Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Epilepsy is a common clinical manifestation of a variety of underlying neuropathologic conditions. Most patients can be adequately managed with pharmacotherapy; approximately 75% of patients diagnosed with epilepsy may be ultimately seizure free on medications alone. However, approximately 5% to 10% of patients will develop pharmacoresistant or medically intractable epilepsy, which may require surgical intervention.
The focus of this chapter is on specific pathologic processes that are associated with medically intractable seizures. The evaluation of these patients is often quite extensive, involving a variety of diagnostic and assessment modalities including a careful history and physical examination, laboratory testing, electroencephalographic (EEG) studies, neuropsychiatric testing, evolving imaging techniques, and surgical methods of monitoring epilepsy utilizing subdural grids and depth electrodes. Entire textbooks are dedicated to the management of epilepsy patients. Those patients who fail multiple attempts at pharmacologic management may be candidates for surgical intervention, which has been highly successful in improving seizure outcomes. The potential causes of medically intractable epilepsy are myriad. Many of the causes, such as specific tumors and vascular malformative lesions, are dealt with elsewhere in this text, with some of the most frequent of the former including prognostically favorable cortical neoplasms in younger patients, such as ganglioglioma, dysembryoplastic neuroepithelial tumor, pleomorphic xanthoastrocytoma, pilocytic astrocytoma, and angiocentric glioma, which some have grouped under the umbrella term “long-term epilepsy associated tumors,” or LEATs. The first two of these glioneuronal tumors are particularly common and may be combined with focal cortical dysplasia (FCD), now considered as the “FCD IIIb” subtype (discussed later in the chapter). This chapter will therefore focus on four general categories of pathology that are regularly encountered in this setting : FCD/malformations of cortical development, hippocampal sclerosis, vascular insults (infarcts), and Rasmussen encephalitis.
Epilepsy-related resections are among some of the more challenging surgical neuropathology specimens to evaluate. A systematic and careful approach to dissecting and evaluating these cases is important in optimizing diagnostic capabilities. Although detailed suggested guidelines, such as those outlined recently by the ILAE group, provide a comprehensive approach that may be followed in larger centers with adequate resources, a few practical points which can be readily adhered to in all laboratories, regardless of resources available, are outlined here.
An attempt should be made to orient the specimen with respect to location—posterior versus anterior, medial versus lateral.
Close inspection of the exterior appearance of the excised tissue should be performed. Abnormalities such as Sturge Weber, gyral abnormalities, certain superficially situated tumors such as dysembryoplastic neuroepithelial tumors, and contusion-related damage related to invasive seizure monitoring may be evident. Weight and size measurements should be taken.
The specimen should be carefully sectioned at approximately 5-mm parallel intervals according to the orientation, ideally in coronal plane along the anterior-posterior axis. The cross sections should be carefully inspected for abnormalities, which should be documented. Look for blurring of the gray-white interface, discoloration, cystic lesions, and abnormal architecture (e.g., nodules of gray matter situated in the white matter where they do not belong). For hippocampal resections, the shiny white surface corresponds to the ventricular surface; sectioning along the short axis will result in coronal sections of the hippocampus.
Tissue can be frozen or processed for research purposes, if appropriate. A careful and thorough sampling of the resected tissue, trying to maintain orientation, should be performed. Sample both areas of grossly apparent abnormalities, as well as adjacent more normal-appearing tissue. Sometimes, tumors, which may be grossly evident, are associated with adjacent FCD, which in fact may be the epileptogenic lesion and may not be grossly evident. Do not be too stingy with tissue sampling (e.g., the ganglion cell component of a ganglioglioma may be only focally present in the tumor and FCD patterns may be variable from region to region).
Since tissue sampled is often larger, more time for fixation and tissue processing may be required prior to sectioning. Paraffin-embedded tissue sections may be cut at a 4- to 5-micron thickness and stained with hematoxylin and eosin.
