Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Access video content for this chapter online at Elsevier eBooks+ ![]()
Burn care is a complex endeavor that requires the coordination of a multidisciplinary team to successfully manage a patient through the phases of resuscitation, critical illness, rehabilitation, reconstruction, and ultimately re-integration into family and society. When a child is burned, there are many additional considerations that will impact how care is delivered, unique to each developmental stage, from infancy to young adulthood. Plastic surgeons occupy a key role on the burn team, and plastic surgery principles are essential to deliver high quality pediatric burn care.
Burns are relatively common, with approximately 486,000 injuries requiring medical treatment per year in the United States alone. From 2009 to 2018, pediatric patients (1 to 16 years) comprised 22.5% of all acute US burn center admissions. For the vast majority of this cohort, the extent of burns were less than 10% total body surface area (TBSA). Scald and contact burns were most prevalent in infants and children, while flame burns were the primary etiology for adolescents and young adults. For patients less than five, minorities were significantly over-represented in this registry data. Overall mortality ranged from 0.2%–0.8% and was closely associated with the %TBSA involved. National data would suggest that pediatric burns are increasingly admitted or transferred to higher volume centers, reflecting the regionalization of burn care.
Globally, there has been a decrease in burn incidence, severity, and mortality; however, data is mostly limited to developed countries. Available data would suggest the greatest burden of burn injury exists in low-income countries. Children are particularly vulnerable to burn injury in low-income countries, with four times greater proportion of deaths compared to high-income countries. Those patients with severe burns that survive will typically have limited or no access to acute surgical care and rehabilitation, resulting in significant post-burn deformities.
A number of epidemiologic studies have explored general risk factors for burn injury in the pediatric population. Various socioeconomic factors have been associated with childhood burns, including poverty, parental employment/education, single-parent households, and poorer living conditions. Demographic factors such as age (≤5 years), male gender, as well as ethnic minorities and immigrant groups are associated with a higher reported incidence of burn injuries in childhood in both developed and developing nations.
