Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Perioperative applications of transesophageal echocardiography (TEE) include monitoring, diagnosis, and procedural guidance. The role of TEE in cardiac surgery, noncardiac surgery, interventional procedures, and critical care continues to evolve.
In noncardiac surgery, intraoperative TEE serves as a routine monitor or as a rescue tool in life-threatening emergencies.
TEE aids in decision making during cardiac surgery, and three-dimensional (3-D) TEE adds incremental value in intraoperative assessments.
TEE is integral to structural heart interventions and is a key component of multimodality imaging.
Echocardiography plays a vital role in the diagnosis and management of shock.
Applications of transthoracic echocardiography (TTE) in the perioperative setting are expanding.
Focused cardiac ultrasound is performed and interpreted at the point of care, and addresses specific questions relevant to the clinical context.
Critical care societies have proposed distinct competencies and guidelines for critical care echocardiography beyond those included in perioperative TEE guidelines. The skill set of the intensivist performing echocardiography overlaps with that of the intraoperative echocardiographer and includes other unique components.
Basic knowledge of echocardiography is an expectation of anesthesiology training.
Simulation is an effective training tool when integrated within a multimodal, curriculum-based approach to echocardiography education.
The editors and publisher would like to thank Drs. Georges Desjardins, Daniel P. Vezina, Ken B. Johnson and Michael K. Cahalan for contributing a chapter on this topic in the prior edition of this work. It has served as the foundation for the current chapter.
Echocardiography is an invaluable tool used throughout the perioperative period. Image acquisition and interpretation occur at the point of care, enabling real-time integration of the findings in the context of the patient’s clinical condition. Transesophageal echocardiography (TEE) has broad functionality in the perioperative environment. TEE serves as an intraoperative monitor, provides detailed structural and functional information, facilitates diagnosis of pathology, and guides percutaneous interventions. Applications of TEE have expanded within cardiac surgery, and into the realms of noncardiac surgery, catheter-based procedures, and critical care. As the use of clinical ultrasound grows in modern anesthetic practice, perioperative clinicians are also beginning to embrace transthoracic echocardiography (TTE). Critical care echocardiography shares many similarities with intraoperative echocardiography, but is simultaneously evolving under the larger umbrella of critical care ultrasonography. This chapter provides a historical synopsis and summary of imaging techniques and echocardiographic views and discusses applications of TEE and TTE in perioperative care.
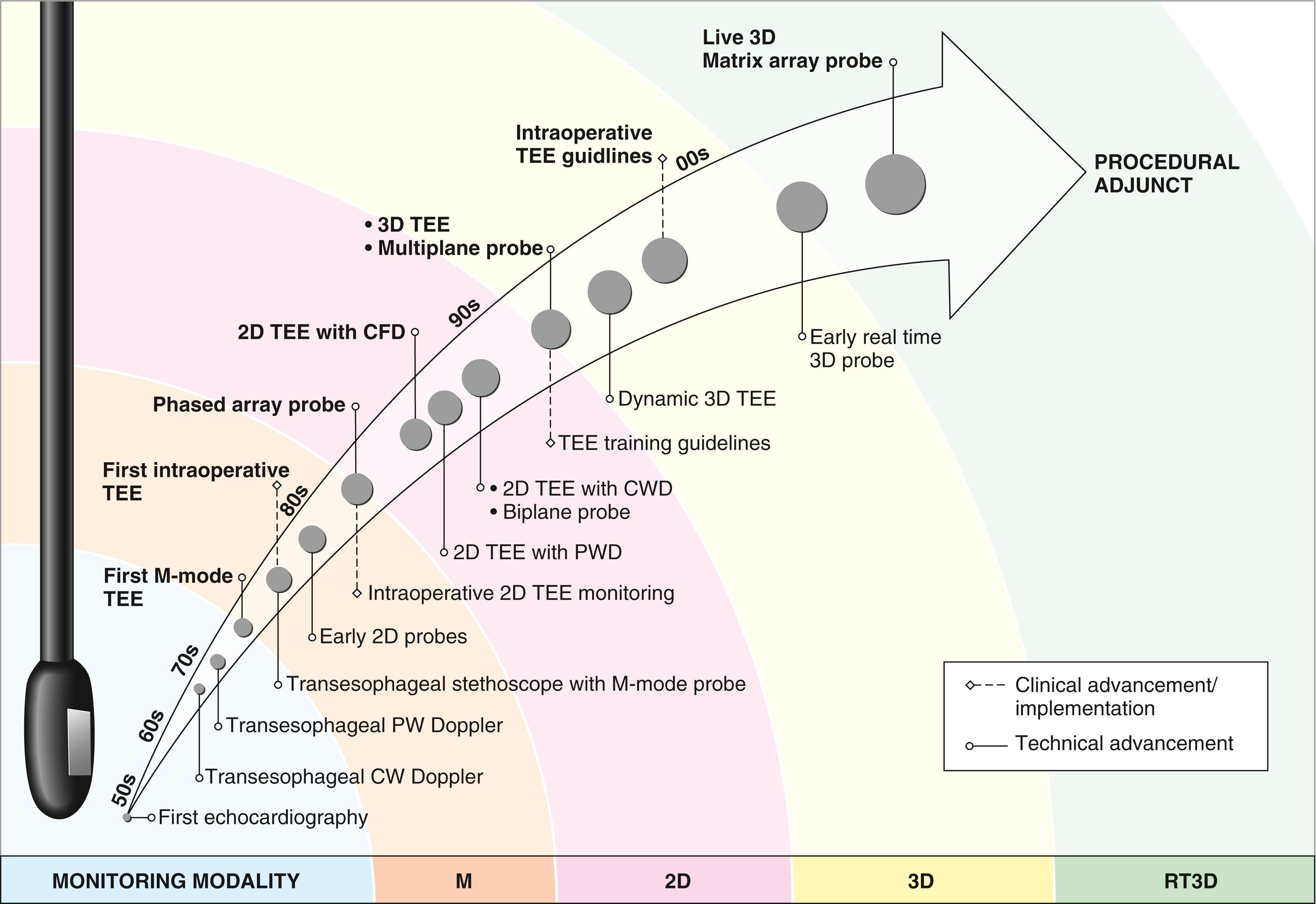
Decades of evolution and advancement have led to the current state of perioperative TEE ( Fig. 37.1 ). Clinical echocardiography first emerged in the 1950s with the use of motion mode (M-mode) ultrasound to record signals from cardiac structures. Nearly two decades later, the first intraoperative echocardiography was performed with epicardial imaging. The first practical clinical application of TEE was reported in 1976. Soon after, a group reported the first use of intraoperative TEE and described its utility in monitoring left ventricular (LV) function during cardiac surgery. In the 1980s, the mounting of two-dimensional (2-D) transducers onto modified flexible gastroscopes created more versatile probes, and pioneering anesthesiologists and cardiologists began to demonstrate the usefulness of TEE as an intraoperative monitor. Further advancements such as transducers with combined 2-D and Doppler capabilities, biplane imaging, multiplane imaging, and pediatric probes unlocked the diagnostic potential of intraoperative TEE. Real-time three-dimensional imaging (RT-3D) entered the scene in the mid-2000s, and since then its intraoperative use has grown exponentially. Advances in probe technology and improved computing power continue to further the practicality of three-dimensional (3-D) image acquisition.
