Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pancreaticoduodenectomy (PD) is one of the few remaining operations where major morbidity rates hover in the range of 25% and the 90-day mortality rate remains in the 2% to 4% range, even under the care of the highest-volume surgeons at the highest-volume centers. This chapter will describe an approach to the exploration, resection, and reconstruction of patients undergoing PD with the understanding that multiple techniques have been shown to be equally as effective and with the recognition that individual steps of the procedure may—and should—be performed in a different order depending on the nature and location of the abnormality. Although I am the sole author on this chapter, my use of the terms “we” and “our” is to recognize that this approach is derived from my current and former mentors and colleagues (namely, Murray Brennan, Leslie Blumgart, William Jarnagin, and Michael D’Angelica) and from other pancreatic experts in centers at which I have had the privilege to collaborate (namely, Johns Hopkins Hospital, Massachusetts General Hospital, University of Verona, and University of Heidelberg).
This chapter will focus on the specific technique of open PD. Minimally invasive approaches (laparoscopic and robotic) are described in a later chapter (see Chapter 127 ). Minimally invasive PD has been developed over the past 20 years; however, more than 95% of these operations continue to be performed with an open technique. The data published to date suggest that a minimally invasive approach to PD can be performed safely with equivalent outcomes to the open approach in very select high-volume centers that have a team dedicated to this endeavor.
Exploration of the abdomen should be initially performed to rule out subradiographic metastatic disease, which would be a contraindication to resection. The use of staging laparoscopy (SL) for patients with adenocarcinoma of the pancreas is subject to individual surgeon preference and institutional experience (see Chapters 24 and 62 ). Reports have suggested that SL is currently performed routinely, selectively, or never. The yield of SL will decrease as the quality of cross-sectional imaging increases. Our current approach is to perform SL in a selective fashion, on a case-by-case basis. Indications for SL include a concerning feature on preoperative imaging or a significantly elevated carbohydrate antigen (CA) 19-9 level. The degree of elevation in CA 19-9 that warrants SL is variable among different studies and ranges from 130 to 250 U/mL. Attention should be paid to the status of the biliary tree at the time of CA 19-9 evaluation because biliary obstruction can increase the CA 19-9 level.
When SL is not felt to be necessary, the operation should begin with a limited upper midline incision. The initial incision should be small to do a visual and manual inspection for metastatic disease, particularly when operating for cancer. Careful inspection of the liver and peritoneal surfaces should be performed, and targeted liver ultrasound should be considered for any liver parenchymal abnormalities (see Chapter 24 ). Once metastatic disease is ruled out, the incision should be extended to whatever length is needed to perform and complete the operation safely for that individual patient.
For more information, see Chapter 2 .
Once retractors are applied, a wide Kocher maneuver is performed to the level of the aorta and the left renal vein, including mobilization of the ligament of Treitz from the patient’s right side. To facilitate this maneuver, the transverse mesocolon is mobilized off of Gerota’s fascia and the head of the pancreas, allowing for dynamic and manual retraction of the transverse colon and its mesentery caudally to optimize exposure. This enables an assessment of the retroperitoneum and relationship of the mass with the superior mesenteric artery (SMA; Fig. 117A.1 ). During the Kocher maneuver, there is no routine oncologic reason to enter Gerota’s fascia of the right kidney or to remove posterior aortocaval lymph nodes. Both of these maneuvers may increase specific risks of the operation, such as lymphatic leak, and provide no proven oncologic benefit. Care should be taken to avoid the right gonadal vein as it enters the inferior vena cava (IVC) because this vein is thin walled and if injured will result in brisk bleeding.
