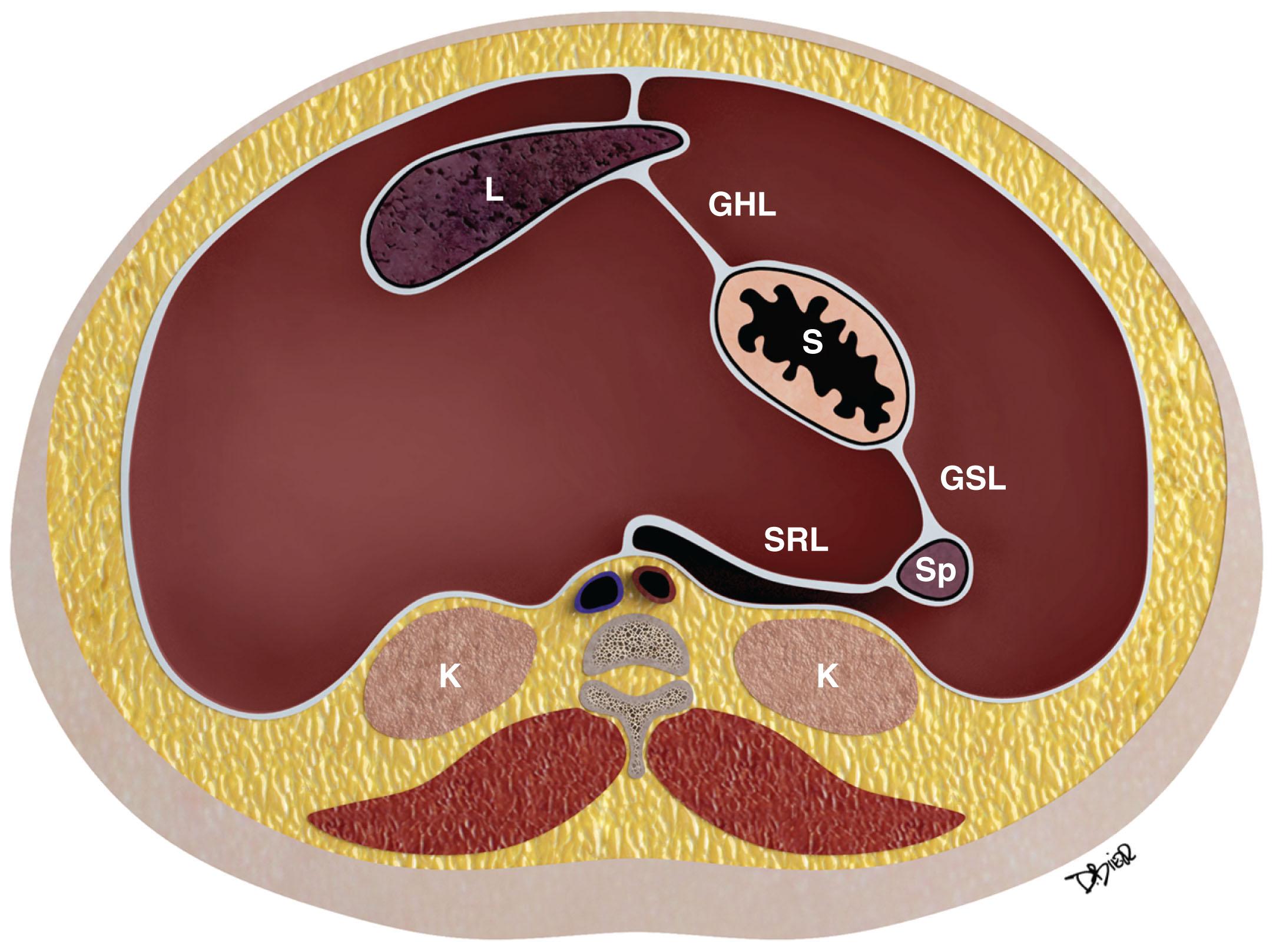
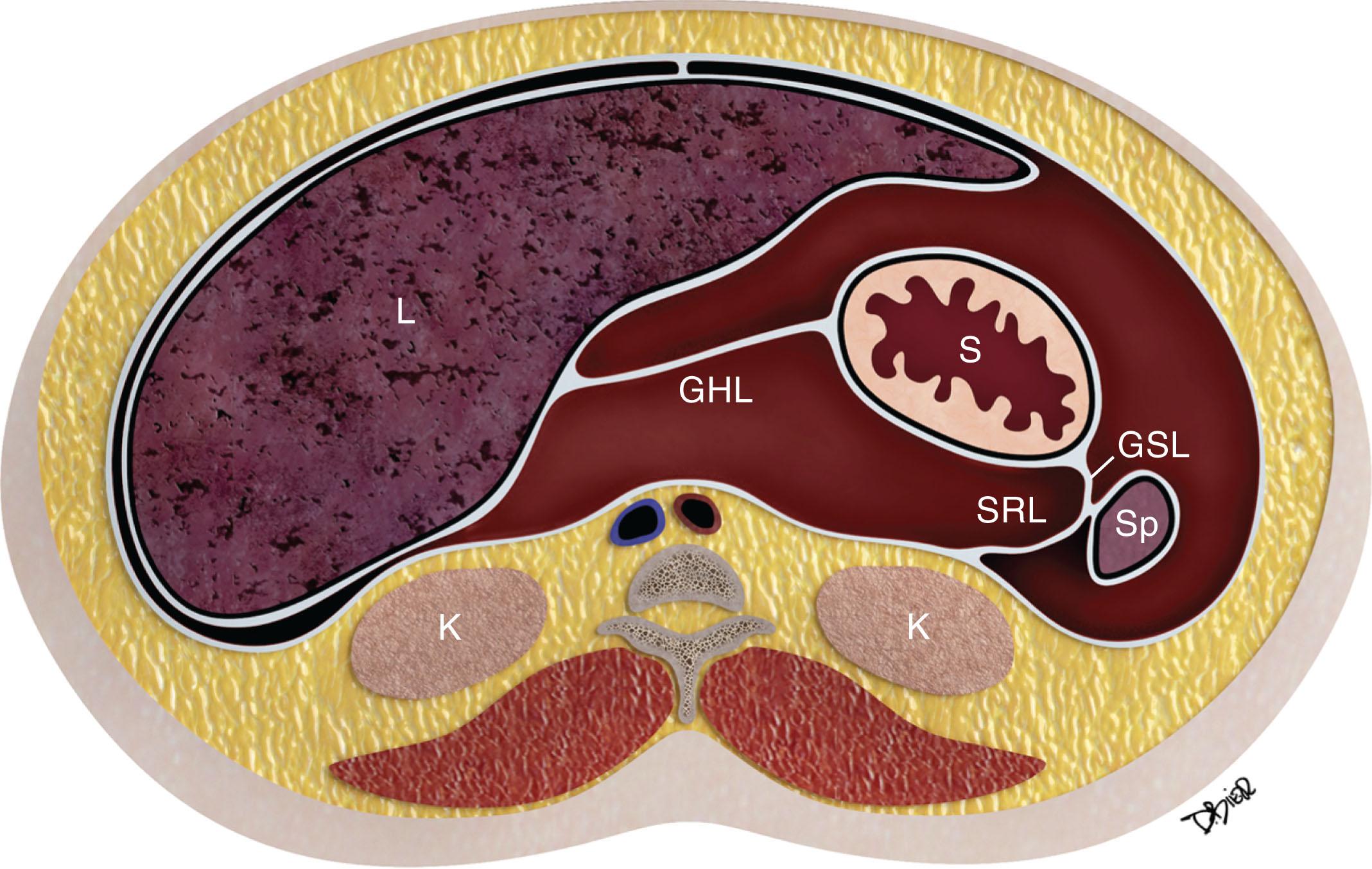
Further growth, organ development, elongation, cavitation, and rotation form the adult peritoneum ( Figs. 33.1 and 33.2 ). This includes the formation of the lesser sac, which is isolated from the remainder of the peritoneum or greater sac except at a small opening called the foramen of Winslow.
A single layer of mesothelial cells forms the peritoneum. It is separated from the submesothelial layer of connective tissue by a basal lamina. The submesothelial layer of connective tissue consists of collagen, elastic fibers, fibroblast-like cells, arteries, veins, and lymphatics. The