The risk and pattern of burn injury changes according to the developmental stage of the child. In the home, the incidence of burns is reported to peak between 15 and 24 months, when exploratory behavior is greatest; motor development, coordination, hyperactivity, and emotional regulation had consistent independent effects on burn injury in a population-based birth cohort. Common scenarios include “pulling down” hot liquids from a higher surface, exposure to or immersion in hot tap water, and exposure to steam or hot liquids from a microwave oven. Other frequently encountered mechanisms include touching hot surfaces such as fireplaces or appliances, contacting electrical outlets, chewing on electrical cables, or playing with matches, candles, and fireworks. Each of these injury patterns occur in the context of specific developmental stages. As a child grows older, their individual characteristics become more influential on the risk of burn injury than environmental factors.
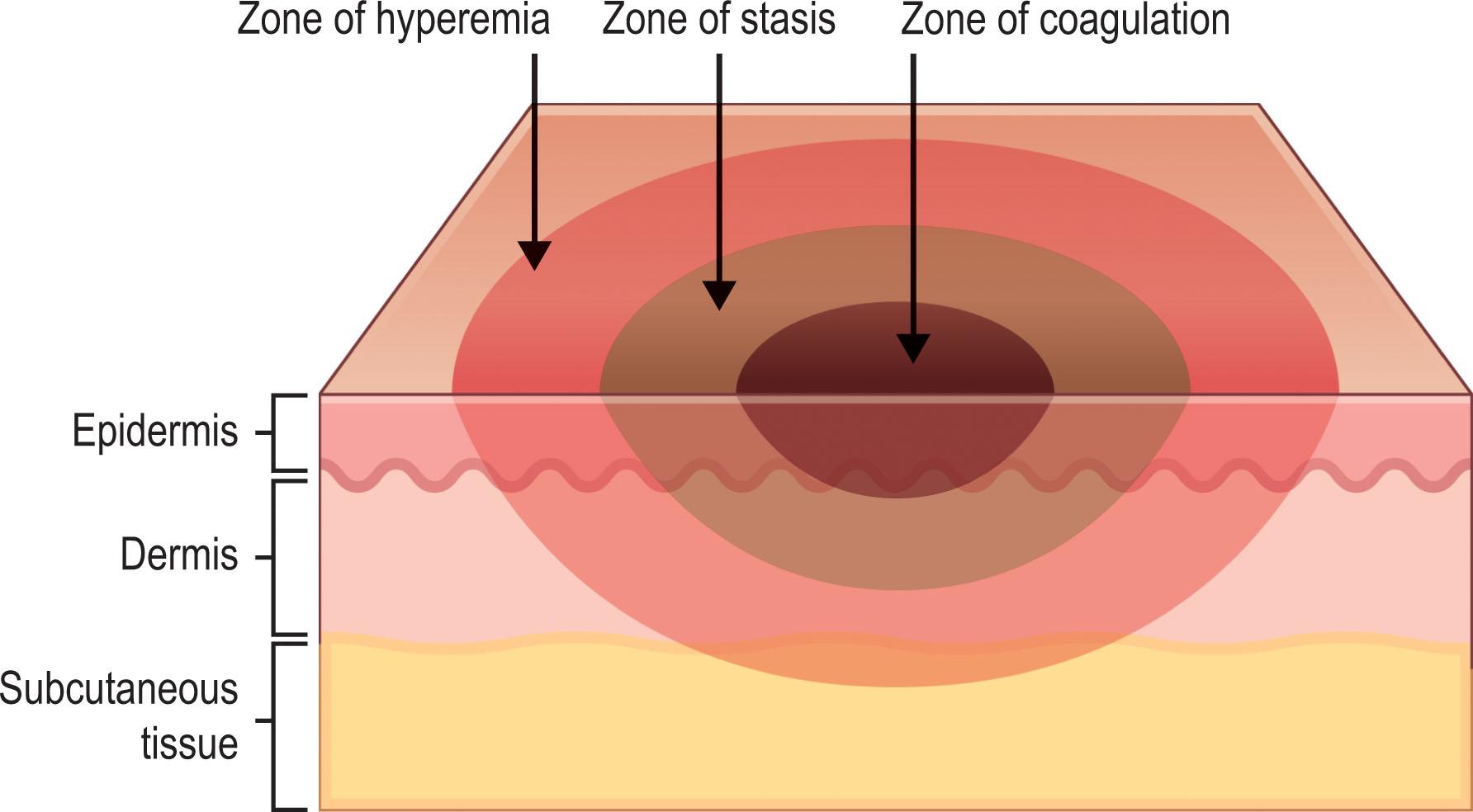
If enough thermal energy is applied to skin, it will lead to protein denaturation and coagulative necrosis. The basic pathophysiology of a burn can be understood as “time versus temperature”, which was demonstrated experimentally to occur as low as 44°C (111°F). Conceptually, the burn wound has a central zone of coagulation, surrounded by the zone of stasis, with an outer zone of hyperemia ( Fig. 21.1 ). In practice, efforts are made to “rescue” this zone of stasis with resuscitation, wound care, and nutrition.
Several unique factors are present in children which will affect burn pathophysiology. Anatomically, the dermis of a child is relatively thin, particularly under the age of five; compared to an adult, equivalent temperatures and duration of exposure are more likely to result in a full-thickness injury. Similarly, an equivalent exposure (i.e., tap water scald) will result in a relatively larger injury in a child due to their small body surface area. The ratio of body surface area to weight is also greater in children, which leads to higher resuscitation volumes. Physiologically, children are thought to have poorer thermoregulation due to their body surface area, in addition to impaired heat generation via shivering in infants with low muscle mass. Developmentally, infants and children may not recognize a dangerous heat source, and subsequently cannot avoid or escape it if left unsupervised. Taken together, these factors may lead to more frequent burn injuries, which are more severe, with more complicated acute care.
Significant progress has been made in the realm of burn prevention, ranging from interventions on an individual/community level, all the way up to regulatory and legislative changes. Burn prevention is particularly relevant in pediatrics given the vulnerability of children and the potential for lifelong sequelae following major childhood burn injuries ( Box 21.1 ). Injury prevention can be classified as primary, secondary, or tertiary. Primary prevention occurs pre-event, such as lowering a water heater to 48.8°C (120°F) to prevent accidental scald injuries. Secondary prevention occurs during the event and minimizes the injury, for example applying cool water to a burn as part of first aid. Tertiary prevention occurs post-event and involves avoiding impairment from the injury, such as appropriate splinting following a deep hand burn. Prevention efforts can be further classified as active (i.e., educational programs) or passive (i.e., legislation and regulation).