Prior to the introduction of TEE in 1976, significant advances in 2-D transthoracic imaging occurred, leading to better visualization of cardiac structures. Production of commercially available instruments soon followed. In the intensive care units (ICUs), some clinicians incorporated echocardiography in the evaluation of cardiac function in acute respiratory distress syndrome and sepsis. TTE was not widely disseminated in ICUs, however, as the intensivist’s tool of choice at the time was the pulmonary artery catheter. During the late 1990s to 2000s, the use of pulmonary artery catheters declined, and TTE simultaneously gained more traction in the ICUs. With the miniaturization of equipment and emphasis on point-of-care ultrasound, use of echocardiography as a hemodynamic monitor and diagnostic tool in the ICU continues to increase.
While a thorough discussion of ultrasound physics is beyond the scope of this chapter, a basic understanding of fundamental concepts is requisite for any echocardiographer. Sound is a mechanical, longitudinal wave of vibrations propagated through a medium. Several parameters describe sound waves including frequency, wavelength, amplitude, and propagation speed. Ultrasound waves are sound waves with frequencies above the audible human range (20-20,000 hertz [Hz]). Echocardiography typically uses frequencies between 2 and 12 megahertz (MHz). Ultrasound transducers use piezoelectric elements to convert ultrasound energy into electrical energy and vice versa. Transducers function both as transmitters and receivers of ultrasound signals. 2-D echocardiography uses a phased-array transducer, which has a row of electrically interconnected piezoelectric elements.
As ultrasound energy propagates through tissue, interactions between the wave and tissue result in absorption, divergence, reflection, and scattering of the energy. Reflection of ultrasound energy at tissue interfaces forms the basis of image generation. These sound-tissue interactions reduce the intensity of the ultrasound signal, and this attenuation limits the depth of imaging. Transmitted energy at tissue interfaces often undergoes refraction and changes directions, contributing to imaging artifacts.
The accurate display of an image depends on imaging resolution, components of which include spatial resolution, temporal resolution, and contrast resolution ( Table 37.1 ). Spatial resolution can be described according to the three beam dimensions: axial, lateral, and elevational. Image formation involves a tradeoff between spatial resolution and depth of penetration. Higher frequency (shorter wavelength) transducers provide superior axial resolution, but limited penetration depth due to attenuation. Lower frequencies (longer wavelengths) penetrate more deeply at the expense of axial resolution. Higher frequencies are better for imaging superficial structures; lower frequencies are better for deeper structures.
| Description | Practical points | |
|---|---|---|
| Spatial resolution | The ability to discriminate between two closely-spaced objects The minimum distance necessary between two structures so that they are displayed as separate objects |
Determines image details Factors that improve spatial resolution often come at the expense of decreased temporal resolution and vice versa |
| Axial | Differentiates between objects along the length of the ultrasound beam | Higher frequency transducers have shorter wavelengths and better axial resolution Axial resolution is superior to lateral resolution |
| Lateral | Discriminates side-to-side (or horizontal) relative to the direction of the beam | Determined by the beam width Best at the focal point of the beam |
| Elevational | Discriminates between objects vertical to the plane of the ultrasound beam | Determined by the beam height Best at the focal point of the beam |
| Temporal resolution | The ability to accurately display a structure’s motion with respect to time | The higher the frame rate, the better the temporal resolution Factors that decrease the time to scan the sector (e.g., decreasing the imaging depth or creating a narrower imaging sector) improve temporal resolution |
| Contrast resolution | The ability to resolve subtle differences in echogenicity, which are displayed as different shades of gray | Improved by harmonic imaging, use of contrast agents, B-color maps, and post-processing controls |
Formation of ultrasound images relies on several assumptions: (1) ultrasound energy propagates in a straight line; (2) all returning echoes originate from the central beam, which is extremely thin; (3) echoes return to the transducer after one reflection; (4) attenuation is constant; and (5) the speed of sound is constant, therefore the depth of a reflector is proportional to the round-trip transit time. Violations of these assumptions result in imaging artifacts. Spectral and color flow Doppler (CFD) and 3-D images are also susceptible to imaging artifacts.
Key ultrasound modalities used in echocardiography include motion mode (M-mode), 2-D imaging, Doppler (spectral and color flow), and Doppler tissue imaging (DTI). Table 37.2 highlights important aspects of these techniques. Additional techniques may be applied in specific contexts and are introduced in the next section.
| Modality | Description/Features |
|---|---|
| Brightness Mode (B-mode) |
|
| Motion Mode (M-mode) |
|
| Two-Dimensional (2D) |
|
| Doppler |
|
| Pulsed-Wave Doppler (PWD) |
|
| Continuous Wave Doppler (CWD) |
|
| Color Flow Doppler (CFD) |
|
| Doppler Tissue Imaging (DTI) |
|
Strain and strain-rate imaging techniques (also called cardiac mechanics or myocardial deformation) are used to quantify global and regional ventricular function. Strain is the relative change in shape or size of an object as a result of an applied force. In the context of the myocardium, it is the fractional change in the length of a segment relative to its baseline and expressed as a percentage. Positive strain indicates lengthening or thickening and negative strain represents shortening or thinning. Three axes are relevant to myocardial deformation: longitudinal, circumferential, and radial. Normal deformation patterns during systole are longitudinal shortening (negative strain), circumferential shortening (negative strain), and radial thickening (positive strain).
Methods for strain analysis include DTI and the more commonly used speckle tracking echocardiography (STE). DTI measures velocities at two points in the myocardium and derives the strain and strain rate. STE, in contrast, tracks unique acoustic speckles in the myocardium over a series of frames and derives strain and strain rate from the change in distance. Duncan and colleagues have written an excellent review on perioperative strain and strain-rate imaging.
Harmonic imaging is a processing technique used to improve the quality of 2-D images. A sound wave propagates nonlinearly through tissue, distorting the wave’s shape. This produces harmonic frequencies, which are integer multiples of the fundamental frequency originally transmitted by transducer. Signals return to the transducer at both the fundamental frequency and harmonic frequencies. Harmonic imaging typically creates images from the second harmonic frequency and filters the fundamental frequency signals. Harmonic imaging increases contrast resolution, improves signal-to-noise ratio, and decreases some artifacts. Disadvantages include slightly decreased spatial resolution and thickened appearance of some cardiac structures.
Contrast echocardiography can be used to improve diagnostic evaluation and enhance suboptimal images. Two methods of contrast echocardiography include injection of agitated saline or injection of commercially available contrast agents. Agitated saline can be used to identify the presence of intracardiac right-to-left shunt, because microbubbles created by agitation do not cross the pulmonary circulation. Commercially available contrast agents use encapsulated microbubbles of high-density gas and are able to traverse the pulmonary circulation, allowing for opacification of the left side of the heart. Perioperative applications of contrast echocardiography include improved endocardial border delineation for assessment of function, assessment of regional wall motion, and exclusion of intracardiac thrombus or mass.