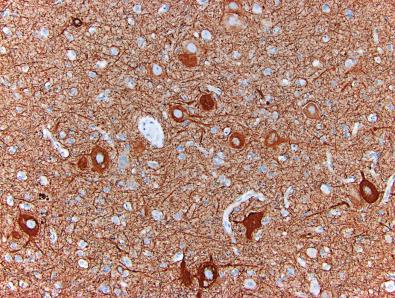
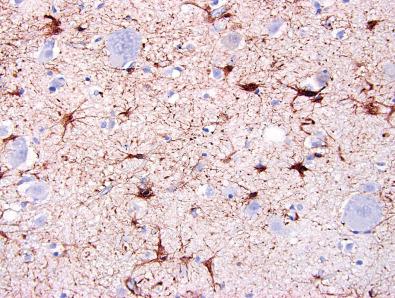
Use of ancillary special stains and/or immunostains will often depend on the abnormalities observed or being evaluated. Routine stains available may vary considerably from laboratory to laboratory. Neural markers such as NeuN, neurofilament protein, and MAP2 can be helpful in delineating subtle forms of FCD. Glial fibrillary acidic protein (GFAP) can be useful in highlighting gliosis. Tumor evaluation may necessitate examining a variety of other markers including IDH-1, ATRX, Ki-67, BRAF, CD34, and p53. Inflammatory lesions, such as Rasmussen encephalitis, may benefit from staining with microglial markers such as CD68 and T lymphocyte markers such as CD3.
FCD represents a phenotypically diverse group of disorders marked by an abnormality of cortical architecture secondary to disrupted or distorted developmental sequences. The most common clinical manifestation of this group of disorders is epilepsy. A variety of synonymous terms have been used in the literature with reference to this group of disorders, including cortical dysplasia, focal dysplasia, neuronal migration abnormalities, cortical malformations, malformations of cortical development, synaptic dysgenesis, cerebral dysplasia, and microdysgenesis.
A number of grossly evident patterns of malformations of cortical development, including entities such as polymicrogyria, agyria, pachygyria, and heterotopias, have long been recognized. In 1971, Taylor and Falconer described 10 epilepsy patients who underwent partial excision of tissue for medically intractable epilepsy. In each case, there was microscopic evidence of cortical disorganization including aggregates of large atypical-appearing neurons. They viewed these changes as an example of a localized or focal form of cortical dysplasia in contrast to the more widespread abnormalities associated with tuberous sclerosis and some of the other grossly evident cortical dysplasia patterns. Detailed descriptions of microscopic abnormalities that were grouped under the heading of cortical dysplasia subsequently emerged. The terminology associated with these pathologies has varied somewhat, depending on the bias of the individual discussing them. Although the cause of most lesions is unknown, what has emerged from the literature is a sense that many of these lesions are the result of altered cortical development due to a variety of potential mechanisms. Although FCD or cortical dysplasia is embedded in the literature, the terminology is, in a sense, a misnomer. Dysplasia typically implies a premalignant condition when used in describing the pathologies in other organ systems; in this setting, it is used to denote a malformation that has no established predisposition to malignancy. It should also be noted that the nomenclature for such lesions is revised periodically, with the most recent consensus of the International League Against Epilepsy (ILAE) having been published in 2011.
The variability of definitions and spectrum of phenotypes recognized by various pathologists in this arena has made determination of the prevalence and demographics of these lesions somewhat difficult to accurately assess. Approximately 15% to 25% of patients referred to epilepsy centers for intractable seizures have FCD. In surgical series where pathology was reviewed, the various forms of FCD comprise approximately 15% of the pathology identified in temporal lobectomy resections for chronic epilepsy, but are much higher, close to 40% in extratemporal lobectomies. The incidence of many of the more severe forms involving abnormal gyral patterns and grossly evident heterotopias is much lower. One source reported an incidence of 0.04 per 1000 for lissencephaly and 0.01 per 1000 for polymicrogyria. The vast majority of patients with these abnormalities present in the first or second decade of life. A subset of patients is diagnosed in adulthood; however, many of these patients have a long history of epilepsy.
The clinical presentation can be quite variable and ranges from cases with extremely debilitating seizures and developmental delay to cases that may be relatively asymptomatic with infrequent seizures. In the more localized forms of FCD, developmental milestones and intellect may be within the normal range or only slightly below average. In more diffuse cases, mental retardation is fairly common. The seizures in most patients with localized FCD exhibit partial rather than generalized seizures. In the series by Raymond and colleagues, seizures originated most commonly in the frontal lobe (47%), followed by the temporal (25%) and parietal lobes (18%).