Childproof your electrical outlets and appliances
Check to make sure the water temperature is just right (<48.8°C [120°F])
Use the back burner and oven mitts
Engage older kids in cooking
Be careful with the microwave
Install smoke alarms and carbon monoxide alarms
Keep flammable materials away from space heaters
Install barriers around fireplaces, ovens, and furnaces
Blow out candles and store matches out of reach
The initial assessment of a child with a major burn injury requires a systematic approach. In many cases, patients will initially present to a non-burn hospital where a rapid assessment must be performed. Once the child’s condition has stabilized, they may be transferred to a burn center for definitive management. The Advanced Burn Life Support (ABLS) course was developed to provide non-specialists with an approach to safely manage and triage a burn patient in the first 24 hours post-injury.
The assessment begins with a primary survey ( Table 21.1 ) to rule out immediately life-threatening conditions using the ABCDE mnemonic. In general, the presence of a large cutaneous burn can be distracting to the team performing the initial assessment; however, it is essential to exclude the presence of additional injuries and avoid premature diagnostic closure. Assessment of the airway is critical, and children are especially vulnerable to obstruction due to anatomic differences including a relatively narrow diameter and more compressible tissue; in particular, minimal airway edema will disproportionately reduce airflow compared to an adult. If respiratory distress is present, or if there is concern of airway edema, endotracheal intubation should be performed by the most experienced provider. Depending on the clinical scenario, care must be taken to protect the cervical spine.
| Airway maintenance | Maneuvers – chin lift or jaw thrust |
| Oropharyngeal airway | |
| Advanced airway | |
| Protect cervical spine – altered mental status or traumatic mechanism | |
| Breathing and ventilation | Auscultate for bilateral breath sounds |
| Respiratory rate | |
| Oxygen saturation | |
| Supplemental oxygen (100%) if suspicion for carbon monoxide poisoning | |
| Monitor for circumferential chest/neck burns for impaired ventilation | |
| Circulation and cardiac status | Heart rate, blood pressure, skin color |
| Cardiac monitoring | |
| Intravenous catheters (large bore, minimum of two) | |
| Initial fluid rates for visibly large burns (≥20% TBSA) | |
|
|
|
|
|
|
| Monitor circumferential extremity burns for impaired circulation | |
| Disability and neurologic deficit | Level of consciousness |
| Pupillary exam | |
| Exposure and environmental control | Stop the burning process |
| Completely undress the patient, including diapers, shoes, jewelry | |
| Examine for signs of other major injuries | |
| Cover with warm, clean and dry sheet |
Breathing and ventilation follow, assessing for typical signs and symptoms of acute respiratory distress. Thoracic trauma must be excluded, beginning with inspection and auscultation of the chest. Continuous oximetry is placed and supplemental oxygen should be provided as needed; if carbon monoxide poisoning is suspected, 100% oxygen must be administered to accelerate clearance. The presence of deep circumferential neck and trunk burns can mechanically restrict the chest, potentially requiring urgent surgical intervention (discussed later).
Circulation and cardiac status are initially assessed with heart rate, blood pressure, and skin color. Cardiac monitors should be placed, and at minimum two large-bore intravenous catheters are inserted. At this point, the total burn size will be unknown, and a formal fluid resuscitation calculation cannot be performed. In this situation, the ABLS course recommends initial fluid rates for visibly large burns based on patient age (see Table 21.1 ). This approach ensures that fluid resuscitation can begin without delay, while focusing on identifying other potential injuries that are immediately life-threatening. Unexplained hypotension strongly suggests an associated non-burn traumatic injury and a high index of suspicion is required at all times to prevent missed diagnoses. Similar to the chest, deep circumferential extremity burns should be noted along with assessment of distal perfusion.
To complete the primary survey, a baseline neurological assessment should document level of consciousness and a pupillary exam. The presence of altered mental status is not typical following a burn, and should prompt investigations into other structural or metabolic causes. The patient should be fully exposed, which includes removing diapers in infants and young children. Any obvious signs of major injury are noted, and the child is covered with a clean, dry sheet, with additional warm blankets to maintain core temperature.