3-D imaging provides information that complements the findings from the 2-D examination. Transducers with 3-D capabilities contain thousands of piezoelectric elements in a rectangular (or matrix) array configuration and create pyramidal-shaped images. The optimal 3-D image involves tradeoffs between temporal resolution, spatial resolution, and sector size. 3-D imaging is susceptible to the same artifacts as 2-D imaging and additional artifacts unique to 3-D image construction. We encourage the interested reader to refer to published 3-D echocardiography guidelines as well as a practical overview focused on intraoperative 3-D image acquisition.
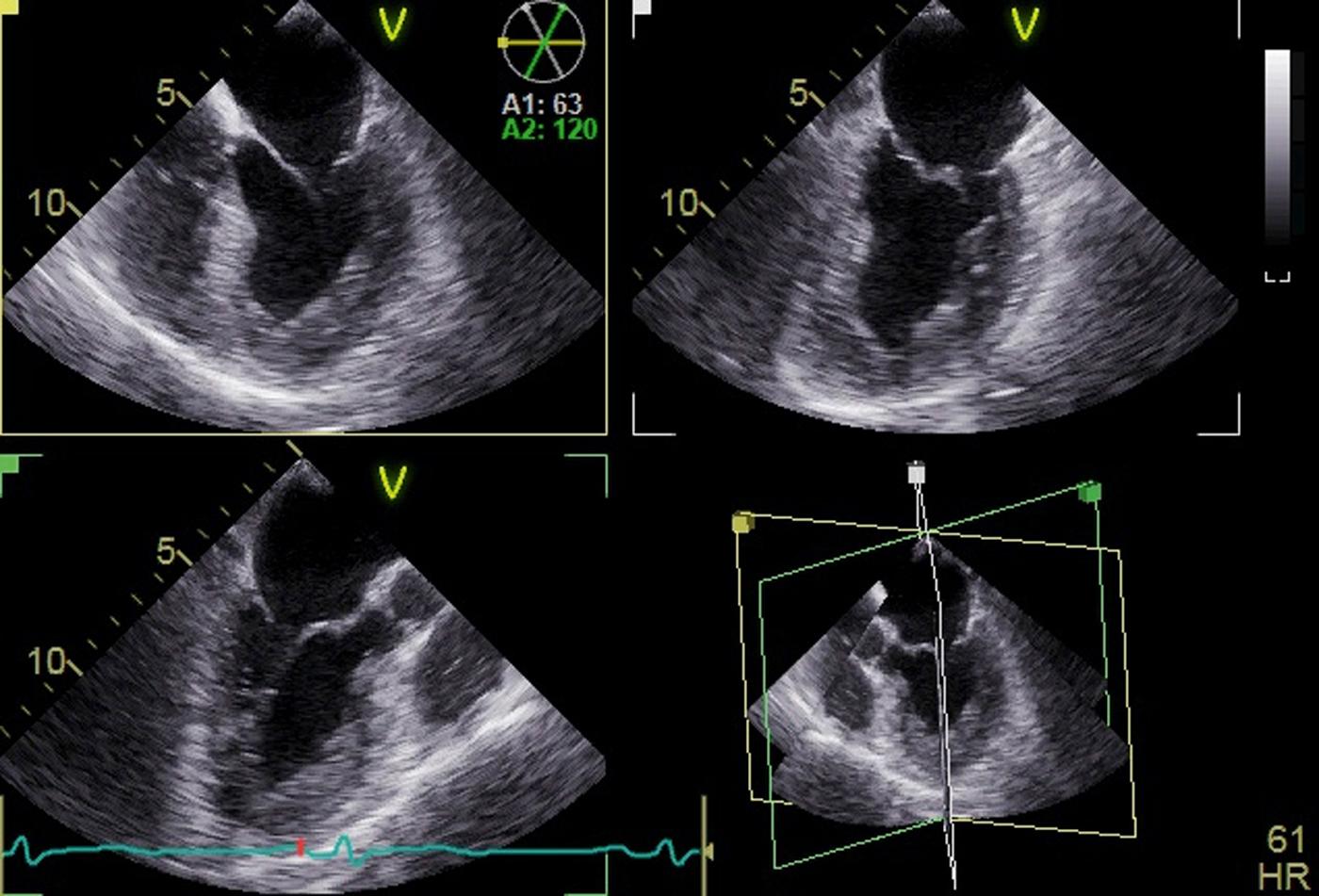
Matrix array (3-D) transducers have multiplane imaging capabilities and can simultaneously display two or more live 2-D imaging planes. In biplane imaging, the first image serves as the reference view, and the second image is obtained by rotating the scanning plane around the longitudinal axis of the reference view. The secondary image can also be adjusted by tilting the imaging plane in the elevational or lateral axis. Multiplane imaging allows simultaneous display of multiple rotatable imaging planes ( Fig. 37.2 ). Box 37.1 lists common perioperative applications of multiplane imaging.
Simultaneous visualization of segmental wall motion
Characterization of the mechanism and origin of valvular regurgitation
Procedural guidance during percutaneous closure of atrial septal defect
Guidance of transseptal puncture for transcatheter left atrial appendage and mitral valve procedures
Evaluation of the left atrial appendage morphology and exclusion of thrombus
3-D images can be displayed live or in “real time.” RT-3D imaging acquires data over a single heartbeat; some authors refer to this as 4-D imaging. The proprietary nomenclature varies, but there are three main RT-3D modes of differing sector size:
Narrow sector: this mode displays a pyramidal volume with the best temporal and spatial resolution of the live modes. The major limitation is that it often does not capture an entire structure of interest ( Fig. 37.3 ).