Children with more severe and diffuse FCD, such as lissencephaly, may have additional findings including apnea, poor feeding, and hypotonia. Symptoms may progress to spastic quadriplegia and opisthotonus.
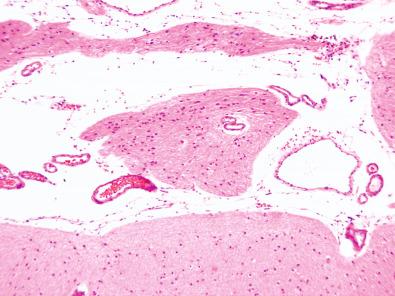
Neuropsychologic evaluations of patients with FCD may reveal intellectual or psychiatric impairments. EEG studies are an important part of the postoperative treatment of these patients and are useful in localizing the seizures. The electrodes and grids used for seizure monitoring are neurosurgically placed and subsequently removed at the time of second surgery; often these are associated with small infarcts, hemorrhages, or contusion-related damage (discussed later in this chapter).
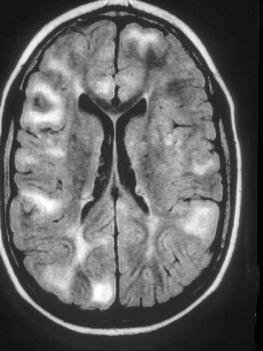
Many of the more severe forms of FCD (including cortical tubers) and those with grossly evident abnormalities are readily evident by imaging studies ( Fig. 25.1 ). More subtle forms with minor architectural disorganization, such as neuronal malalignment, may not be evident on conventional imaging. High-resolution magnetic resonance imaging (MRI), which allows for the reconstruction of very thin contiguous sections through the brain, permits increased identification of some of these lesions. However, there are still limitations to the imaging modalities available. In a study examining the pathology of 95 MRI-negative epilepsy cases, Wang et al. identified FCD on histopathologic examination in 45% of cases. Only seven patients in this series had no identifiable pathologic abnormalities. The lack of findings on MRI is usually considered a predictor for surgical failure. Even in visible lesions there are limitations to the ability to assess abnormalities. High-resolution MRI may identify a region of thickened cortex, but may not always be able to distinguish between pachygyria, polymicrogyria, or more subtle FCD patterns as the cause of the thickening. A combination of approaches, including volumetric T1-, axial T2-, and coronal thin-section T2-weighted images, as well as axial fluid attenuated inversion recovery (FLAIR) images (see Chapter 4 ) can be useful in assessing lesional symmetry, gyral folding patterns, gray-white interfaces, white matter signal abnormalities, and uniformity of cortical signal. Metabolic and functional studies, including positron emission tomography (PET) and single-photon emission computed tomography (SPECT) imaging, can provide complementary information, particularly when conventional studies fail to demonstrate abnormalities.
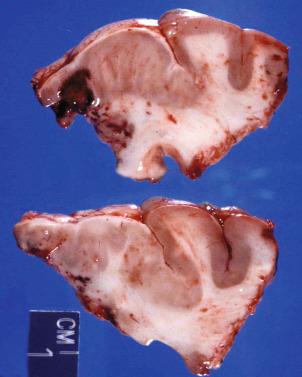
As previously mentioned, the spectrum of FCDs runs the gamut from easily discernible lesions to those that are subtle and only microscopically evident. The gross pathology in fragmented specimens is often best appreciated on the preoperative MR images. Some individuals prefer to separate out the grossly evident pathologies such as lissencephaly, pachygyria, polymicrogyria, and heterotopia from the FCDs as separate malformations. Others view all these lesions as part of the same spectrum. One group of the grossly evident malformations includes disorders of gyral formation. Agyria (lissencephaly) and pachygyria are both marked by the presence of an abnormally thickened cortical ribbon. Agyria refers to a brain with a smooth surface, marked by an absence of gyri, whereas pachygyria is characterized by reduced numbers of broadened gyri. Polymicrogyria or micropolygyria denotes a condition in which the cerebrum is composed of small, irregularly formed gyri separated by shallow sulci ( Fig. 25.2 ). The process may be either localized or more diffuse in distribution, but has a particular predilection for involving the perisylvian region. On cross section, polymicrogyric cortex appears abnormally thin and has been described as having a “festooned” or garland appearance. A subset of these malformations is associated with an ever growing list of known genetic associations and familial predispositions.