Once the child is stabilized and immediate life-threatening injuries have been excluded, a secondary survey ( Table 21.2 ) is performed. This first involves a history surrounding the burn injury, namely how, when, and where it happened. Depending on the age of the patient, this may be limited to collateral history from family members, acquaintances, or paramedics. Documenting what first aid was performed, if any, is essential. The mechanism of burn injury must be established along with relevant details. For scald burns – what setting (bath, sink, etc.), what liquid (water, soup, etc.), how much liquid, what temperature (freshly boiled, tepid, etc.), and what clothing was worn. For flame burns – what setting (indoors, outdoors, etc.), was there exposure to smoke, were fuels/accelerants involved, was there a blast/explosion, were any others injured. For contact burns – what object (space heater, iron, etc.), what temperature, and what duration of contact. For electrical burns – what setting (home, industrial, etc.), what voltage, duration of contact, and was there a loss of consciousness. For chemical burns – what setting, what chemical (if known), what duration of contact, was there possible ingestion or eye involvement. The mnemonic AMPLET is recommended, and includes allergies, medications, previous illness, last meal/drink, events/environment, and tetanus/immunization status.
| History of presenting illness | Circumstance of injury including timeline |
| Mechanism of injury (flame, scald, electrical, etc.) | |
| First aid provided | |
| Collateral from parents, emergency medical services, etc. | |
| Medical history (AMPLET) | Allergies |
| Medications | |
| Previous illness | |
| Last meal or drink | |
| Events/environment related to the injury | |
| Tetanus and childhood immunizations | |
| Accurate weight | Will determine amount of fluid required |