submesothelial layer or subperitoneal space is a virtual space that allows continuity between the mesenteries, the ligaments, the abdominal wall, and the retroperitoneum.
The peritoneum normally also contains a small amount of sterile fluid for lubrication, bacterial defense, and fluid transport.
The peritoneum is classified as either visceral or parietal. The abdominal and pelvic walls are lined by the parietal peritoneum. Conversely, the visceral peritoneum covers the intraperitoneal organs or viscera and forms the omenta and mesenteries.
In males, the greater peritoneal cavity is a closed continuous cavity. Conversely, in females, it is discontinuous at the ostia of the oviducts, providing a communication between the peritoneal cavity and the lower pelvis, which is extraperitoneal.
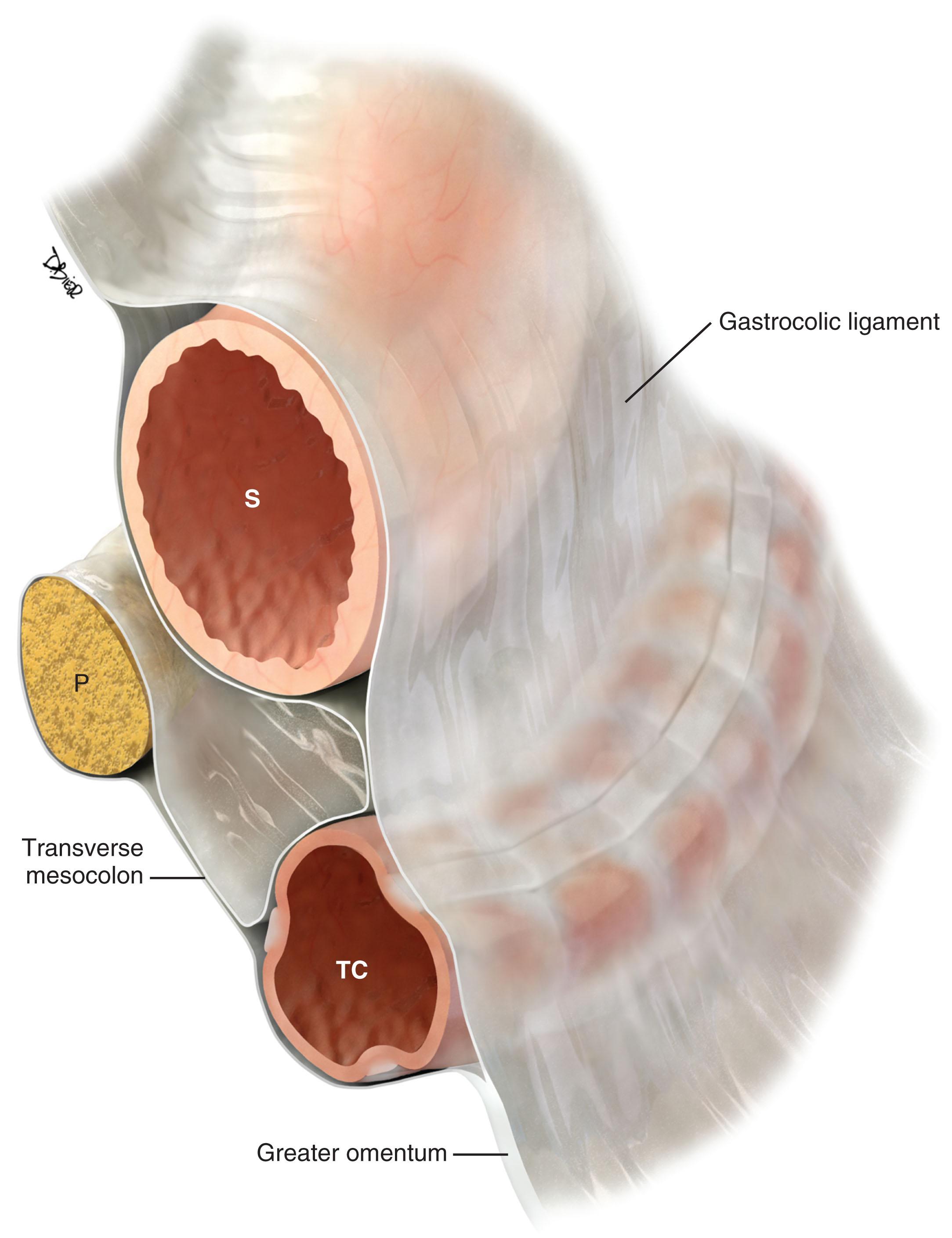
Double folds of the peritoneum result in formation of ligaments and mesenteries. They suspend and form the supporting structure for the peritoneal organs. For example, the mesentery suspends the small bowel within the peritoneal cavity and also serves to carry the arteries, lymphatics, and nerves. The omenta are formed from a double fold of the visceral peritoneum that extends from the stomach ( Figs. 33.3 and 33.4 ). The peritoneal cavity is divided into various interconnecting compartments by the ligaments and mesenteries.