Grossly evident heterotopias may be seen as another manifestation of FCD ( Fig. 25.3 ). Both nodular and band-like heterotopias have been described, frequently situated in the periventricular region. Laminar or band heterotopias have sometimes been referred to as “double cortex” and typically run parallel to the cortical ribbon. Lesions may be either unilateral or bilateral, with many cases now conforming to one of several X-linked and autosomal genetic disorders referred to as periventricular nodular heterotopia (PVNH) types 1–6 (see http://www.ncbi.nlm.nih.gov/omim ).

The term hemimegalencephaly refers to an asymmetrical enlargement of the cerebrum. This finding may be seen in association with other gyral abnormalities, including polymicrogyria and pachygyria and in association with neurocutaneous disorders, such as linear nevus sebaceous syndrome and tuberous sclerosis.
The cortical tubers of tuberous sclerosis are another grossly evident pattern of FCD. These lesions appear as an expanded gyrus that is very firm to palpation due to the presence of marked gliosis and calcifications. Lesions may be single or multiple and vary in size.
More subtle forms of grossly evident FCD may be encountered. On gross section, some of these may manifest with an abnormal gyral pattern or blurring of the gray-white interface ( Fig. 25.4 ). In cases with prominent gliosis, the region may be firm to palpation.
The spectrum of microscopic lesions that have been described under the general heading of FCD or a malformation of cortical development varies somewhat among expert pathologists, depending on their personal biases and thresholds for subtle lesions. For the latter in particular, immunostains for NeuN (to highlight cortical architecture), neurofilament protein (to highlight dysplastic neurons), and GFAP (to highlight patterns of gliosis) may be helpful. Depending on suspicions of low-grade neoplasms, balloon cells, and/or white matter abnormalities, other helpful stains may include MAP2 (positive in normal neurons and their processes and diffuse glioma cells, but often negative in glial component of ganglioglioma), CD34 (often highlighting balloon cells and other ramified cells in FCD ILAE type IIb, ganglioglioma, and pleomorphic xanthoastrocytoma), and Luxol fast blue/periodic acid–Schiff (LFB/PAS) to highlight blue-staining myelin, including in locations not normally encountered.
The most common histologic appearance of agyria and pachygyria is a four-layered cortex: a molecular layer and three variably thick layers of neuronal cells. However, the layered architecture is often not readily evident on routinely sectioned hematoxylin-eosin (H & E)–stained tissue sections and may be better appreciated on low-magnification examination of a NeuN immunostained section. Frequently, the malformed cortex overlies a rim of white matter that contains small gray matter heterotopias.
The microscopic appearance of polymicrogyria is more varied than that for agyria and pachygyria. The most commonly encountered phenotype involves two- or four-layered cortex. The two-layered cortex is marked by a molecular layer superimposed on a disorganized neuronal layer. Contiguous convolutions often appear fused between the molecular layers of two adjacent “gyri,” thus lacking any sulcus formation between them. Four-layered polymicrogyria is less common and includes a molecular layer with two underlying neuronal layers separated by a relatively paucicellular layer that contains myelinated fibers. As mentioned earlier, however, the individual cortical layers may be difficult to discern on routine sections, whereas the convolutions and shallow sulci are often easily appreciated on a NeuN stain ( Fig. 25.5 ).

The heterotopias are defined by the presence of gray matter aggregates within regions of the brain that normally contain only white matter. Nodular heterotopias, often periventricular in location, are marked by a disordered arrangement of neuroglial cells without any obvious layering ( Fig. 25.6 ). There may be evidence of a simple radial organization to the neurons within the heterotopia. A band heterotopia is marked by a linear arrangement of gray matter tissue, which is separated from the overlying cortex by white matter. Similar to the nodular heterotopias, there is a haphazard arrangement of neural and glial cells within the band heterotopia.