| Physical exam | Head and neck |
| Chest | |
| Abdomen | |
| Genitourinary | |
| Musculoskeletal | |
| Neurologic | |
| Vascular | |
| Wound assessment | Burn location(s) |
| Burn size (%TBSA) | |
| Burn depth |
A full head-to-toe exam is performed, structured by organ system. An accurate weight must be obtained to direct medication dosing and calculating a fluid resuscitation. Any injuries not detected on the primary survey should be noted with appropriate lab work and imaging. Concern for child abuse and neglect (discussed later) should be raised depending on a variety of physical findings that may be independent of the burn injury.
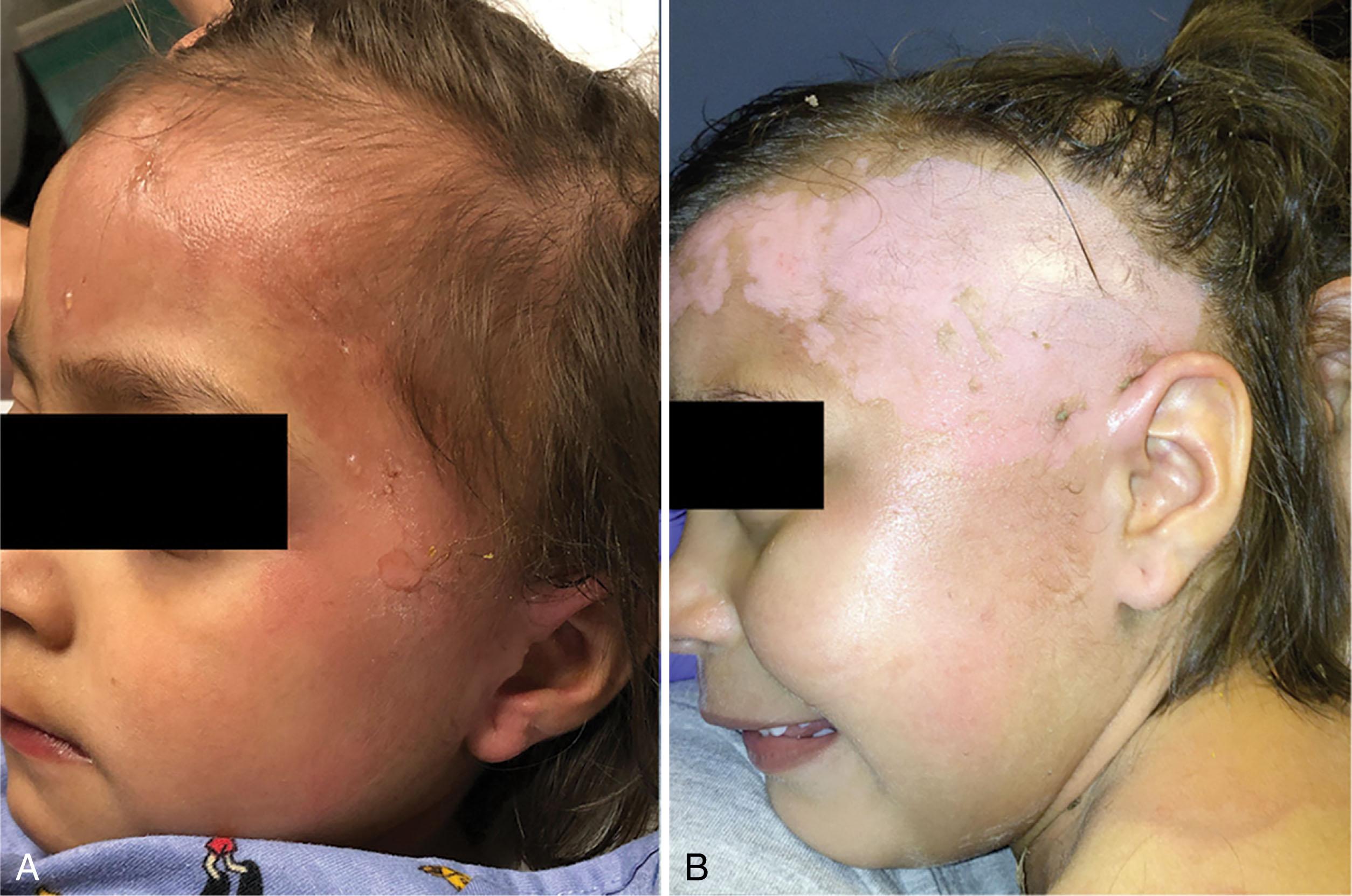
The assessment of the burn wound should accurately document the anatomic structures involved and estimate the total burn size and depth. This will require exposure of the patient, and one should remain vigilant to protect against hypothermia. Additionally, this process has the potential to cause pain and anxiety, so steps should be taken to mitigate any distress using distraction techniques and/or pharmacologic strategies (discussed later). On presentation, partial-thickness and full-thickness burn wounds are often obscured by detached epidermis, undebrided blisters and bullae, hair, soot, and/or other debris. These factors make proper wound assessment challenging and can underestimate the extent of burn injury. Debridement of burn blisters was historically controversial but is now mostly supported by basic and clinical studies. It is our practice in most cases to cleanse the burn wound using warm soapy water to remove devitalized tissue, and if the injury involves the hairline or facial hair expose the underlying skin using clippers ( Fig. 21.2 ).