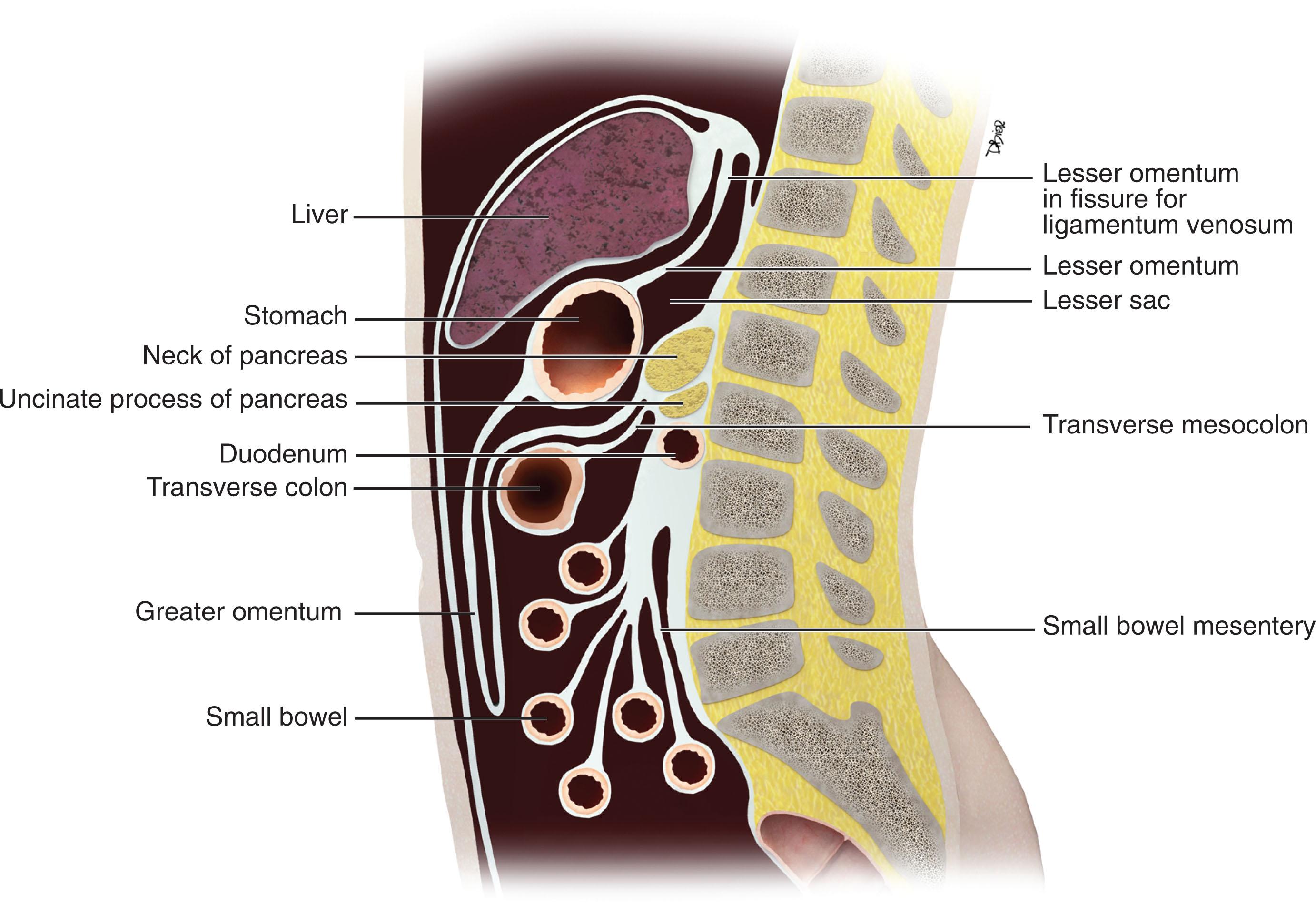
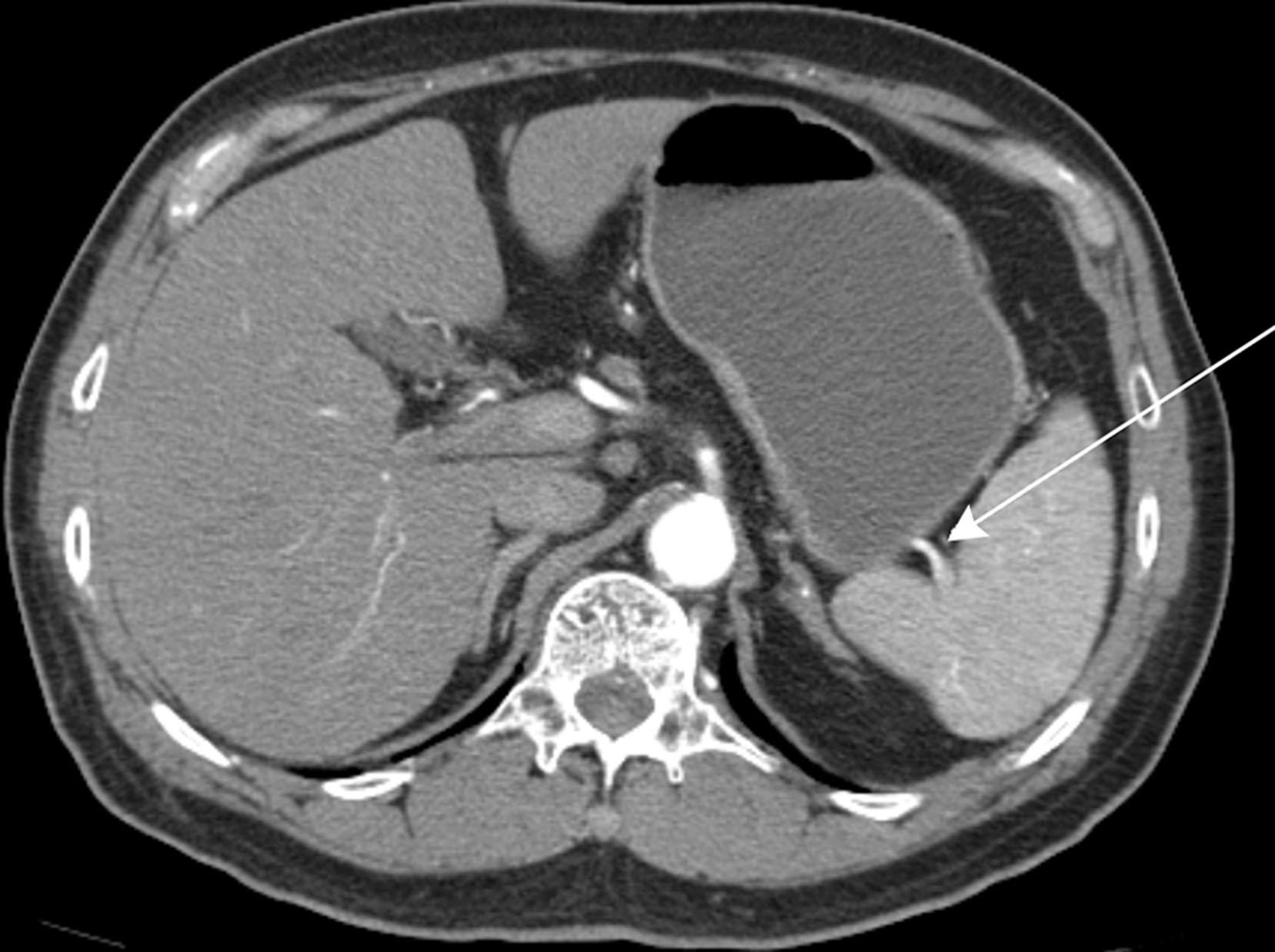
The peritoneal cavity is divided into a supramesocolic and an inframesocolic space by the transverse mesocolon ( Fig. 33.5 ). The supramesocolic space is further divided into the right and left supramesocolic space by the falciform ligament. The right supramesocolic space also is subdivided into the anterior perihepatic space and a posterior compartment known as the lesser sac. The right and left supramesocolic space communicates via the foramen of Winslow, allowing communication between the lesser sac and the remainder of the peritoneal cavity or greater sac.