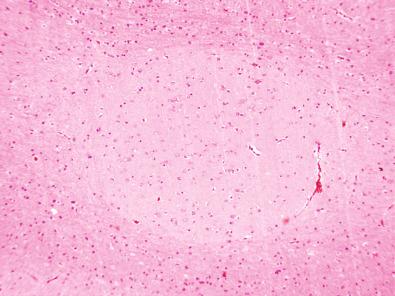
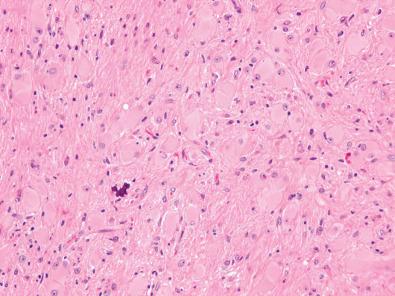
More generalized approaches to the microscopic appearance of FCD recognize distinct patterns. The most common forms are marked by architectural disorganization of the cortex, including an abnormal number of neuronal cell layers (as previously described with agyria, pachygyria, and polymicrogyria) or a disordered arrangement of neuronal cells within a given layer of cortex ( Figs. 25.7–25.9 ). Normally, neurons are oriented with their apical dendrites perpendicular to the surface. A malpositioning of neurons within a layer with cells laying askew can be seen. Additionally, neurons may be abnormally situated within the cortex; that is, large pyramidal neurons may be located in layers where they are not usually present (molecular layer and layers 2 and 4) ( Fig. 25.10 ). Other described abnormalities include persistence of a subpial granular cell layer and marginal heterotopia marked by the presence of neural parenchyma extending into the pial arachnoidal region ( Fig. 25.11 ). Most of these patterns are identifiable by routine light microscopic examination with H & E–stained sections. As stated earlier, however, some cases benefit from additional stains including neurofilament antibody, NeuN, or cresyl violet to highlight neurons, their distribution, and whether a subset is dysplastic ( Figs. 25.12–25.14 ).
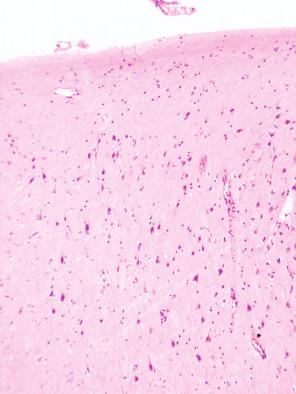
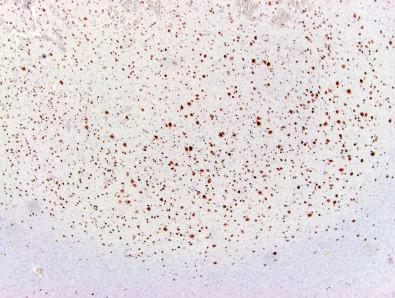
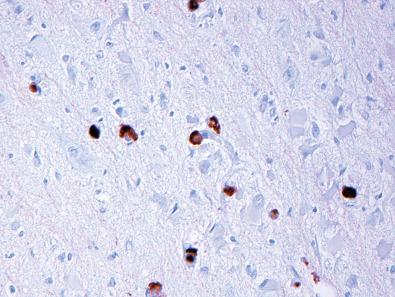
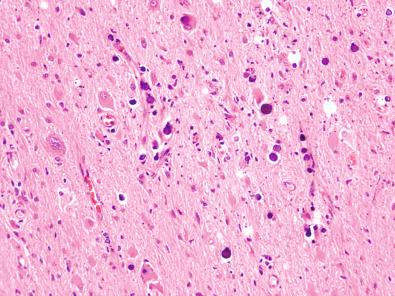
A subset of FCD is marked by neuronal cytomegaly or enlarged neuronal cells. Besides their increased size, these cells generally do not demonstrate other morphologic abnormalities. Dysmorphic neurons may also be present and are definitional for the ILAE type II subtypes (discussed later in this chapter) ( Fig. 25.15 ); they may be highlighted by a neurofilament stain that can show abnormal positivity within the cell body ( Fig. 25.16 ). These cells may be either normal size or enlarged, but they demonstrate cytologic atypia, most commonly marked by abnormalities of Nissl substance (often large and chunky or unevenly distributed), nuclear shape or size, nucleolar morphology, or cell processes. Occasionally, abnormal collections of small, rounded granular-type neurons may also be encountered. These clusters are most frequently seen in association with heterotopias and can be found rather frequently in the amygdala and hippocampal regions in patients with temporal lobe epilepsy (so-called hamartia) ( Fig. 25.17 ).
