Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acute pelvic pain of sudden onset can be caused by both gynecologic and nongynecologic disorders. Adnexal accidents such as rupture or torsion of ovarian cysts, pelvic infections, tubal rupture of ectopic pregnancies, and aborting intrauterine pregnancies are the more common gynecologic causes. Gastrointestinal conditions, such as appendicitis and bowel obstruction, and genitourinary problems, such as cystitis and ureteral stones are the significant nongynecologic causes. Early diagnosis and expeditious treatment, often surgical, are important for safe and effective clinical management of acute pelvic pain.
The most common type of cyclic pelvic pain is recurrent painful menstruation or dysmenorrhea. Dysmenorrhea may be primary, when caused by excessive production of prostaglandins (PGs), mainly PGF 2α , or secondary, when an underlying condition for the pain such as adenomyosis or endometriosis is diagnosed. Primary dysmenorrhea occurs in ovulatory cycles and in younger women (17 to 22 years). Other causes of secondary menstrual and perimenstrual recurrent pain include chronic pelvic infection, degenerating fibroids, and pelvic congestion. Secondary dysmenorrhea is not limited to pain only during menses and typically occurs in older women (>30 years of age).
Treatment of primary dysmenorrhea involves provision of an explanation for the cause of the pain, and reassurance, along with nonsteroidal antiinflammatory drugs (NSAIDs), hormonal contraceptives to block ovulation, and other nonpharmaceutical interventions such as transcutaneous nerve stimulation and acupuncture. Treatment of secondary dysmenorrhea depends on the underlying cause of the pain, with NSAIDs the preferred initial choice.
Chronic pelvic pain (CPP) is noncyclic pain that lasts for more than 6 months. Like other forms of pelvic pain, CPP has both gynecologic and nongynecologic causes. Chronic pain, including CPP, differs from acute pain in several important and measurable ways. With acute pain, the pain perception, suffering, and behavior are usually commensurate with the degree of sensory input. With chronic pain, such as CPP, the suffering and behavioral responses may be quite exaggerated, and may persist even after the pain stimulus has remitted.
The appropriate evaluation and treatment of CPP is challenging. The most effective treatment occurs when a multidisciplinary team manages the patient with ongoing, as opposed to episodic care. Psychiatric referral for psychopharmacologic therapy may be needed. This aspect of therapy is crucial, because many of these patients may be severely depressed and they may be withdrawn interpersonally, sexually, and occupationally.
Pelvic pain is a frequent complaint in gynecology. It may be acute, cyclic, and associated with menstruation, or chronic, lasting for more than 6 months. Acute pelvic pain is sudden in onset and is usually associated with significant neuroautonomic reflexes such as nausea and vomiting, diaphoresis, and apprehension. There are several important gynecologic and nongynecologic causes of acute pain.
Half of all menstruating women are affected by painful menstruation or dysmenorrhea making it the most common type of pelvic pain. Ten percent of these women have severe symptoms necessitating time off from work or school. Chronic pelvic pain (CPP) includes reproductive and nonreproductive organ–related pelvic pain that is primarily acyclic and that lasts for 6 months or more.
It is important for the gynecologist to be aware of both the gynecologic and nongynecologic causes of acute pelvic pain ( Box 21-1 ). Delayed diagnosis and treatment of acute pelvic pain may increase the morbidity and even the mortality.