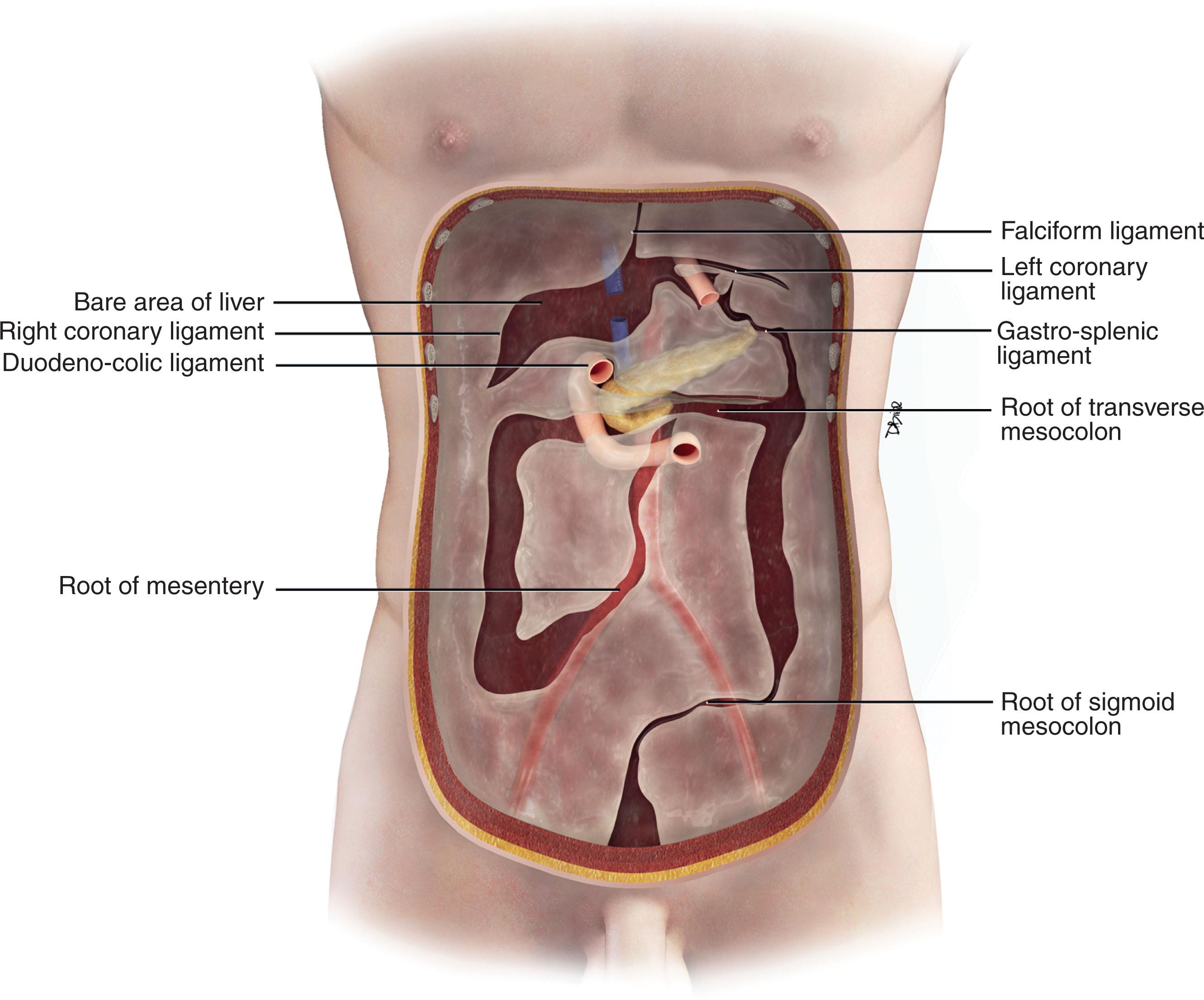
Important supporting ligaments in the supramesocolic space include the gastrohepatic ligament, hepatoduodenal ligament, gastrocolic ligament, gastrosplenic ligament, and splenorenal ligament ( Figs. 33.6 to 33.8 ). The ligaments are anatomically connected and continuous, and their location and relationship can be identified by certain landmarks, mostly vasculature ( Table 33.1 ).

| LIGAMENT | ORGAN RELATIONSHIP | LANDMARKS |
|---|---|---|
| Gastrohepatic ligament | Lesser curvature of the stomach to left hepatic lobe | Left gastric vessels and left gastric nodal station |
| Hepatoduodenal ligament | Lesser curvature of the stomach to the hepatic hilum | Portal vein, hepatic artery, extrahepatic bile duct, and nodal stations |
| Gastrocolic ligament/supracolic omentum | Greater curvature of the stomach to the body of the transverse colon | Perigastric branches of the left gastroepiploic vessels with anastomosis to the right gastroepiploic vessels |
| Greater omentum | Transverse colon extending as an apron anterior to the small bowel | Epiploic vessels and branches of the gastroepiploic vessels |
| Gastrosplenic ligament | Continuous and to the left of the gastrocolic ligament, from the greater curvature of the fundus and upper body of the stomach to the splenic hilum | Short gastric vessels and left gastroepiploic vessels |
| Splenorenal ligament | Continuity between the spleen and the tail of the pancreas | Distal splenic artery or proximal splenic vein |
The inframesocolic compartment is divided into a right and a left inframesocolic space by the obliquely oriented small bowel mesentery. The ascending colon provides the lateral border of the right inframesocolic space. The inframesocolic compartment consists of the root of the mesentery, the jejunal mesentery, the ileal mesentery, the ascending mesocolon, the descending mesocolon, the sigmoid mesentery, and the pelvic floor and peritoneal folds ( Table 33.2 ).