Balloon cells are a salient feature of FCD (ILAE IIb cases discussed later) ( Fig. 25.18 ). Originally referred to as the “Taylor type” dysplasia, similar appearing cells may also be encountered in the cortical tubers of tuberous sclerosis ( Fig. 25.19 ). These cells are readily identifiable on H & E staining. They are large cells with abundant “astrocytic-like” eosinophilic cytoplasm with eccentrically placed “neuron-like” vesicular nuclei, often with a prominent nucleolus. The derivation of these cells remains a matter for some debate in that they have been noted to stain with antibodies of both neuronal and glial differentiation, occasionally also aberrantly expressing CD34. Ultrastructurally, these cells are characterized by prominent numbers of intermediate molecular-weight filaments and nonmembrane-bound electron-dense globose structures. In the setting of tuberous sclerosis, these cells are accompanied by prominent gliosis and dystrophic mineralization ( Figs. 25.20 and 25.21 ).
The phenotypic variability of FCD has prompted many attempts at devising classification or “grading” systems for these lesions. The precise etiology of most cases is not known, although a variety of potential mechanisms accounting for disruptions or alterations in cortical development and neuronal migration are recognized. Consequently, most of our attempts at classifying these lesions are based purely on morphology and, in some limited basis, clinical correlates.
A variety of approaches to classification have been published in the literature over the years. These differ in terms of inclusion of grossly apparent lesions as separate diagnostic categories (or not), philosophical approaches in terms of whether one is a “lumper” or “splitter,” and how broadly or narrowly one interprets the definition of FCD. A clear association of some patterns with known genetic alterations is important to recognize and delineate. Associations with other pathologic conditions such as hippocampal sclerosis or tumors are also important to acknowledge. Some approaches have attempted to correlate morphologic findings with embryology in terms of estimating the time point in development when the lesion may have originated. More recently, efforts at correlating morphology with clinical parameters have been attempted, albeit imperfectly.
The two most recently devised and utilized approaches include the Palmini classification and the subsequently developed ILAE approach. The Palmini approach separates so-called malformations of cortical development from FCD. Mild malformations of cortical development are defined by either ectopically placed neurons in or adjacent to layer 1 (type I) or microscopic neuronal heterotopia outside layer 1 (type II). FCDs are divided into types I and II. Type I lesions are characterized by isolated architectural abnormalities such as dyslamination, accompanied or not by other abnormalities of mild malformations of cortical development (type Ia) or architectural abnormalities plus giant or immature but not dysmorphic neurons (type Ib). Palmini et al. type IIa lesions are characterized by architectural abnormalities with dysmorphic neurons but without balloon cells; type IIb lesions additionally contain balloon cells.
The ILAE classification ( Table 25.1 ) eliminates the malformation of cortical development designation and redefines the type I lesions into three subsets. ILAE type Ia is defined by abnormal radial cortical lamination, type Ib by abnormal tangential cortical lamination, and type Ic by both radial and tangential abnormalities, although it is not always easy to stratify routinely stained sections in this manner. ILAE type IIa and IIb lesions correspond to those previously described in the Palmini et al. classification. The ILAE adds a type III designation for lesions associated with other pathologies: Type IIIa lesions are associated with hippocampal sclerosis; type IIIb lesions with glial or glioneuronal tumors (or LEATs, described previously); type IIIc with vascular malformations; and type IIId with other lesions such as trauma, ischemic injury, and encephalitis.