Adnexal accidents, e.g., ovarian cyst torsion, rupture, or hemorrhage
Acute infections, e.g., endometritis or pelvic inflammatory disease
Pregnancy complications, e.g., ectopic gestation or abortion
Gastrointestinal, e.g., appendicitis, enteritis, or intestinal obstruction
Genitourinary, e.g., cystitis, ureteral stones, or urethral syndrome
Other, e.g., pelvic thrombophlebitis, vascular aneurysm, or porphyria
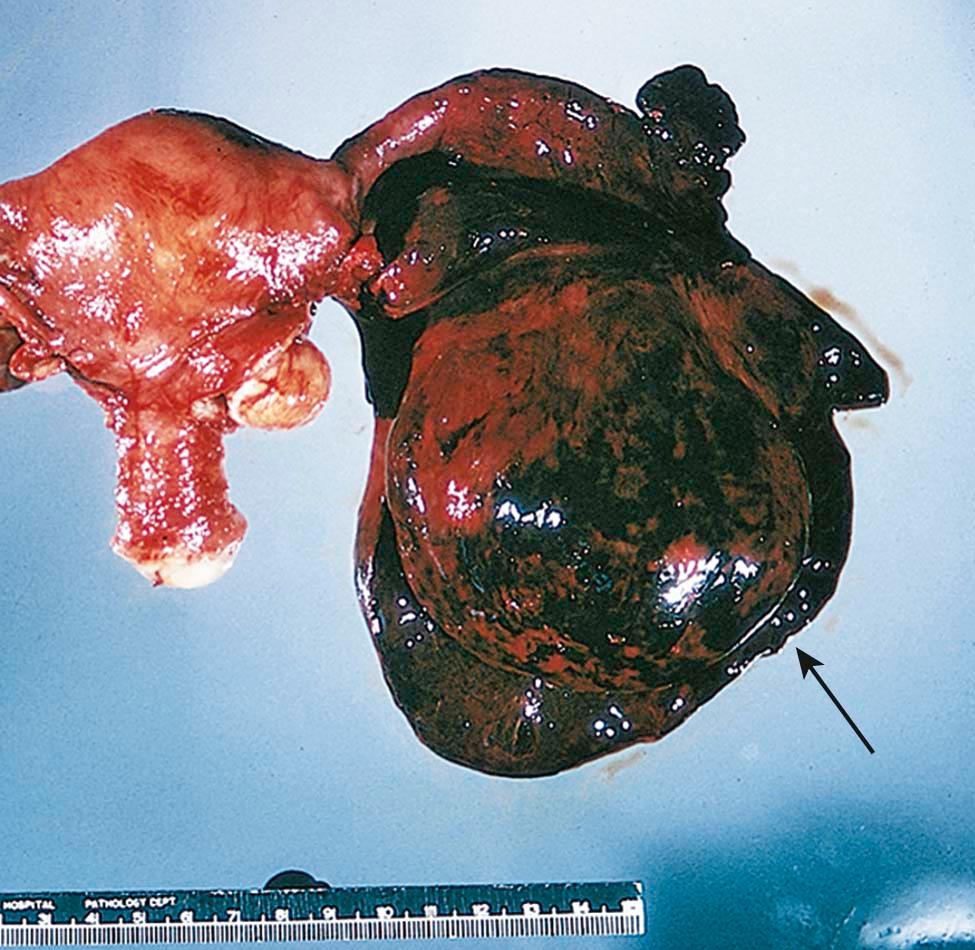
Adnexal accidents, including torsion or rupture of an ovarian or fallopian tube cyst ( Figure 21-1 ), can cause severe lower abdominal pain. Normal ovaries and fallopian tubes rarely undergo torsion, but cystic or inflammatory enlargement predisposes to these adnexal accidents. The pain of adnexal torsion can be intermittent or constant, is often associated with nausea, and has been described as reverse renal colic because it originates in the pelvis and radiates to the loin. An enlarging pelvic mass is found on examination and ultrasound, with decreased or absent blood flow to the adnexa on Doppler-ultrasonic studies. The need for surgical intervention is common and urgent.
Functional ovarian cysts (e.g., corpus luteal or follicular cysts) may rupture causing leakage of fluid or blood that causes acute pain from peritoneal irritation. When there is significant associated bleeding, the pain may be followed by a hemoperitoneum and hypovolemia. Surgical intervention is mandatory in this setting, after adequate resuscitation with packed red cells and intravenous fluids.
Reproductive organ infections such as endometritis or salpingo-oophoritis (commonly referred to as pelvic inflammatory disease or PID) can present acutely. Rupture of a tubo-ovarian abscess is a surgical emergency that can progress to hypotension and oliguria after initially presenting with diffuse lower abdominal pain. Pelvic infection is covered in greater detail in Chapter 22 .
Several complications of early pregnancy, such as ectopic gestation (see Chapter 24 ) and threatened or incomplete abortion, can cause acute pelvic pain and are generally associated with abnormal bleeding. Ectopic tubal pregnancies produce pain as the fallopian tube dilates and ruptures into the abdominal cavity, and can be life-threatening when not diagnosed expeditiously.