| LIGAMENT | ORGAN RELATIONSHIP | VASCULAR LANDMARKS |
|---|---|---|
| Root of mesentery | From the horizontal portion of the duodenum to the right iliac fossa | Superior mesenteric artery, superior mesenteric vein, and ileocolic artery and vein |
| Ileal mesentery | From the root of the mesentery to the ileum | Ileal artery and veins |
| Ascending mesocolon | Root of the mesentery to the ascending colon | Right colic artery and vein, cecal artery and vein |
| Jejunal mesentery | From the base of the mesentery to the jejunum | Jejunal artery and vein |
| Descending mesocolon | Base of the transverse mesocolon along the tail of the pancreas to the descending colon | Left colic artery and vein |
| Sigmoid mesocolon | Root of the sigmoid mesocolon | Sigmoid arteries, superior hemorrhoidal artery and vein |
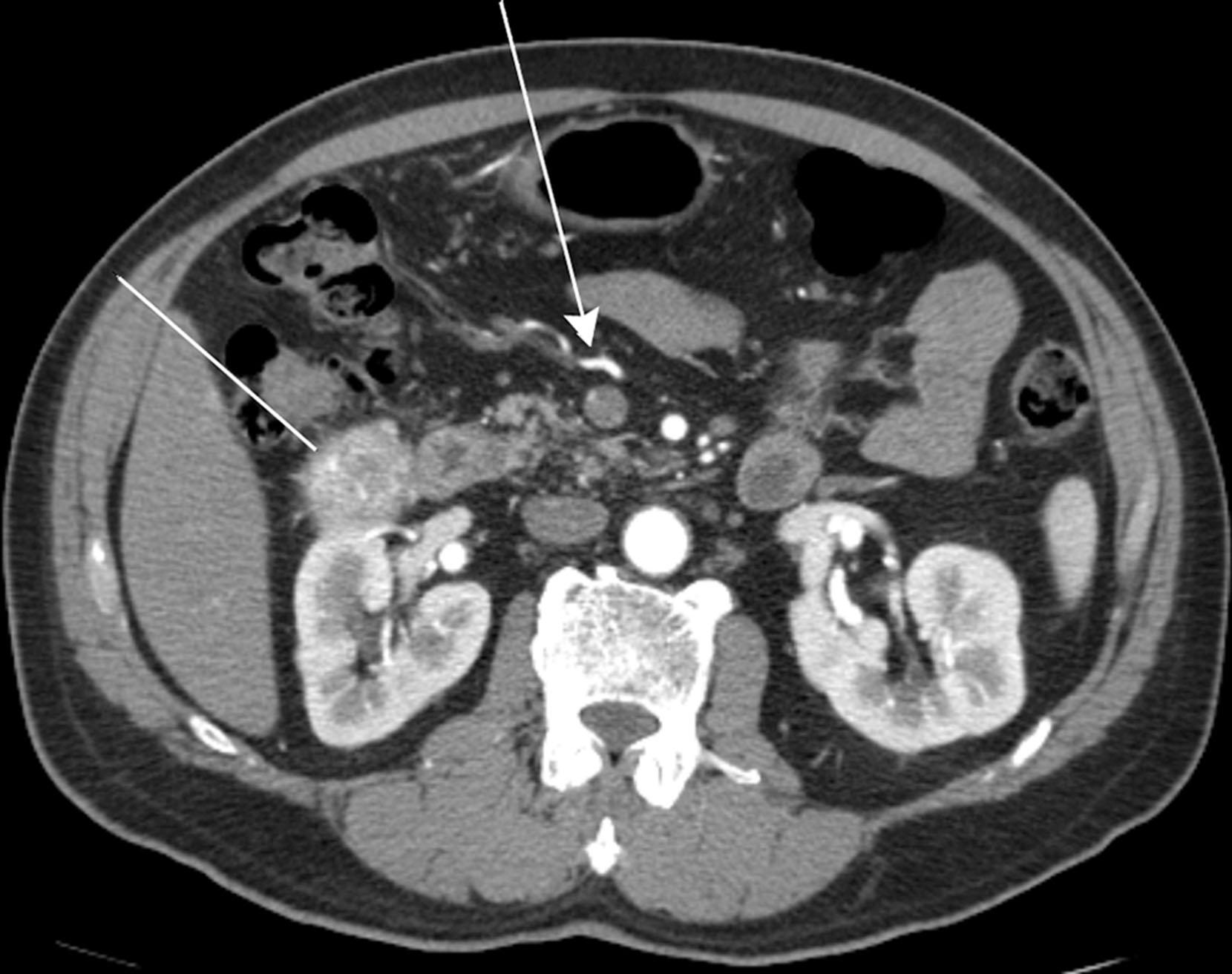