| FCD Type | Criteria |
|---|---|
| ILAE Ia | Isolated lesions presenting as radial dyslamination of neocortex |
| ILAE Ib | Isolated lesions presenting as tangential dyslamination of neocortex |
| ILAE Ic | Isolated lesions presenting as both radial and tangential dyslamination |
| ILAE IIa | Isolated lesion characterized by cortical dyslamination and dysmorphic neurons without balloon cells |
| ILAE IIb | Isolated lesion characterized by cortical dyslamination and dysmorphic neurons with balloon cells |
| ILAE IIIa | Occurs in combination with hippocampal sclerosis |
| ILAE IIIb | Occurs with epilepsy-associated tumors |
| ILAE IIIc | Adjacent to vascular malformations |
| ILAE IIId | In association with epileptogenic lesions acquired in early life (i.e., traumatic injury, ischemic injury, or encephalitis) |
| Palmini IA | Isolated architectural abnormalities (dyslamination, accompanied or not by other abnormalities of mild malformation of cortical development, or MCD) |
| Palmini IB | Architectural abnormalities, plus giant or immature, but not dysmorphic, neurons |
| Palmini IIA | Architectural abnormalities with dysmorphic neurons but without balloon cells |
| Palmini IIB | Architectural abnormalities with dysmorphic neurons and balloon cells |
Studies have examined the reproducibility of diagnoses using both approaches. Both approaches have good interobserver and intraobserver variability associated with the type II lesions. Reproducibility of diagnoses is not nearly as good for distinguishing between type I and with the ILAE type III lesions. The clinical differences between type I and II lesions in both classifications are well recognized. The importance of distinguishing among subtypes of type I lesions and between malformations of cortical development and type I lesions (in the Palmini approach) are not so clear. One recent study looking specifically at postsurgical outcomes between ILAE Ib and Ic subtypes showed no significant difference with respect to seizure frequency postsurgery for the subtypes; similar findings were noted in comparing the Palmini et al. Ia and Ib subtypes.
There is a well-known association of FCD with certain low-grade glioneuronal tumors or LEATs, most notably ganglioglioma and the dysembryoplastic neuroepithelial tumor. From a differential diagnostic standpoint, distinguishing a focal cortical dysplasia from a dysembryoplastic neuroepithelial tumor is not difficult; however, gangliogliomas may at times present a challenge. Helpful features of ganglioglioma include the presence of a clearly atypical glial cell (gliomatous) component, an atypical neuronal cell component, and the radiologic appearance of a mass. The neoplastic glial nuclei can often be highlighted with immunostains for GFAP, although sometimes it is difficult to distinguish background processes. In such cases, the cytologically atypical nuclei can often be highlighted on OLIG2 and SOX10 stains, which normally only stain the small rounded nuclei of oligodendrocytes. Additionally, gangliogliomas often feature eosinophilic granular bodies and perivascular lymphocytes, neither of which frequent FCDs. Lastly, a subset of gangliogliomas are immunoreactive for the BRAF V600E mutant protein, a feature not found in FCDs. Nevertheless, cases of gangliocytoma may closely mimic FCD and the distinction may rest on whether the lesion has the appearance of a mass or not.
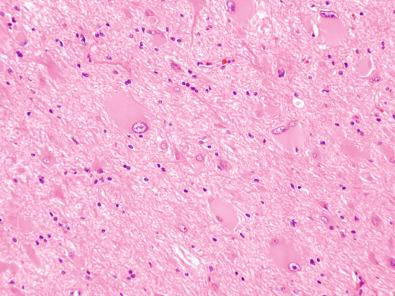
Changes adjacent to a remote infarct can be marked by architectural disorganization, particularly in such lesions that develop early in life, when the brain is still developing, Often, however, the infarct is accompanied by areas of cystic degeneration (cystic encephalomalacia) and marked cortical atrophy with loss of neurons and gliosis. The distinction at times may become arbitrary in that many focal cortical dysplasias likely arise secondary to ischemic damage sustained during brain development.
Ancillary studies may be useful in certain circumstances in the evaluation of focal cortical dysplasia. In many cases, the morphologic findings are readily evident on careful examination of H & E–stained sections. More subtle abnormalities, as previously mentioned, might benefit from additional antibody stains, such as NeuN or GFAP stains. Currently, no immunomarkers or molecular markers can reliably predict prognosis in a particular case.