Beginning with the anatomical distribution of the burn, precise terminology will facilitate better communication with the multidisciplinary team and other consultants (i.e., volar versus dorsal hand). Burns involving specialized structures (face, genitalia, etc.), crossing major joints (elbow crease, dorsal ankle, etc.) and circumferential or near-circumferential extremity wounds may warrant urgent intervention or transfer to a higher level of care.
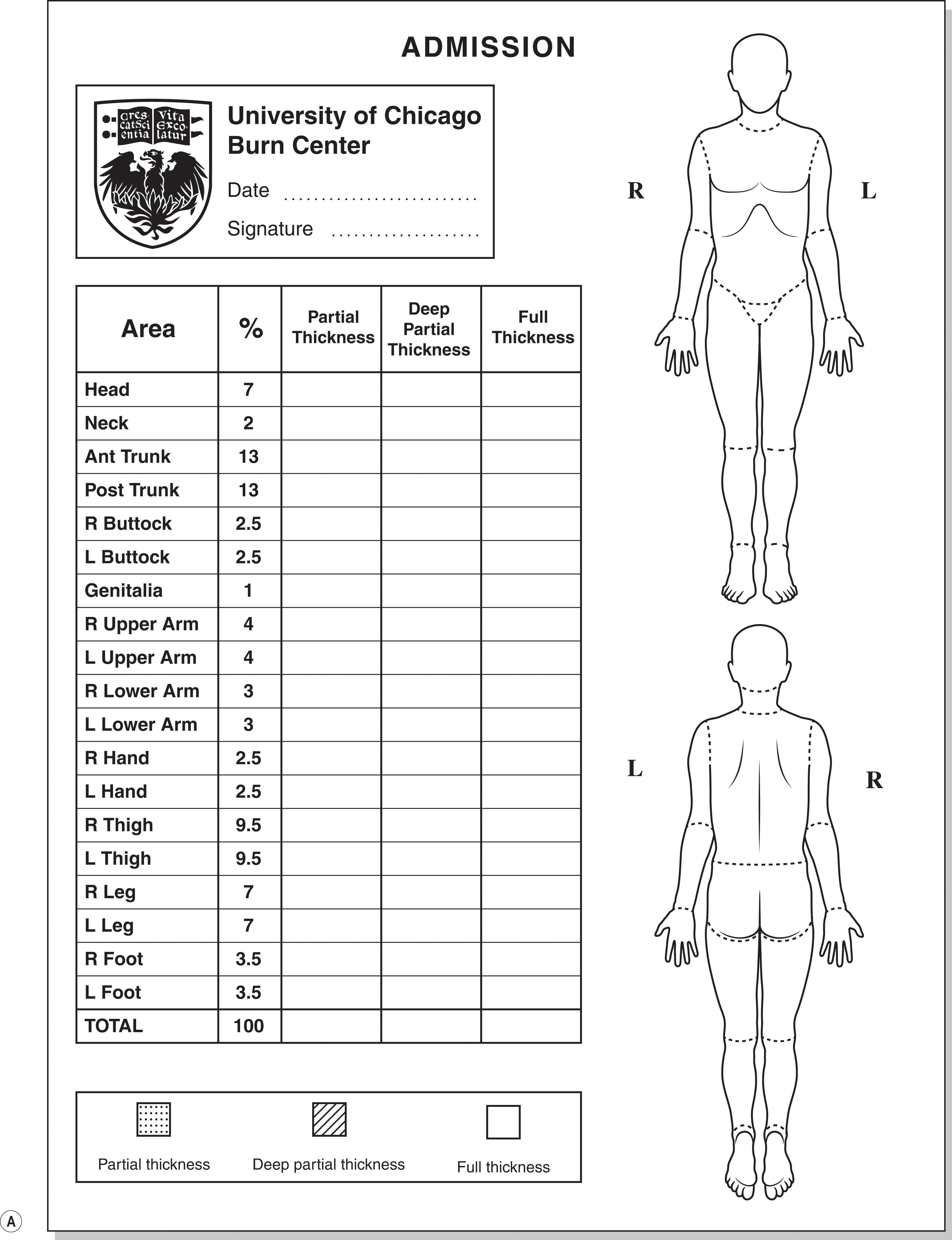
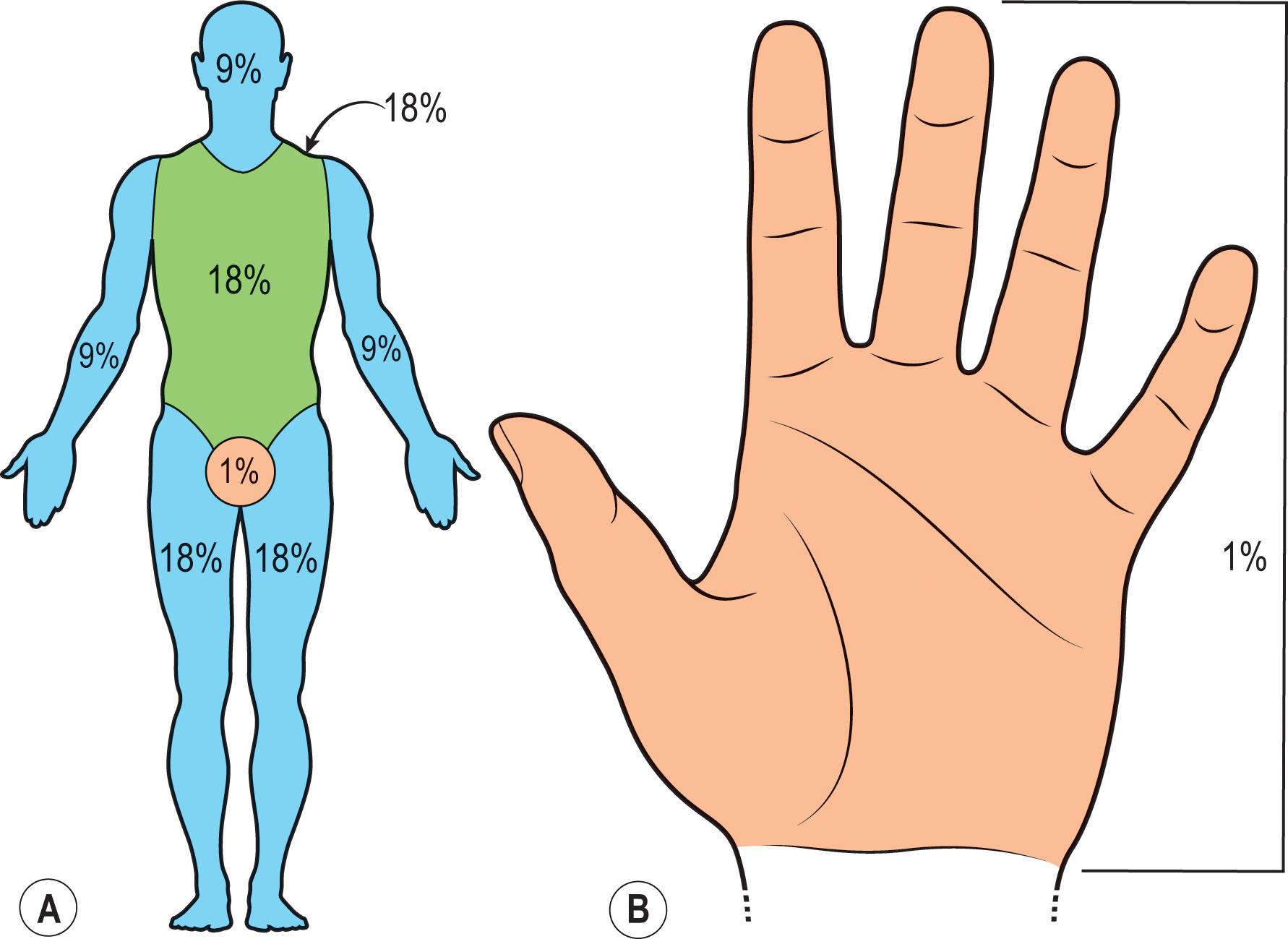
Determination of burn size can be difficult, and providers of all levels may overestimate %TBSA by as much as threefold. Such errors can lead to over-resuscitation and inappropriate triage and transfer. The Lund and Browder diagram remains the gold standard and adjusts for changes in body surface proportions between children and adults ( Fig. 21.3 ). Burn size can be quickly estimated using the “rule of nines” ( Fig. 21.4A ), but this is limited in younger children given differences in body proportions. The “palmar method” ( Fig. 21.4B ) utilizes the area of the patient’s palm from wrist crease to fingertips. This is particularly useful for small burns but can be incorrectly applied if the provider’s palm is used as a reference rather than the patient, or if the fingers are excluded. The obesity epidemic has further complicated the estimation of %TBSA and called into question the reliability of available methods in this population. Emerging technology makes use of three-dimensional photography to more objectively calculate total burn size; however, these tools have not yet gained widespread adoption.
The depth of injury is defined by the skin layer involved and is commonly classified as superficial (first degree), partial thickness (second degree), or full thickness (third degree). A superficial burn involves only the epidermis and is erythematous and painful, but does not