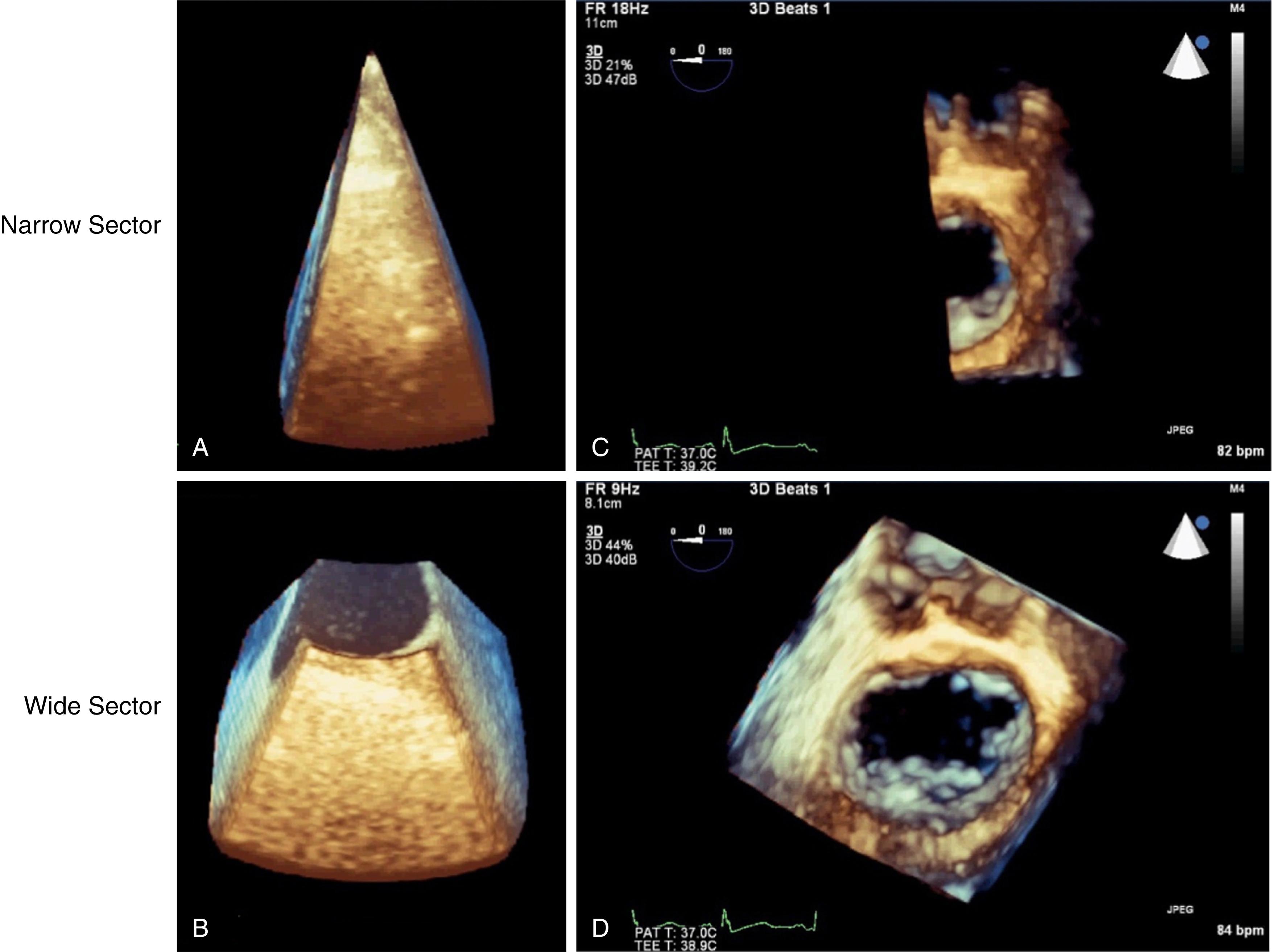
Wide sector: this mode “zooms in” on a selected region of interest. There is a decrease in temporal and spatial resolution compared to narrow sector imaging. Images are easy to acquire. This mode is ideal for real-time image manipulation (see Fig. 37.3 ).
Full-volume: full-volume mode has the largest imaging sector. Live full-volume images have reduced temporal and spatial resolution. Ideally, acquisition of full-volume images occurs over multiple beats. Live full-volume mode has utility when multiple-beat acquisition is not feasible.
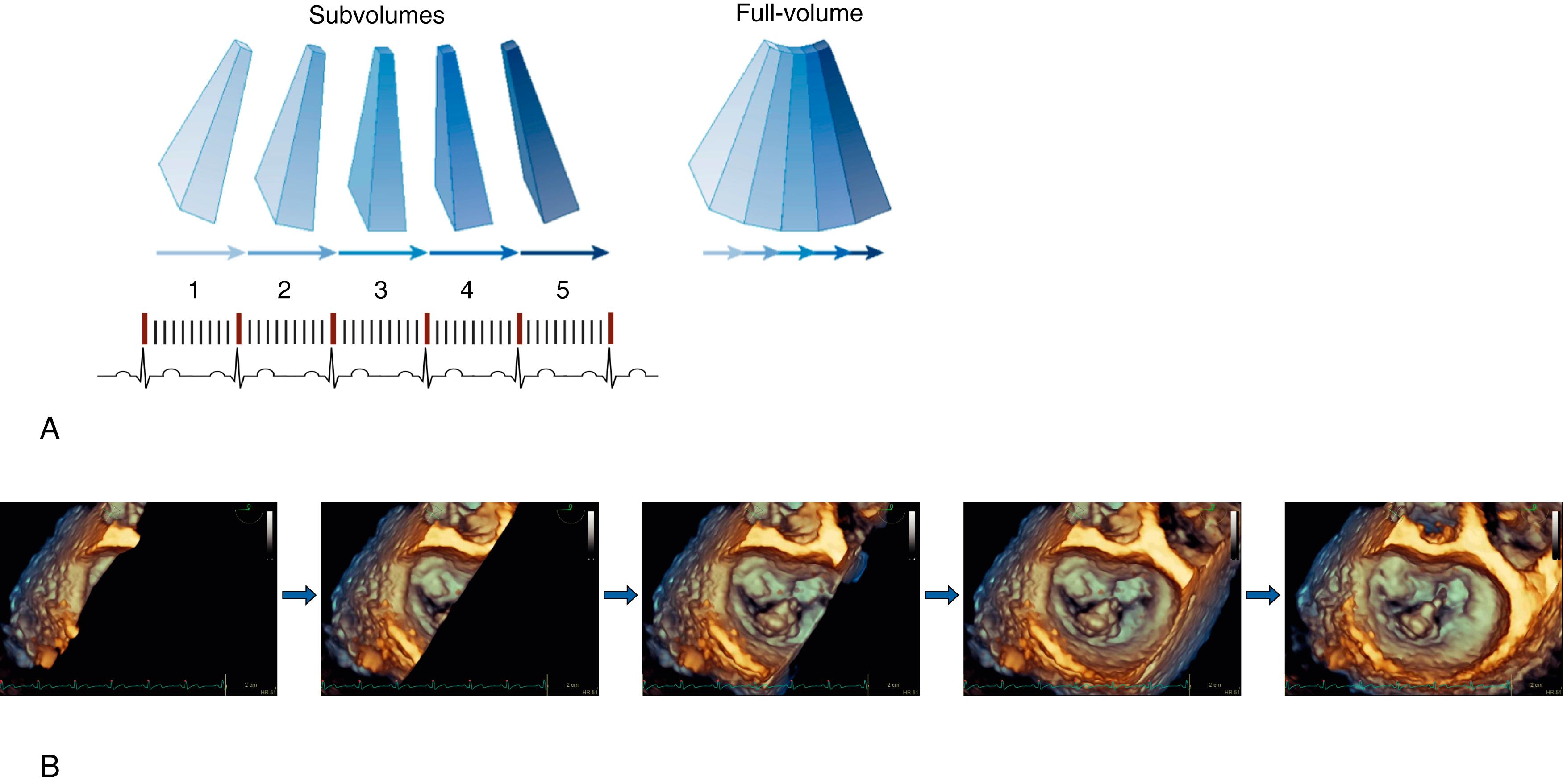
Gated acquisition divides the imaging volume into multiple narrow subvolumes that are acquired over a specified number of heartbeats. “Stitching” the subvolumes together creates the final image. In order to obtain the subvolumes at the same time in the cardiac cycle, image acquisition is gated to the R-wave of the electrocardiogram (ECG). Gated acquisition requires normal cardiac rhythm and the absence of electrical interference and respiratory variation.
Wide sector: multiple-beat gated acquisition using wide sector mode significantly improves the temporal resolution of the “zoomed in” view. Spatial resolution marginally improves.
Full-volume: this mode has the largest sector size with optimal spatial resolution and high temporal resolution ( Fig. 37.4 ; Video 37.1).
CFD may be incorporated with any of the modalities, but leads to a reduction in temporal resolution. Optimal CFD images are obtained using R-wave gated multiple beat acquisitions.