Morphologically, cases marked by dysmorphic neurons and balloon cells (i.e., the type II patterns) are more likely to demonstrate a high degree of intrinsic epileptogenicity. Seizures are more often severe in this setting, and the pathology may be extensive or multifocal in some patients. As such, response to surgical intervention is often not as good as it is in the more subtle forms (type I) or more localized cases.
Some FCDs are associated with known genetic alterations. Most of these are relatively unusual entities and as a group constitute a minority of cases. It is beyond the scope of this chapter to discuss each in detail.
The general approach to treating focal cortical dysplasia is pharmacologic management. When this fails, surgical intervention may be necessary. Localized lesions are more amenable to partial lobectomy. More extensive pathology may require more extensive resection and in extreme cases a hemispherectomy. Lesions visualized on MR images make for better surgical targets. Surgical outcomes are still suboptimal in some cases. Reasons for inadequate postoperative seizure control vary and may include a failure to detect the full extent of the disease, the presence of multifocal disease, or the presence of dual or in rare cases triple pathology. Success may also at times be limited by the presence of functional cortex within or near the lesion, limiting resectability. Seizure-free status following surgery for focal cortical dysplasia ranges from 11% to 70%.
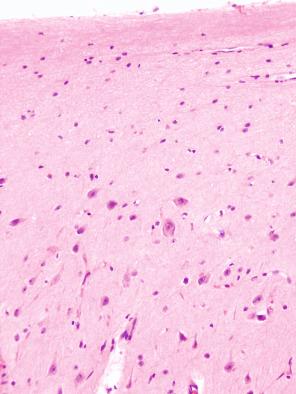
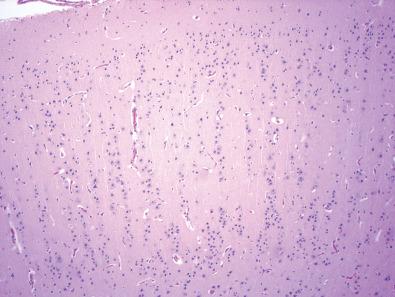
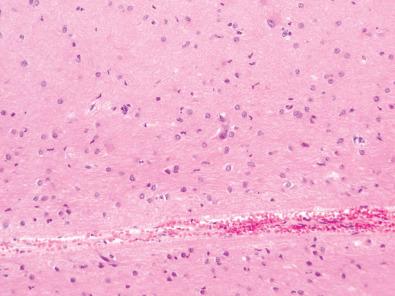
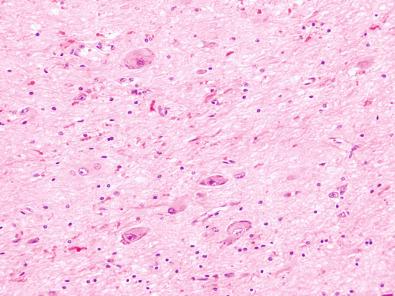
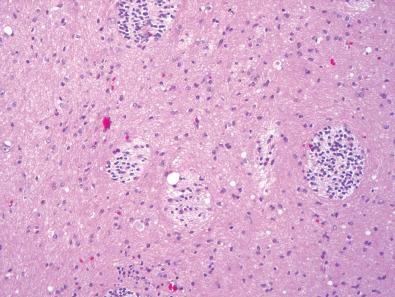
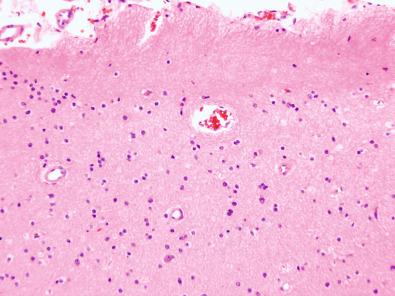
Hippocampal sclerosis is associated with chronic epilepsy and is characterized by severe segmental loss of neurons with accompanying gliosis in one or more regions of the hippocampal formation. Related lesions include Ammon's horn sclerosis, mesial temporal sclerosis, endplate sclerosis, and incisural sclerosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here