Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Patellar instability remains a problematic entity in the athletic patient population. Most studies agree that adolescent females represent the highest risk group of patients for first-time patellofemoral dislocation. Treatment of patellar instability must be individualized, with care taken to identify both historical and anatomic risk factors. First-time instability that results in a loose chondral or osteochondral body should be addressed with both attention to the loose piece and the stabilization of the joint, most commonly in the form of medial patellofemoral ligament (MPFL) reconstruction. Treatment of recurrent instability begins with MPFL reconstruction and involves the addition of realignment procedures and/or reshaping of the dysplastic trochlea, according to the limited available literature and surgeon judgment. This chapter will focus on the recognition and treatment of patellar instability in the female athlete.
Most studies agree that adolescent females are the highest risk group of patients for first-time patellofemoral dislocation. Other risk factors include family history, history of contralateral instability, and a number of anatomic factors.
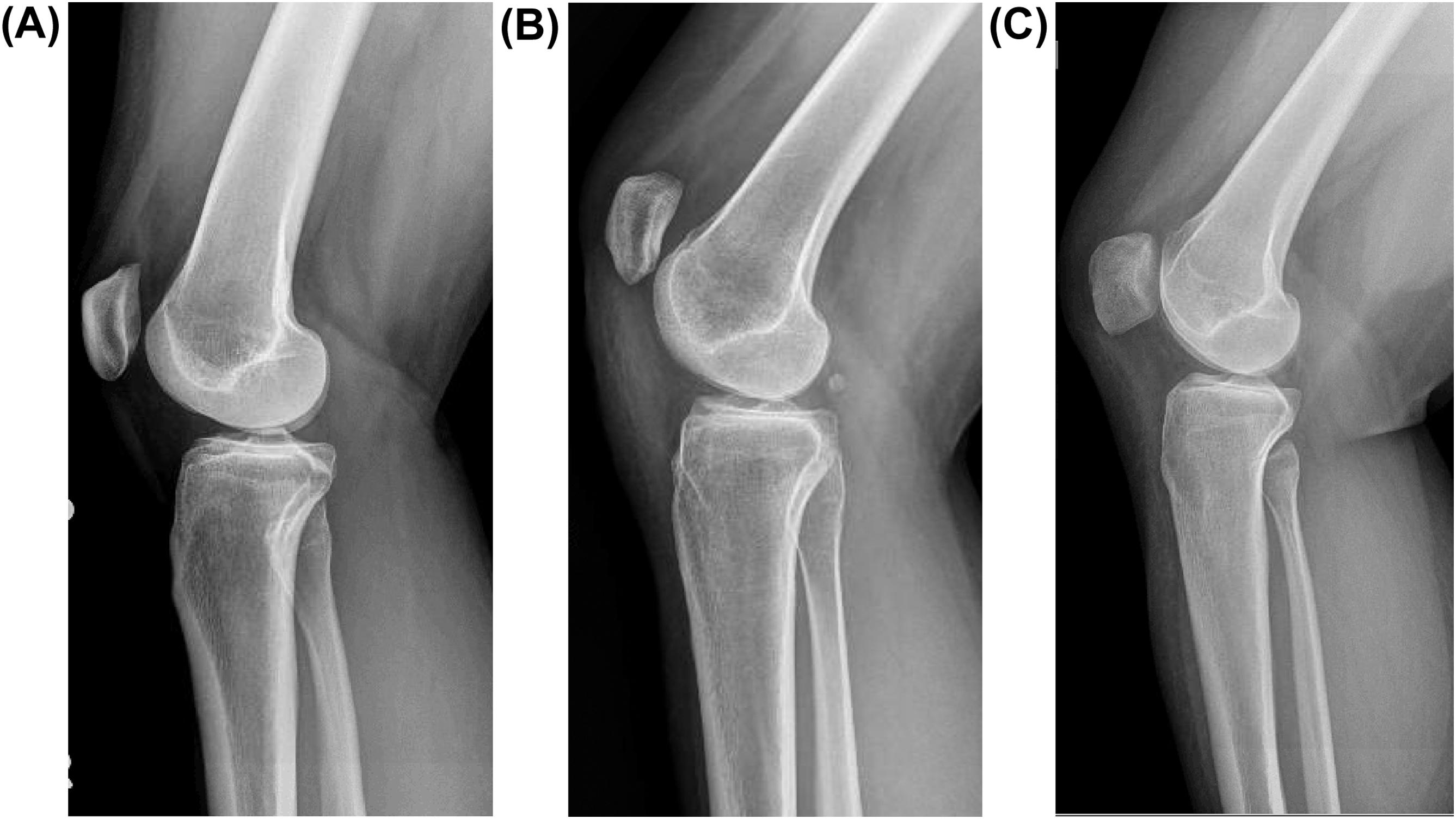
The most predictive anatomic risk factor for patellar instability is trochlear dysplasia. Several different classification systems and strategies have been employed to describe an abnormally shaped trochlea, including the Dejour classification, sulcus angle, trochlear depth, and trochlear facet ratio. Others focus simply on the anterior height of any supratrochlear “spur,” or “boss” as predictive of recurrence. A complete understanding of the three-dimensional nature of a dysplastic trochlea can prove elusive, but many studies have concluded that trochlear dysplasia, no matter its definition, emerges as the most predictive of the risk factors for recurrence following a first-time patellofemoral dislocation. Thus many surgeons discard the precise quantification of dysplasia and classify it on a lateral X-ray or cross-sectional imaging simply as mild, moderate, or severe ( Fig. 8.1 ).
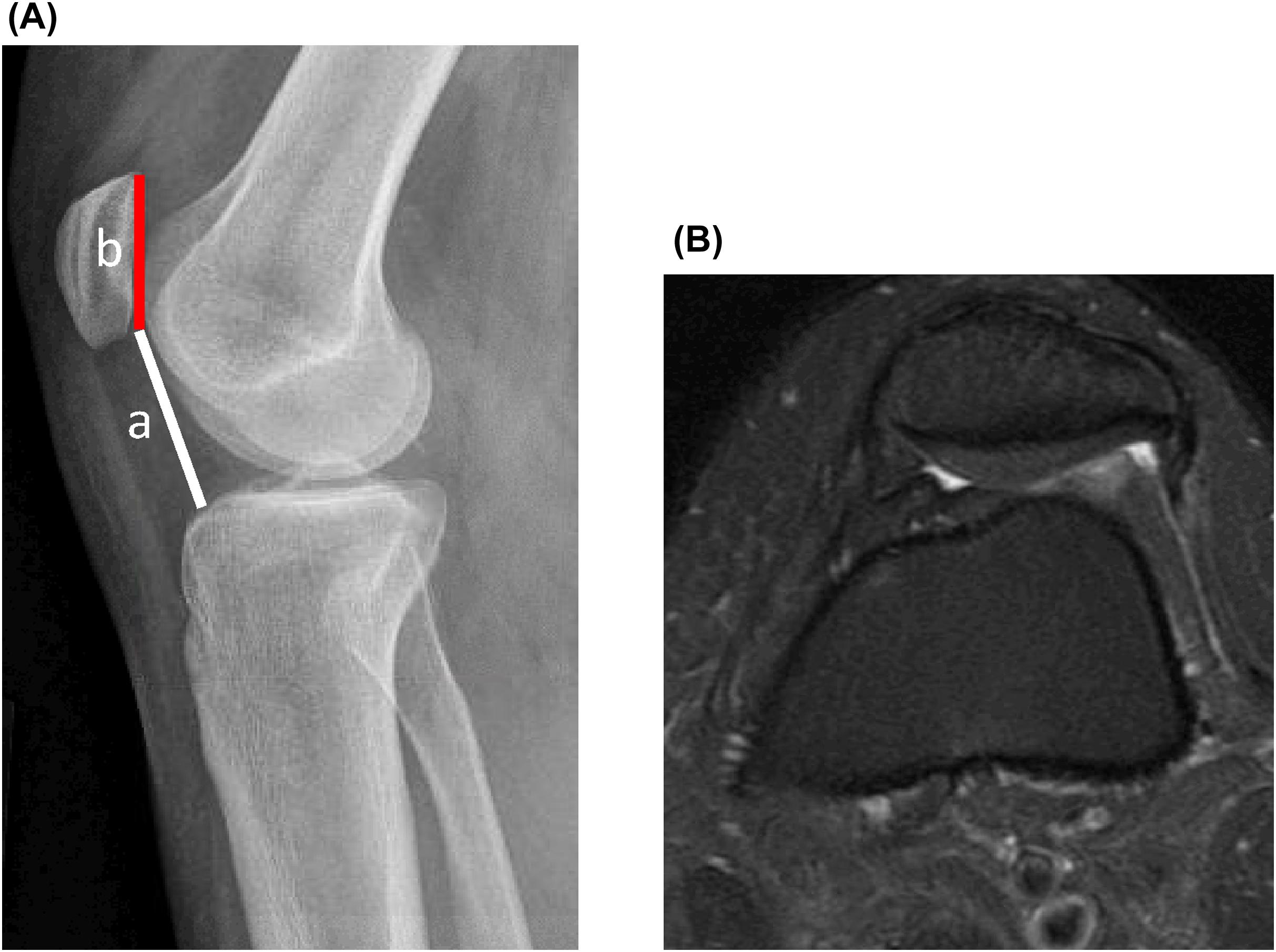
Patella alta has also been described as a risk factor for recurrent instability. This risk factor has also been measured in several ways, some of which reference either the joint line (Blackburne-Peel) or the tibia (Insall-Salvati, modified Insall-Salvati, and Caton-Deschamps). Others have focused on the relationship of the patella to the femur and/or femoral trochlea, including simple articular overlap, Biedert's patellotrochlear index, and/or Dejour's sagittal patellofemoral index. The latter strategy is attractive because the relationship of the patella to the trochlea seems most relevant in the measurement of patellar height. However, these measurements require magnetic resonance imaging (MRI) and can be confounded by a laterally tracking patella and difficulty identifying the precise distal location of the transition from trochlear groove to femoral condyle. In principle, patella alta indicates that a higher riding patella requires more knee flexion to engage and stabilize the patella in its trochlear groove. This places more stress on the soft tissue restraints of the knee during early flexion until bony congruity and its inherent stability take over. An axial MRI can provide clues that patella alta is present, when the patellar chondral surface is visualized without the corresponding trochlear cartilage in view ( Fig. 8.2 ).
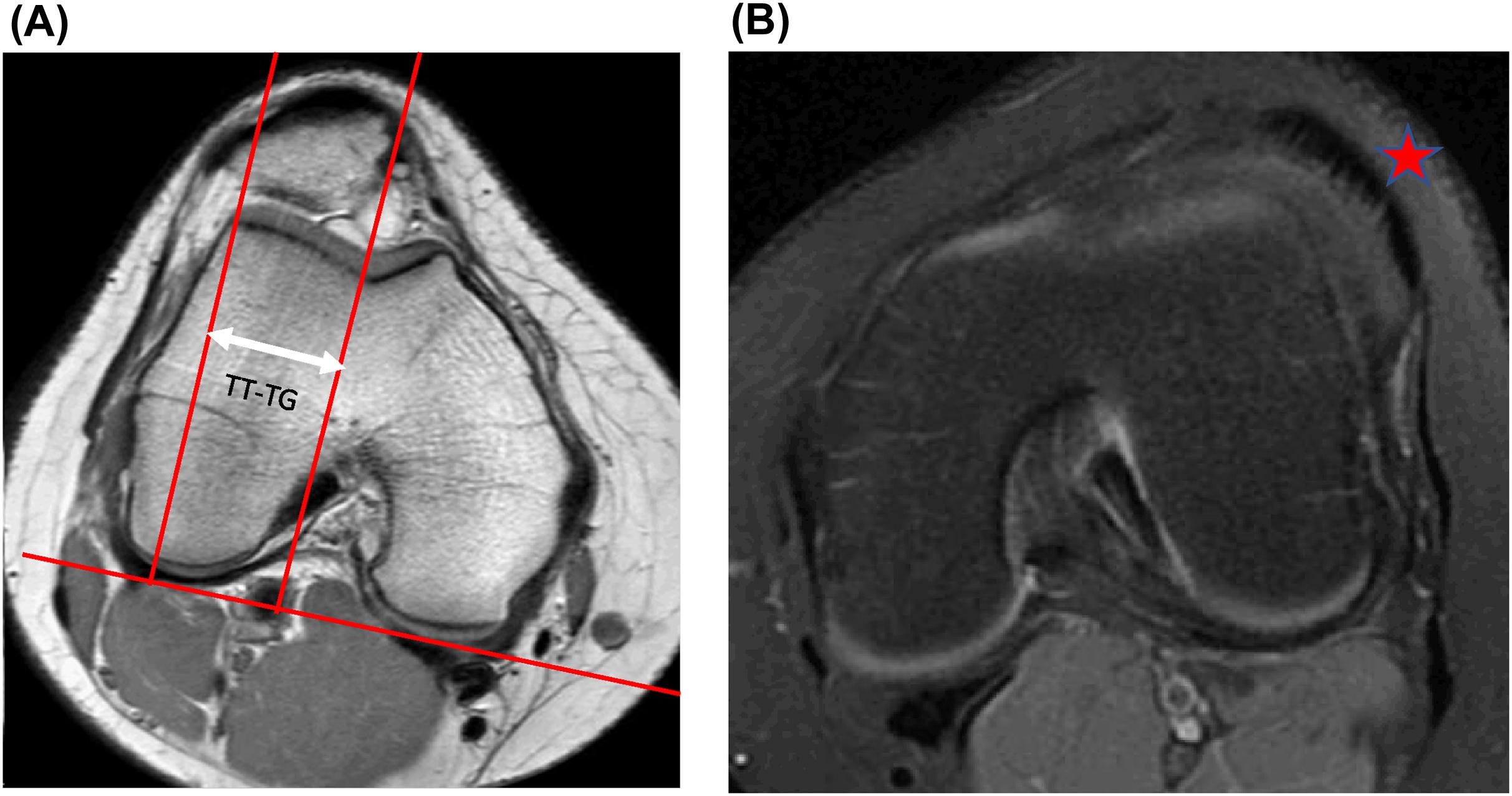
Coronal alignment also plays a role in patellar stability. Significant genu valgum is useful to recognize during skeletal immaturity, as guided growth or hemiepiphysiodesis can be a simple intervention to resolve this problem, rather than a more invasive distal femoral osteotomy if correction is required in a skeletally mature patient. More complicated is the understanding of the path taken by the extensor mechanism as it crosses the knee. Arthroplasty surgeons often use the tibial tubercle-to-posterior cruciate ligament (PCL) distance (TT-PCL), a measure of the lateralization of the tibial tubercle relative to the PCL origin on the tibia. For patellar stability, this has not been shown to be as predictive as the tibial tubercle-to-trochlear groove (TT-TG, Fig. 8.3A ) distance, a measure of the distance from the trochlear groove nadir to the midpoint of the tibial tubercle. The difference indicates that something about the dynamic rotation of the tibia with knee flexion and extension contributes to patellar stability. More recently, attention has been paid to the location of the patellar tendon relative to the lateral trochlea ( Fig. 8.3B ). One group even found this factor to be more predictive of patellar instability than the TT-TG.