Multiplanar reformatting enables alignment of orthogonal planes to accurately measure linear dimensions and areas (e.g., planimetry of stenotic orifice, annular area).
Quantitative applications exist for 3-D imaging and eliminate some of the geometric assumptions required in 2-D imaging calculations. Example analyses include calculation of ventricular ejection fraction (EF), analysis of mitral valve structure, and dynamic annular measurements. The degree of automation and need for post-processing manipulation vary. Some analyses are performed exclusively offline, making them useful in research, but less applicable to intraoperative decision making.
The American Society of Anesthesiology (ASA) and Society of Cardiovascular Anesthesiologists (SCA) issued perioperative TEE practice guidelines in 1996, categorizing indications for TEE in various clinical settings. An updated version in 2010 recommended the indications for perioperative TEE based on literature review and expert opinion. In the absence of contraindications, TEE should be used in all adult open heart and thoracic aortic surgical procedures. It should be considered in coronary artery bypass graft surgeries to confirm diagnostic information, detect pathology, influence the anesthetic or surgical plan, and assess surgical results. It is recommended that TEE be considered on a case-by-case basis in small children undergoing cardiac surgery due to unique risks in this population. For catheter-based intracardiac procedures, the 2010 guidelines state TEE may be used. Separate guidelines focus specifically on the role of echocardiography in interventional and catheter-based procedures. In noncardiac surgery, TEE is indicated in the setting of persistent unexplained life-threatening circulatory instability. If the surgical procedure or the patient’s known or suspected pathology could result in severe hemodynamic, pulmonary, or neurologic compromise, TEE may be used. TEE is recommended in critical care if the diagnostic information is expected to alter management and cannot be obtained by other modalities expediently. European guidelines offer similar recommendations for the use of perioperative TEE, while the American Heart Association (AHA) and American College of Cardiology (ACC) make more limited recommendations regarding specific indications for intraoperative TEE.
In addition to describing indications for perioperative TEE, the 1996 ASA/SCA guidelines also distinguish between basic and advanced levels of training. In 2002, an American Society of Echocardiography (ASE)/SCA Joint Task Force authored guidelines for training in perioperative echocardiography, defined as TEE, epicardial echocardiography, or epiaortic ultrasonography performed in surgical patients immediately before, during, or after surgery. These guidelines do not include TTE. Expectations for cognitive and technical skills of both basic and advanced training are outlined with recommendations for the minimum numbers of echocardiographic examinations performed. Further discussion of training and certification occurs at the end of the chapter.
Critical care societies have further defined competencies and applications of echocardiography in critical care beyond that established by the ASA/SCA guidelines. Several internationally based expert panels have proposed training objectives and competency-based training standards in consensus statements. Similar to the distinction between basic and advanced training in perioperative echocardiography, these statements distinguish between basic and advanced critical care echocardiography, or a basic and expert skill set. The Society of Critical Care Medicine has provided evidence-based recommendations for the use of bedside echocardiography (TEE and TTE) in the evaluation of the critically ill patient.
TEE is a safe and relatively minimally invasive procedure, although echocardiographers should be aware of potential complications resulting from probe insertion and manipulation. Table 37.3 lists absolute and relative contraindications to TEE. The risks and benefits must be carefully considered in patients with oral, esophageal, or gastric disease. Hilberath and associates provide an excellent summary on the safety of TEE, with reviewed studies reporting an overall complication rate in adults of 0.18% to 2.8% and major complication rate of 0.2% to 1.2%. A 2017 retrospective study reviewed recent data regarding complications in a contemporary cardiac surgery cohort. Of the 7948 patients that underwent TEE, 111 (1.4%) were identified as having complications likely attributable to TEE (no other cause identified). Incidence of significant dysphagia was 0.3% and esophageal or gastric complications 0.9%. Independent risk factors associated with complications were age, body mass index, previous stroke, procedure other than isolated coronary artery bypass grafting (CABG), cardiopulmonary bypass time, and return to the operating room for any reason.
| Absolute Contraindications | Relative Contraindications |
|---|---|
Esophageal pathology
|
History of:
|
| Active upper gastrointestinal bleeding | Recent upper gastrointestinal bleeding |
| History of esophagectomy | Active peptic ulcer disease, esophagitis |
| Perforated viscus | Esophageal varices |
| Barrett’s esophagus | |
| Symptomatic hiatal hernia | |
Restricted cervical spine mobility
|
|
| Coagulopathy or thrombocytopenia |
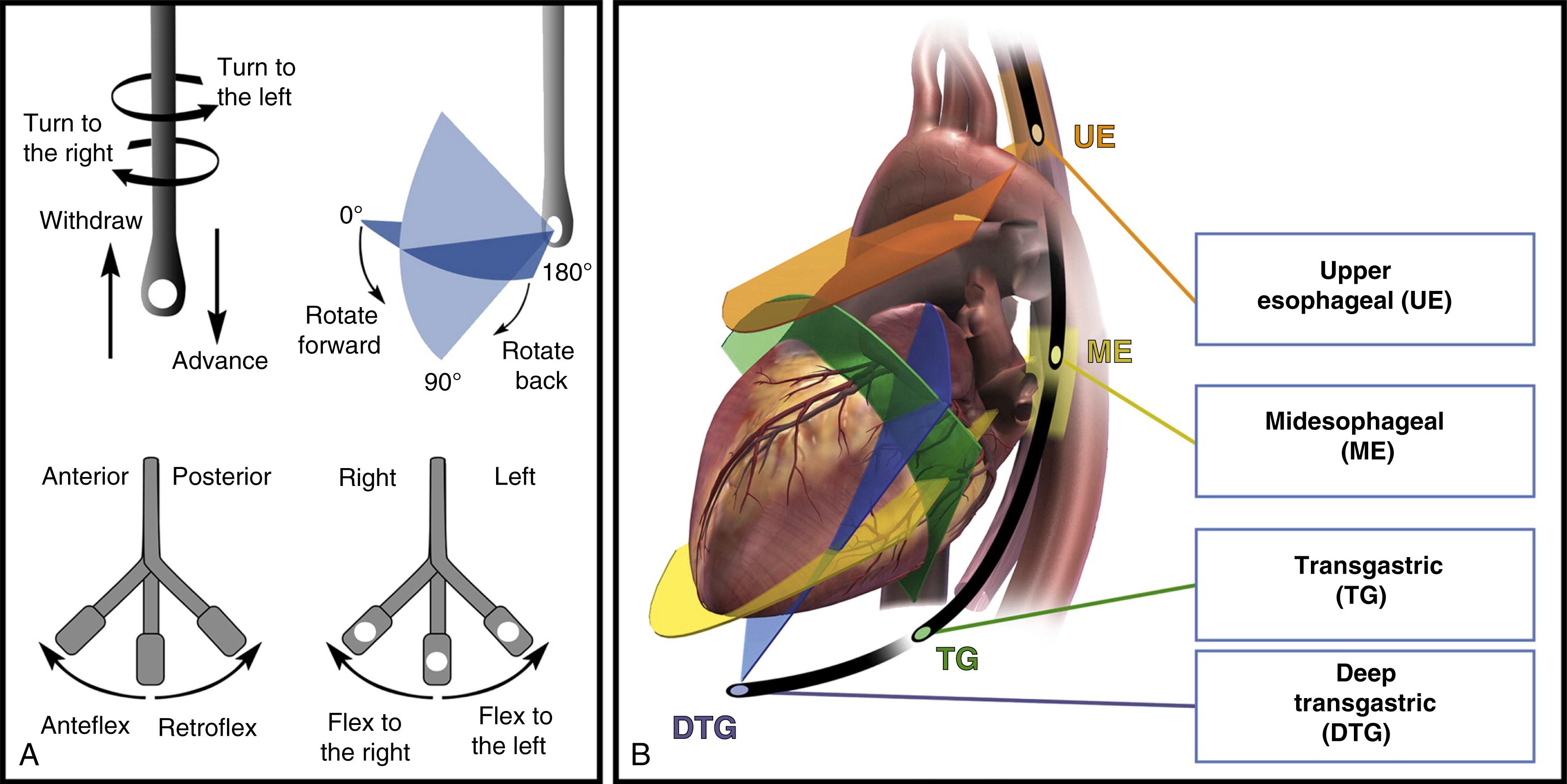
TEE probe manipulation includes withdrawal/advancement, turning left/right, and angle adjustment. The large knob on the handle controls anteflexion/retroflexion and the smaller knob allows flexion to the left and right. TEE image acquisition occurs at four different levels: upper esophageal (UE), midesophageal (ME), transgastric (TG), and deep transgastric (DTG) ( Fig. 37.5 ).
