Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
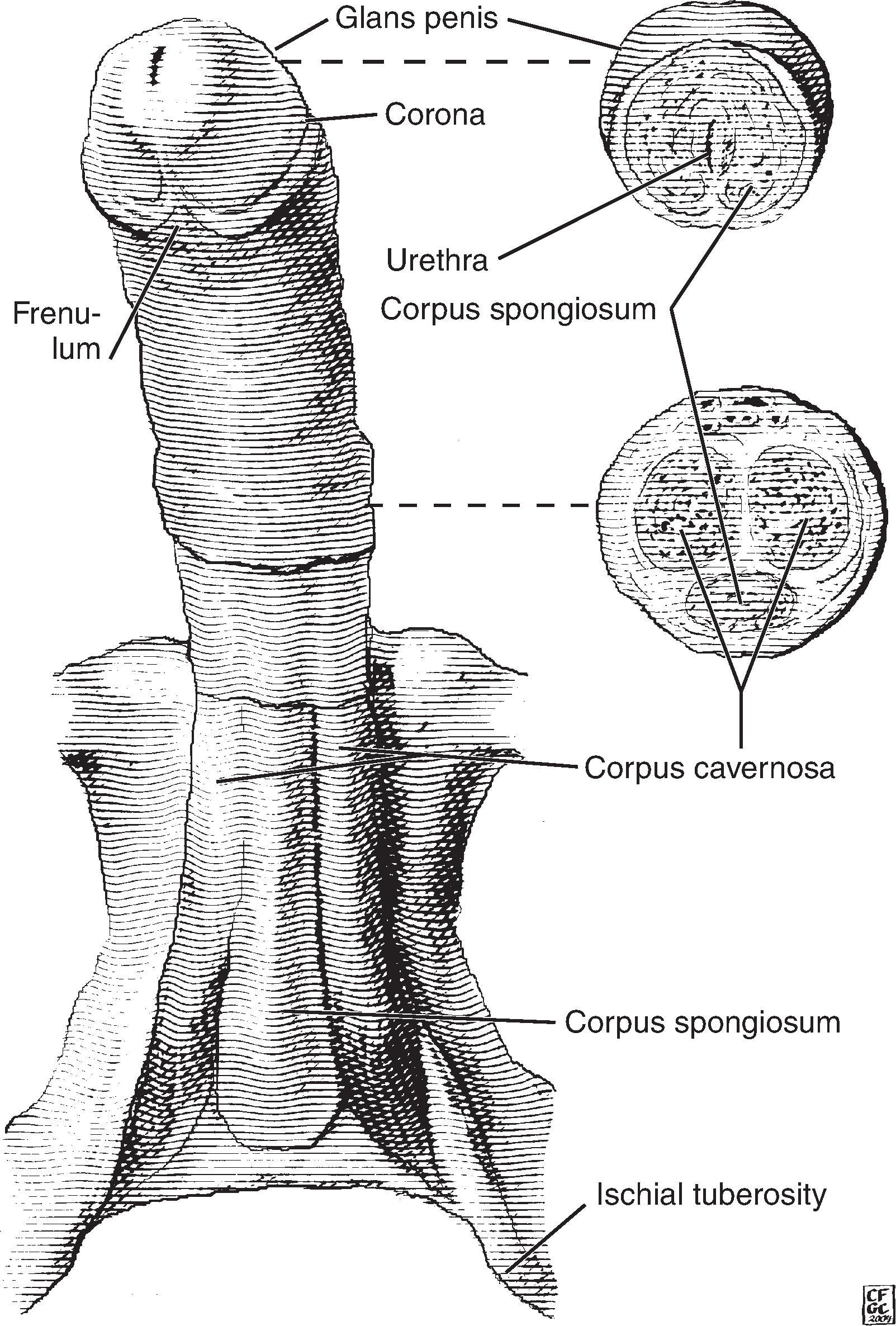
The majority of penile carcinomas are squamous cell carcinomas arising in the glans (~50%), foreskin/prepuce (~20%; mucosal surface more commonly involved than outer surface), coronal sulcus (~5%), or, rarely, in other sites ( Fig. 27.1 ). About one-third are associated with Human Papilloma Virus (HPV) with type 16 followed by type 18 being most common.
Amputations of the penis are almost always for the resection of an invasive squamous cell carcinoma or a urothelial carcinoma. Rarely, the penis is resected for a sarcoma or for paliative reasons. During gender-affirming surgery for transwomen, portions of the penis are used for reconstruction. The remainder of the tissue is generally not sent for pathologic evaluation due to the low likelihood of clinically significant lesions.
Record the dimensions of the total specimen (length, circumference) and foreskin (length, width, thickness).
The type of foreskin (prepuce) has been defined as follows.
Short: The preputial orifice is located behind the glans corona.
Medium: The preputial orifice is between the corona and the meatal orifice.
Long: The entire glans is covered and the meatal orifice cannot be seen unless the foreskin is retracted.
A phimotic foreskin is long and cannot be retracted. This condition is commonly related to inflammatory conditions, infections, and trauma. This type of foreskin is found in about half of patients with carcinoma of the penis.
Tumors usually arise in the glans, foreskin (mucosal surface more common than cutaneous surface), or coronal sulcus. Describe the location of the tumor and all of the structures involved by tumor.
Describe the lesion including size, color, growth pattern (fungating, papillary, polypoid, verrucous, ulcerated), consistency (friable, soft, rubbery, hard), contour (well-defined, infiltrating, pushing margins), and distance from the proximal resection margin. Record the presence of hemorrhage or necrosis.
Describe any skin lesions not related to the tumor.
Ink the margin. The proximal margin can be taken en face if grossly uninvolved by tumor. This allows all anatomical structures to be evaluated. The urethra may retract and require a deeper section in order to include the margin.
If the tumor is close to the margin (e.g <1 cm away), perpendicular sections at the closest approach are more informative.
Open the urethra along the ventral aspect where it is closest to the surface. Do not place a probe into the urethra, as this can disrupt the urothelium and areas of tumor involvement. Extend this cut deeper to bisect the penis into left and right halves. Record the depth of invasion and involvement of foreskin, frenulum, glans, meatus, corpora cavernosa, urethra, and corpus spongiosum.
Fix the specimen overnight in formalin.
Microscopic sections are taken the following day. Additional serial sections are taken of each half. The central portion of the tumor can be used to determine the best axis for sectioning. It is important to take sections perpendicular to the skin surface to accurately evaluate the depth of invasion and the structures involved, as these are important prognostic factors.
The foreskin should be completely submitted in consective sections.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here