Nongynecologic causes of acute lower abdominal pain (see Box 21-1 ) are frequently in the differential diagnosis when a woman presents with pelvic pain. Appendicitis is a common gastrointestinal cause of acute lower abdominal pain that eventually localizes to the right lower quadrant of the abdomen (McBurney point). The unilateral intensity of the pain usually differentiates it from salpingo-oophoritis. Rupture of an infected appendix into the pelvic cavity can have a significant adverse effect on female fertility and may be a diagnostic challenge during pregnancy (see Chapter 16 ). Diverticular abscess is also not uncommon but usually occurs in postmenopausal women.
Acute cystitis (see Chapter 22 ) and ureteral stone formation (lithiasis) and passage are both frequently painful. Urethral syndrome can present acutely and become chronic over time when not recognized and treated. Painful pelvic floor disorders are covered in more detail in Chapter 23 .
Dysmenorrhea is painful menstruation with absence of pain, generally, between menstrual periods. It may be primary when there is no readily identifiable cause, or secondary to organic pelvic disease. The typical age range of occurrence for primary dysmenorrhea is between 17 and 22 years, whereas secondary dysmenorrhea is more common in older women (>30 years of age).
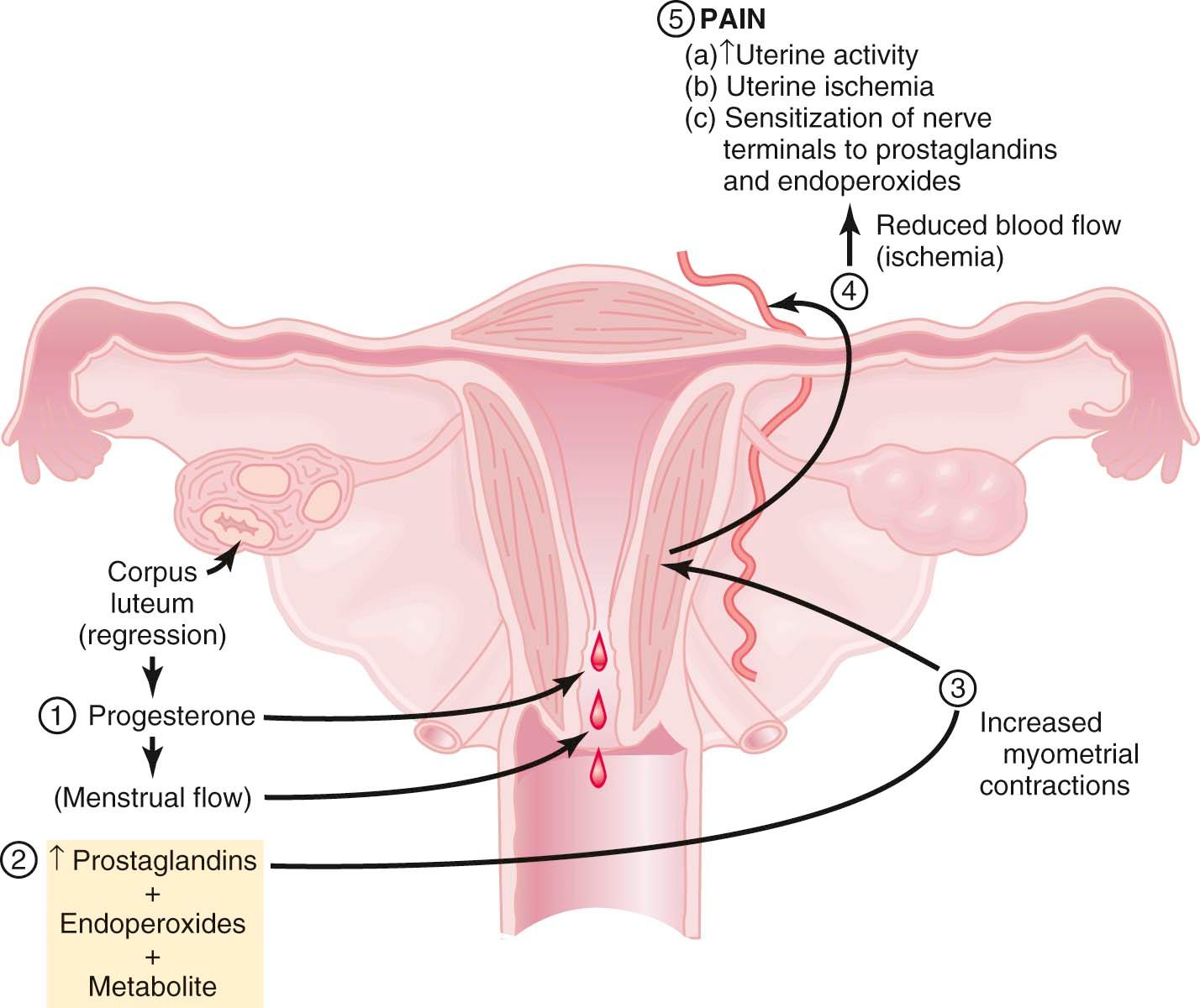
Primary dysmenorrhea occurs during ovulatory cycles and usually appears within 6 to 12 months of the menarche. The etiology of primary dysmenorrhea has been attributed to uterine contractions with ischemia and production of prostaglandins. Women with dysmenorrhea have increased uterine activity, which results in increased resting tone, increased contractility, and increased frequency of contractions. During menstruation, prostaglandins are released as a consequence of endometrial cell lysis, with instability of lysosomes and release of enzymes which break down cell membranes.
The evidence that prostaglandins are involved in primary dysmenorrhea is convincing. Menstrual fluid from women with this disorder has higher than normal levels of prostaglandins (especially PGF 2α and PGE 2 ), and these levels can be reduced to below normal with nonsteroidal antiinflammatory drugs (NSAIDs), which are effective treatments. Infusions of PGF 2α or PGE 2 reproduce the discomfort and many of the associated symptoms such as nausea, vomiting, and headache. Secretory endometrium contains