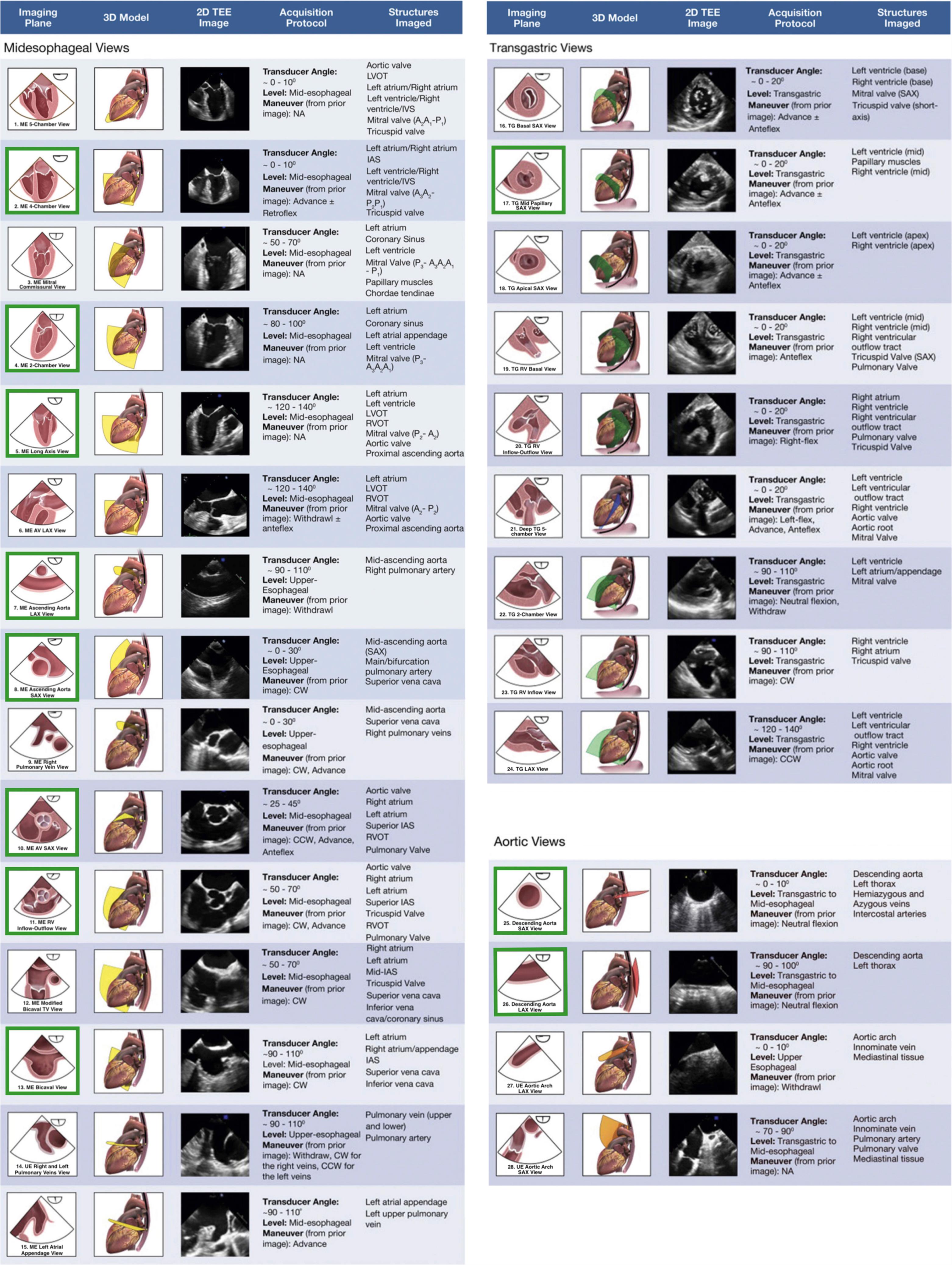
The basic perioperative TEE examination serves as an intraoperative monitoring tool used to identify cardiac causes of hemodynamic or respiratory instability. The basic perioperative examination includes 11 views suited to evaluating hemodynamic instability. A suggested examination sequence progresses through the 11 views as follows: ME four-chamber (ME 4C), ME two-chamber (ME 2C), ME long axis (ME LAX), ME ascending aorta long-axis, ME ascending aorta short-axis, ME aortic valve short-axis (ME AV SAX), ME right ventricular inflow-outflow (ME RV Inflow-Outflow), ME bicaval, TG midpapillary short-axis (TG SAX), descending aorta short-axis, and descending aorta long-axis.
A comprehensive TEE examination enables practitioners with appropriate training to fully utilize the diagnostic capabilities of TEE. Twenty-eight views (including the 11 basic views) are recommended for comprehensive assessment ( Fig. 37.6 ). Technical aspects of image acquisition have been extensively reviewed elsewhere. Echocardiographers should complete their examinations systematically to avoid missing key findings. As a result of individual patient anatomy and the time constraints of the intraoperative environment, not all views are obtained in every examination.
While epicardial echocardiography ushered in the era of intraoperative echocardiography, its use was supplanted by TEE. In the setting of contraindications to TEE or the need for better visualization of anterior structures, epicardial echocardiography remains an alternative modality.
Epiaortic ultrasound (EAU) serves as an imaging adjunct, allowing visualization of the ascending aorta and aortic arch, regions that are unable to be visualized on TEE. Detection of ascending aorta atheroma is superior with EAU compared to that of TEE or manual palpation. EAU impacts surgical strategy, but data as to whether this translates into improved clinical outcomes are limited and heterogeneous. Examination guidelines and example imaging views are available.