Peritoneal folds or reflections in the pelvis also result in potential spaces and compartments ( Figs. 33.9 and 33.10 ). The urinary bladder, obliterated umbilical arteries, and inferior epigastric vessels indent upon the parietal peritoneum to form the anterior and posterior paravesicular spaces.
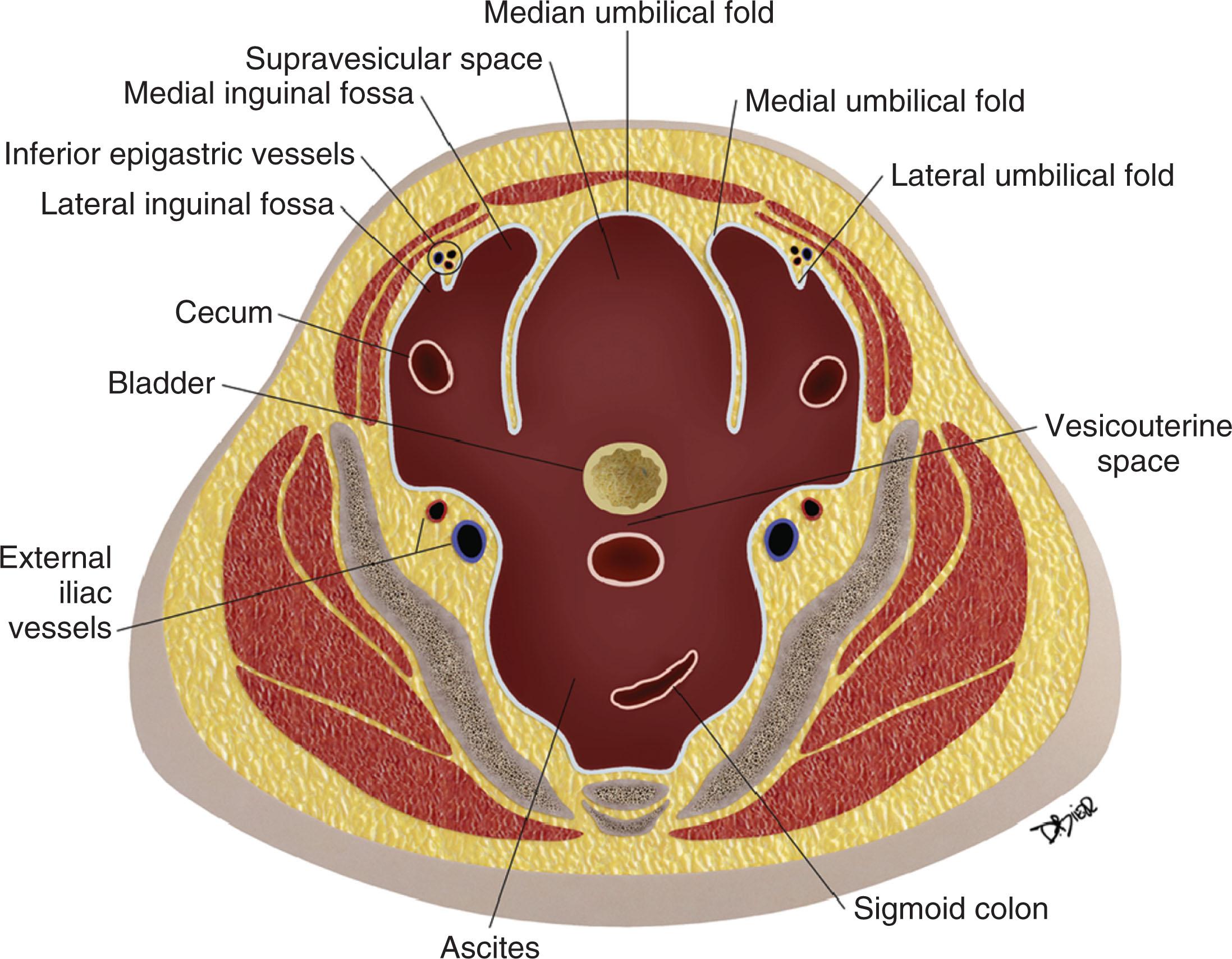
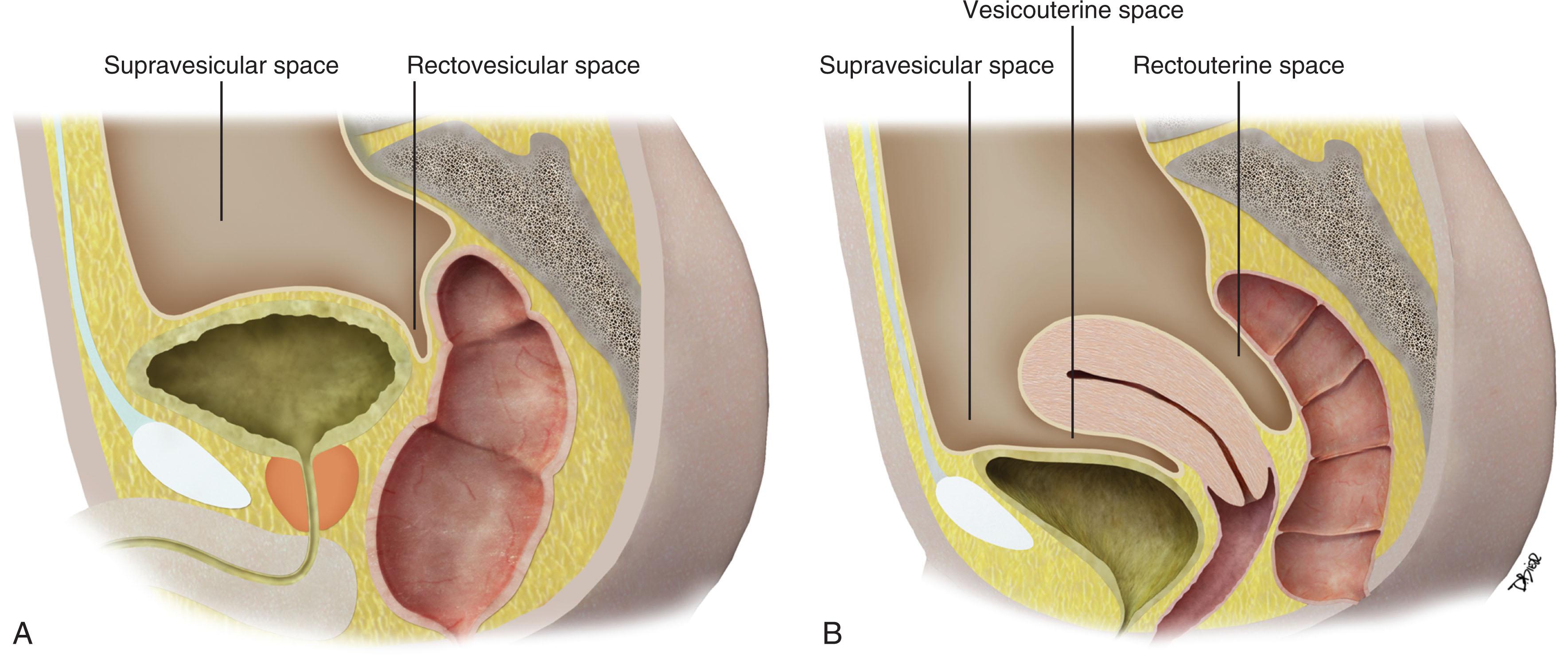
The anterior paravesicular space is further divided into the supravesicular space and medial and lateral inguinal fossae. These compartments are demarcated by the median, medial, and lateral umbilical folds, each of which can be identified by the urachus, obliterated umbilical arteries, and inferior epigastric vessels, respectively.
The lateral inguinal fossa is the site for the internal inguinal ring and can contain portions of the cecum or sigmoid colon. The medial inguinal fossa can also contain portions of the cecum or sigmoid colon and is the site for the femoral canal.