desquamate. It is not considered clinically significant and is not included when calculating the %TBSA burned ( Fig. 21.5A ). A partial-thickness burn involves destruction of the epidermis and a portion of the dermis; the skin will blister, swell, weep with variable colors from pink to white depending on the extent of dermal involvement ( Fig. 21.5B ). Accordingly, a superficial partial-thickness burn will heal with minimal scarring, while a deep partial-thickness burn will remain open for longer and may require surgical intervention. Finally, a full-thickness burn involves destruction of the epidermis and entire dermis, which will appear dry, leathery, white, or charred ( Fig. 21.5C ). These burns nearly always require surgical intervention (depending on the size) as they do not have the capacity to heal without significant scarring. Burns beyond the dermis (into fat, fascia, or muscle) is generally classified as fourth degree burns. In practice, assessment of burn depth is challenging, such that even experienced burn surgeons can fail to predict the wound thickness. In some cases, the immediate appearance of the burn is not entirely reflective of what the definitive wound diagnosis will be; this can be attributed to either simple demarcation over time, or wound conversion due to extrinsic factors such as ischemia or inflammation. The burn depth of these wounds should be classified initially as “indeterminate”. In a classic study of toddlers with scald burns, delaying surgery beyond five days resulted in smaller excisions, suggesting a more accurate assessment of depth over time. Technology such as laser Doppler imaging has been shown to accurately predict the healing potential of pediatric burns ; however, despite favorable data it is not routinely used at most centers.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here