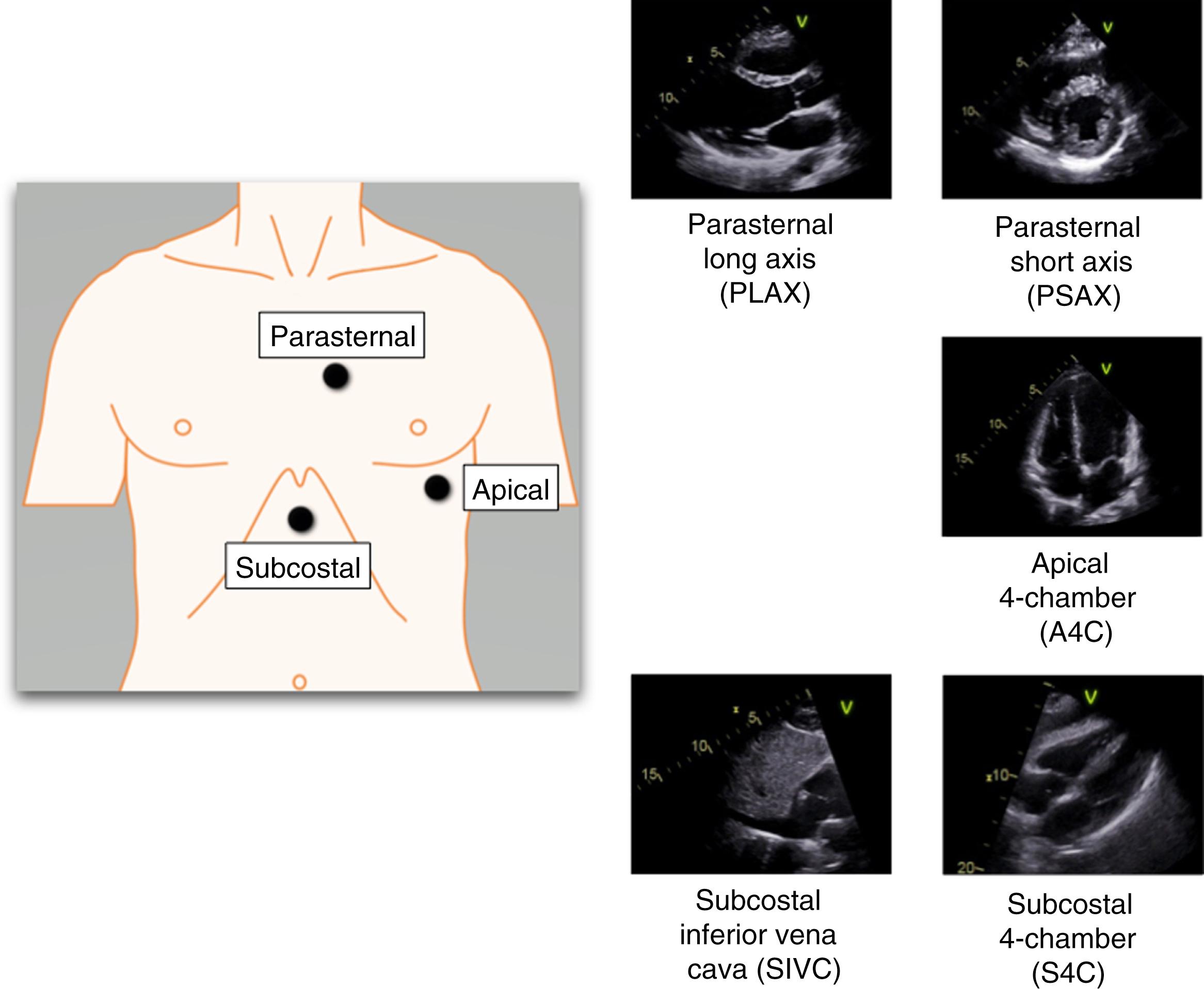
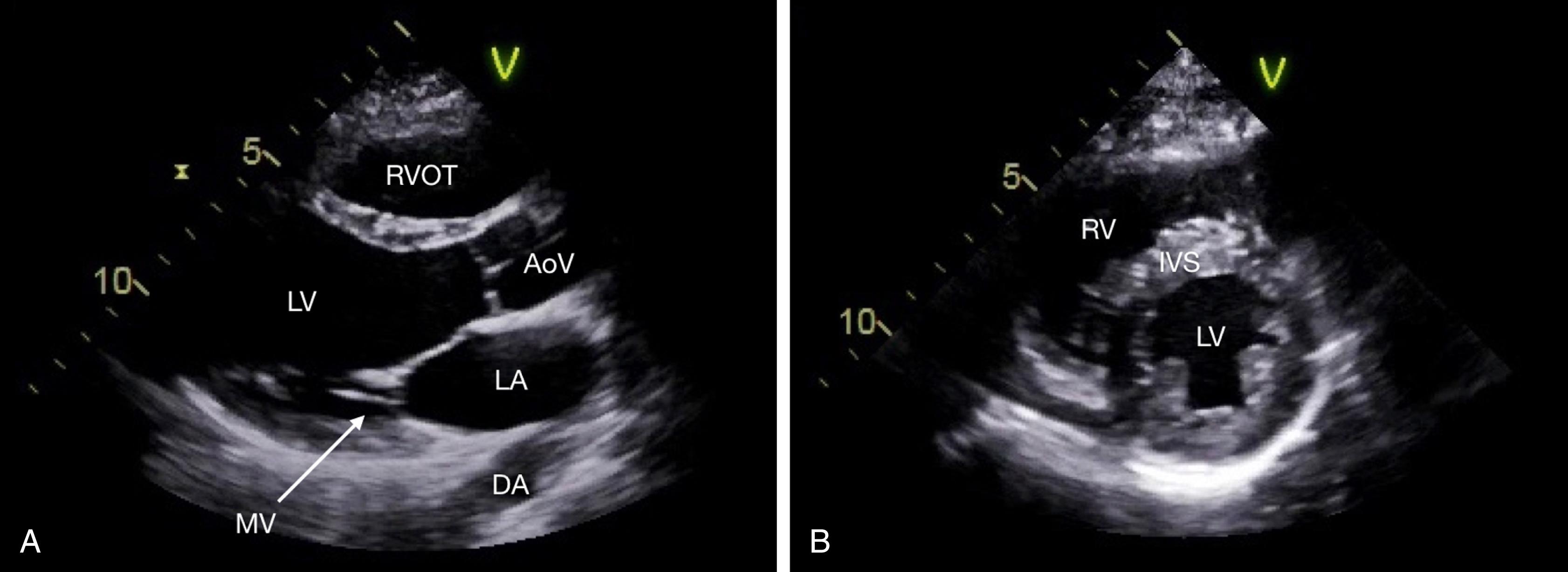
Three elements describe transthoracic sonographic views: (1) transducer position or window, (2) imaging plane, and (3) structures imaged. When feasible, patients should turn to their left side with the left hand resting behind the head. The main windows are parasternal, apical, subcostal, and suprasternal. Imaging motions include translation (sliding), tilting, angulation, and rotation.