The posterior paravesicular space is demarcated by peritoneal coverings of the rectum and bladder to form the rectovesicular and pararectal space. In the female, the rectovesicular space is further divided into the vesicouterine recess and rectouterine space (cul-de-sac).
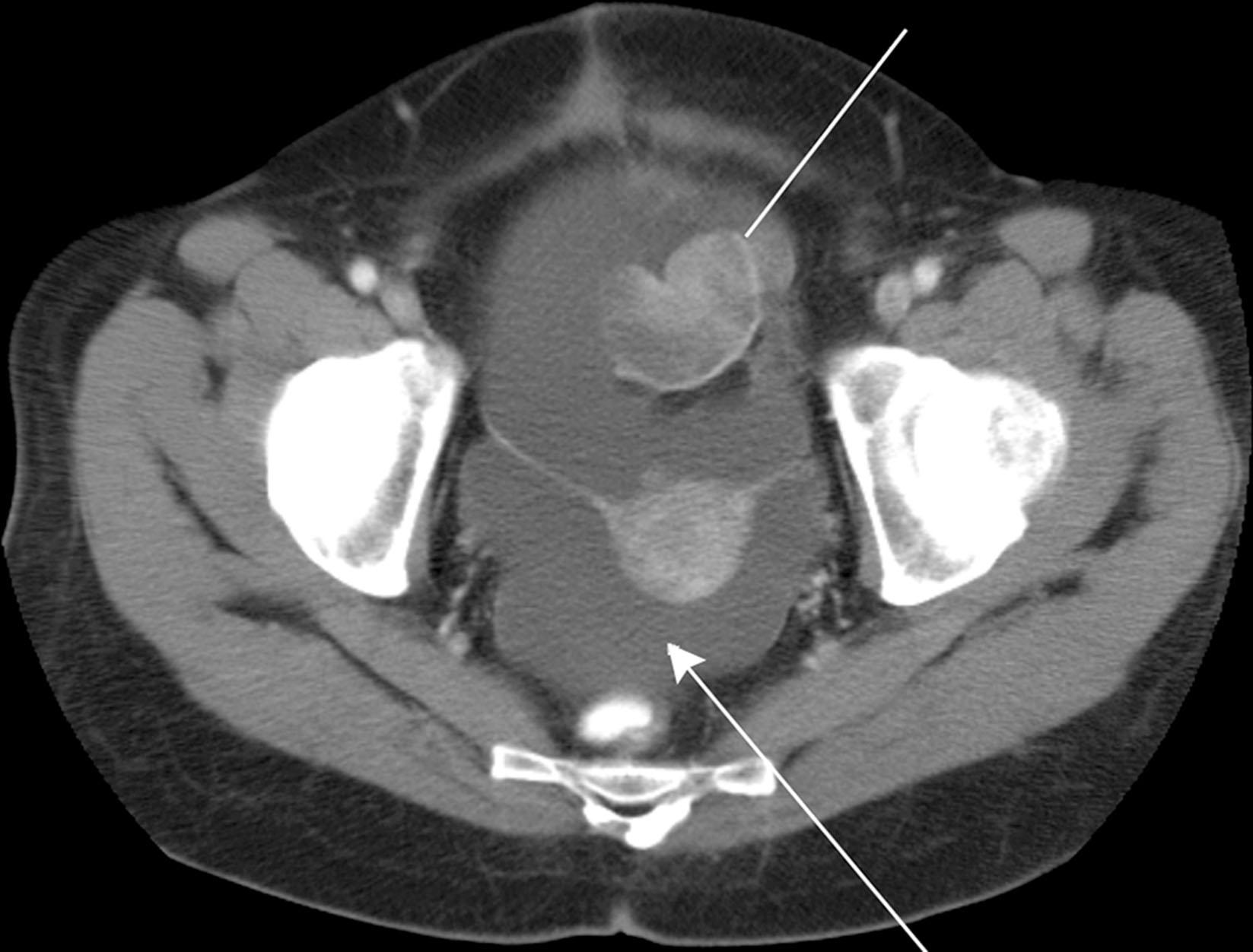
These large potential spaces can be easily delineated when there is accumulation of ascites, abscesses, metastasis, and other disease processes ( Figs. 33.11 and 33.12 ).
Embryologic development of the peritoneum is complex; basic knowledge of its development aids in an understanding of disease spread.
Peritoneum lines the abdominal and pelvic walls and organs, aiding in lubrication, organ support, movement, and host defense.
Foldings of the peritoneum form the ligaments and mesenteries, suspending and supporting internal organs.
Ligaments and mesenteries create the compartments and potential spaces within the abdominal and pelvic cavity.
![Figure 33.11, Computed tomography with intravenous contrast. Ascites in a 13-year-old with rhabdomyosarcoma. Ascites fill the pelvis, optimizing visualization of the anterior paravesicular spaces. The lateral and medial inguinal fossae are separated by the lateral umbilical fold (landmarked by the inferior epigastric vessels [ arrow ]). The supravesicular space lies in between the medial umbilical fold, which is the site of the obliterated umbilical vein ( line ). Figure 33.11, Computed tomography with intravenous contrast. Ascites in a 13-year-old with rhabdomyosarcoma. Ascites fill the pelvis, optimizing visualization of the anterior paravesicular spaces. The lateral and medial inguinal fossae are separated by the lateral umbilical fold (landmarked by the inferior epigastric vessels [ arrow ]). The supravesicular space lies in between the medial umbilical fold, which is the site of the obliterated umbilical vein ( line ).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/PeritonealCavityandGastrointestinalTract/10_3s20B9780323695381000331.jpg)
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here