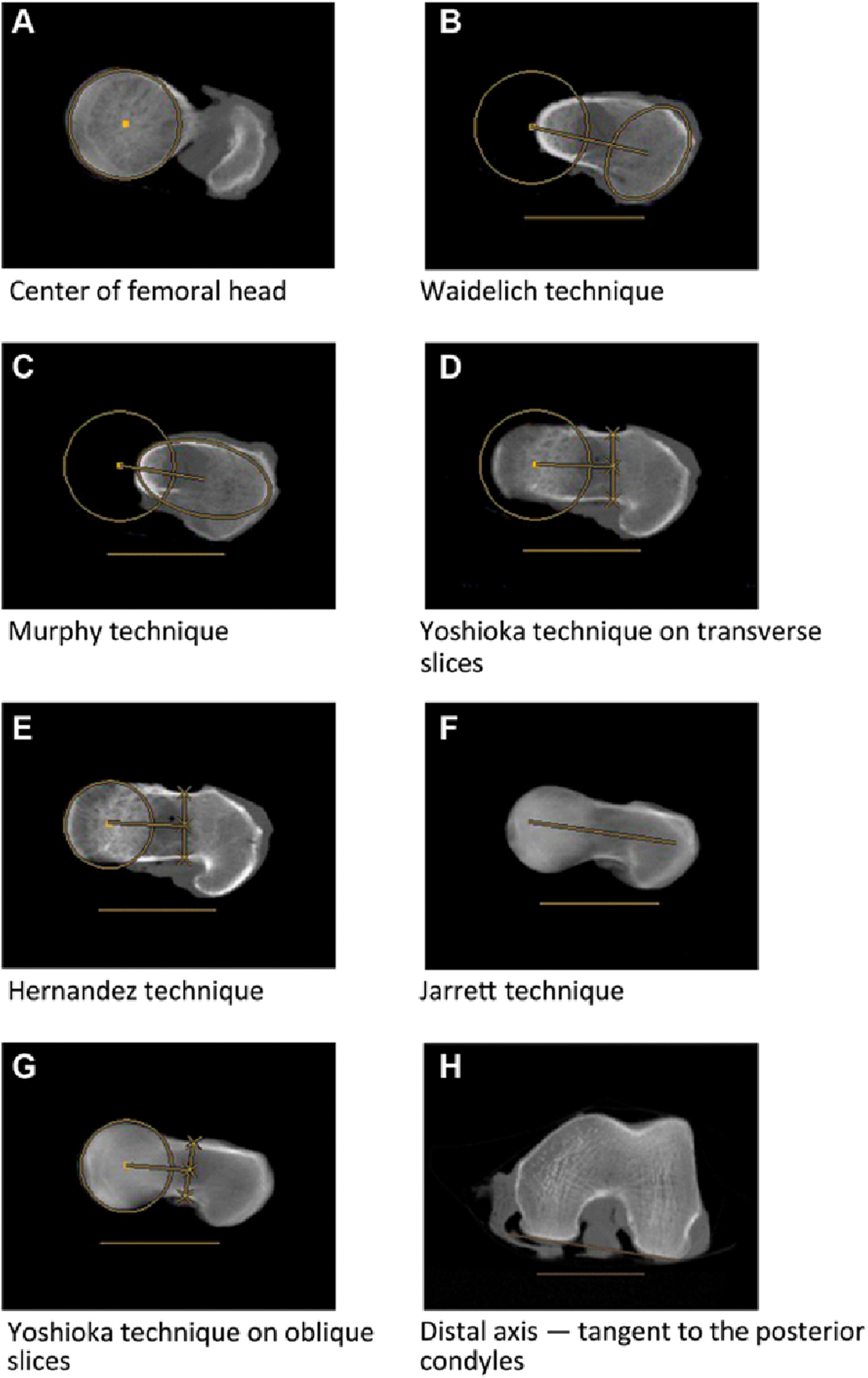
Perhaps the most poorly understood risk factor of all is femoral anteversion, in part because it is not always routinely measured in the process of evaluating an unstable patellofemoral joint. Average femoral anteversion is 15 degree, and some authors have demonstrated that even at 20 degrees, the patellofemoral joint exhibits abnormal lateral forces. Many different methods of measuring femoral anteversion have been suggested, rendering comparison of studies difficult ( Fig. 8.4 ). Literature guidance for correction of femoral anteversion in patellofemoral instability is limited, but surgeons who commonly perform derotational femoral osteotomy procedures cite a margin of error of 10–15 degrees during the procedure and therefore do not intervene unless the femoral neck is 30–35 degrees or more anteverted relative to the shaft.
Other factors such as ligamentous laxity and lower extremity motion patterns with jumping and landing have been implicated in patellar instability, but little is known precisely about how they should affect surgical management or factor into rehabilitation protocols.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here