much more prostaglandin than proliferative endometrium. Women with primary dysmenorrhea have upregulated cyclooxygenase (COX) enzyme activity as a major cause of their pain. Anovulatory endometrium (without progesterone) contains little prostaglandin, and these menses are usually painless. The thin endometrium in women using hormonal contraceptives also exhibits decreased prostaglandin synthesis.
Figure 21-2 summarizes the relationships among endometrial cell wall breakdown, prostaglandin synthesis, uterine contractions, ischemia, and pain.
The clinical features of primary dysmenorrhea are summarized in Box 21-2 . Cramping usually begins a few hours before the onset of bleeding and may persist for hours or days. It is localized to the lower abdomen and may radiate to the thighs and lower back. The pain may be associated with altered bowel habits, nausea, fatigue, dizziness, and headache.
90% experience symptoms within 2 years of menarche (i.e., when ovulation begins).
Dysmenorrhea begins a few hours before or just after the onset of menstruation and usually lasts 48-72 hours.
Pain is described as cramp-like and is usually strongest over the lower abdomen, but may radiate to the back or inner thighs.
Nausea and vomiting
Fatigue
Diarrhea
Lower backache
Headache
Normal findings
NSAIDs, which act as COX inhibitors, are highly effective in the treatment of primary dysmenorrhea ( Box 21-3 ). Typical examples include ibuprofen (400 to 600 mg every 6 to 8 hours), naproxen sodium (250 to 500 mg every 8 hours), and mefenamic acid (500 mg every 8 hours). Decreasing prostaglandin production by enzyme inhibition is the basis of all NSAIDs. Pain relief is better if NSAIDs are started 2 to 3 days before menstrual flow. Hormonal contraceptives, such as oral contraceptive pills (OCs), patches, or transvaginal rings, reduce menstrual flow and inhibit ovulation and are also effective therapy for primary dysmenorrhea. Extended cycle use of OCs or the use of long-acting injectable or implantable hormonal contraceptives or progestin-containing intrauterine devices minimizes the number of withdrawal bleeding episodes that users have. Some patients may benefit from using both hormonal contraception and NSAIDs.
Reassurance and explanation
Nonsteroidal antiinflammatory drugs
Hormonal contraceptives (including hormone-releasing intrauterine devices and vaginal rings)
Progestins
Analgesics
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here