With increasing use of ultrasonography at the point of care, it is important for the clinician to recognize the distinction between focused cardiac ultrasound (FoCUS, FCU) and limited TTE examination. Guidelines endorsed by several societies describe the key differences between the two examinations. FoCUS is a simplified, point-of-care ultrasound examination that complements the physical examination ( Box 37.2 ). FoCUS addresses specific questions within a given clinical context. Relevant abnormalities are characterized as present or absent, and questions are answered in a yes/no format. In contrast, limited TTE is broad in scope. Interpretation includes normal, pathological, and incidental findings, and quantitative techniques may be employed. Fewer images are acquired in a limited examination compared to a comprehensive examination. Limited TTE requires a practitioner with advanced training and expertise.
Goal-directed
Problem-oriented
Limited in scope
Simplified
Time sensitive and repeatable
Qualitative or semiquantitative
Performed at the point of care
Usually performed by clinicians
FoCUS, Focused Cardiac Ultrasound.
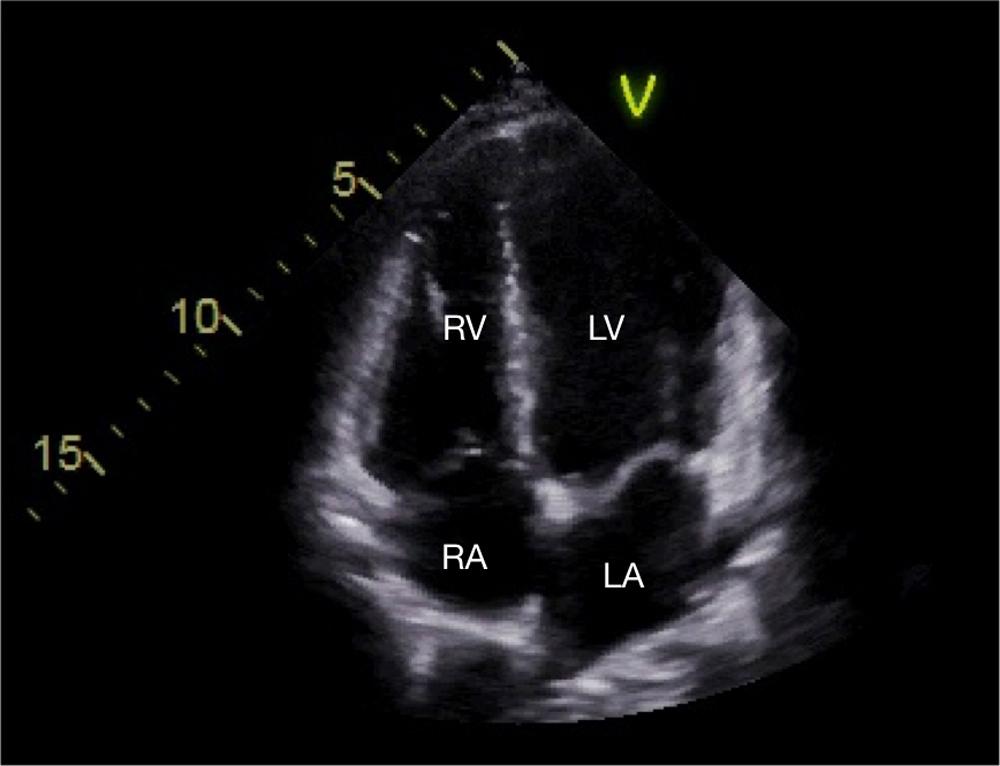
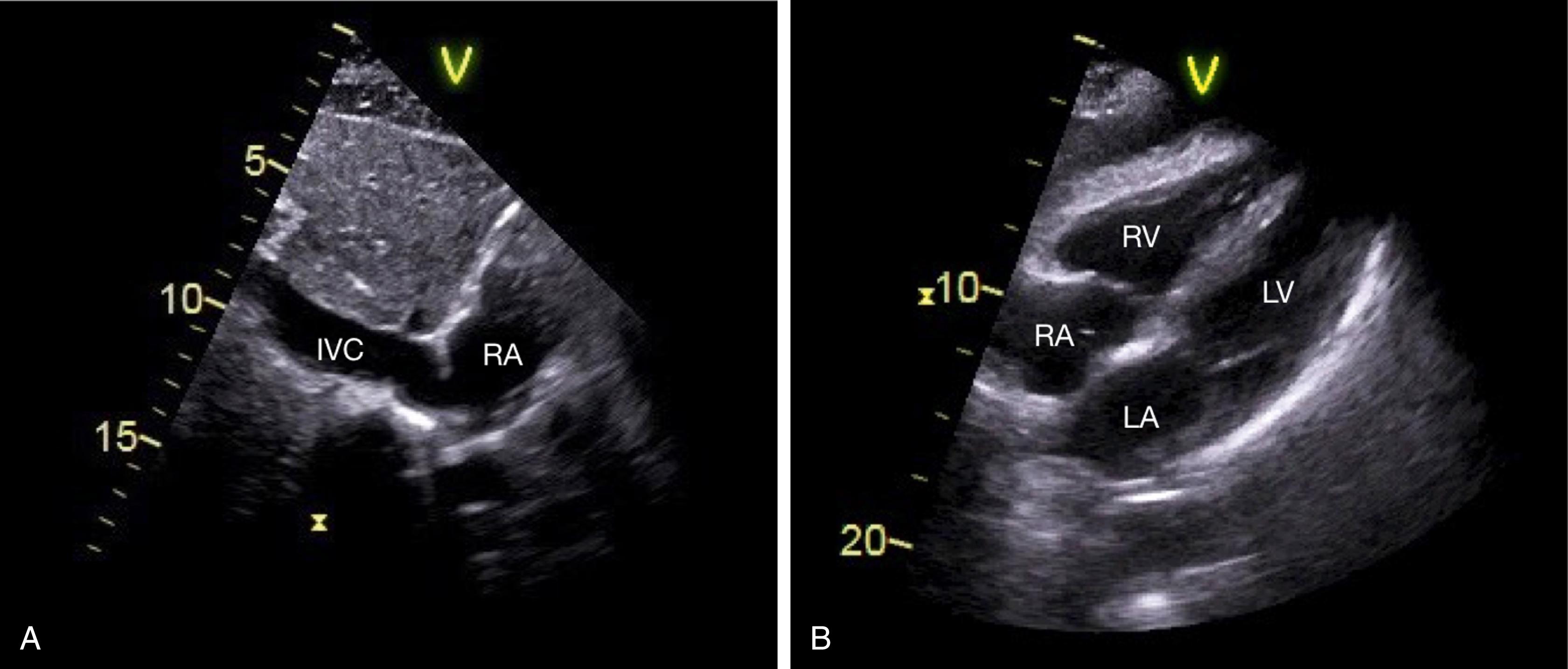
Abnormalities identified by FoCUS require follow-up with formal comprehensive echocardiography. If FoCUS does not reveal pathology but there is clinical suggestion of cardiac disease, formal comprehensive echocardiography should also be pursued. Many FoCUS protocols exist, most including five key views: parasternal long-axis (PLAX), parasternal short-axis (PSAX), apical four-chamber (A4C), subcostal four-chamber (SC4), and subcostal inferior vena cava (SIVC) ( Fig. 37.7 through 37.10 ; Video 37.2). Protocols often incorporate lung ultrasound. For those interested in details of image acquisition, we refer the reader to a practical introductory primer.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here