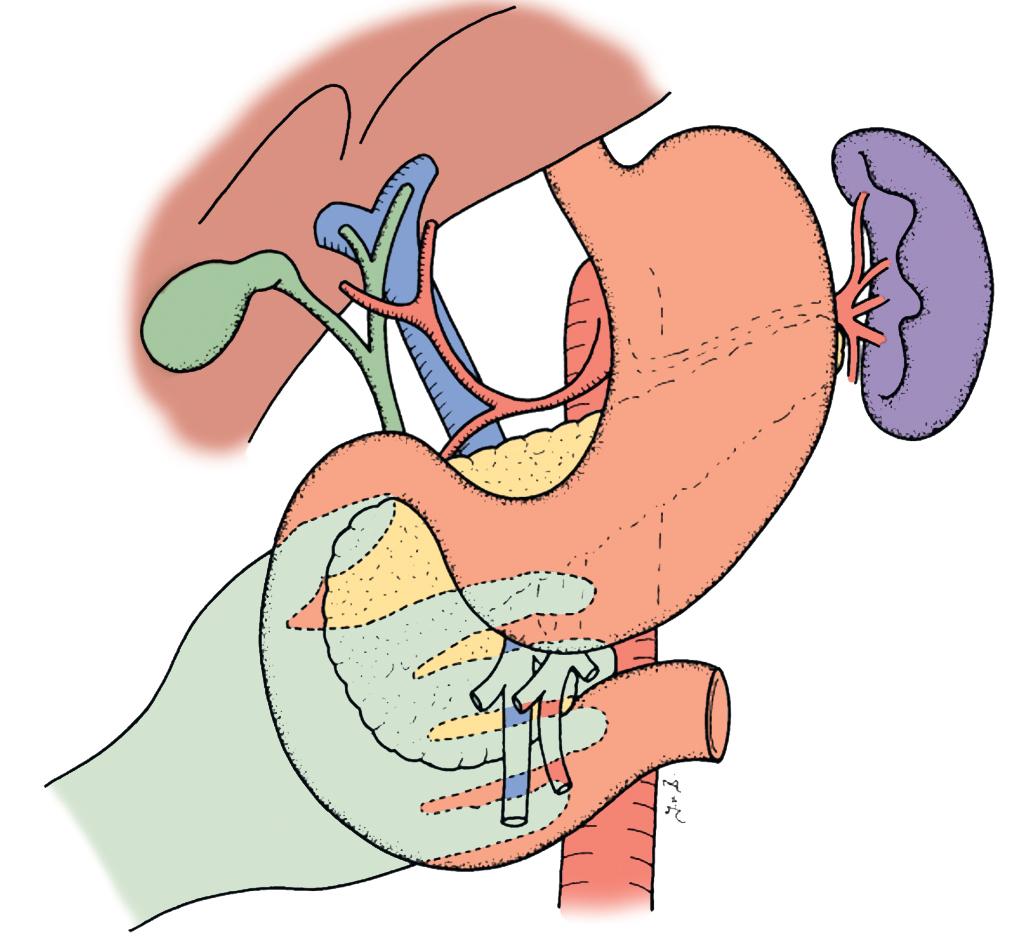
At this time, the SMA can also be inspected from the ligament of Treitz and dissected on its right lateral surface to exclude any tumor infiltration. This approach has been termed the artery-first approach ( Fig. 117A.2 ) and may help with assessment of SMA involvement early in exploration. We do not routinely perform this particular maneuver because high-quality preoperative imaging and careful palpation in the operating room are typically adequate for excluding gross SMA involvement.

After Kocherization, access to the lesser sac should be achieved through dissection of the greater omentum off of the transverse colon. Some surgeons may enter the lesser sac by directly dividing the omentum near the gastroepiploic vessels. Although this may seem to be the more direct and technically easier approach, it will result in an ischemic distal omentum as the branches from the gastroepiploic arcade are divided. In an obese patient with significant omental bulk, this ischemic tissue is at risk for postoperative infection, particularly in the setting of postoperative pancreatic leak. An additional advantage to lifting the omentum off the transverse colon to enter the lesser sac is that the healthy perfused omentum can be later used as a vascularized flap to cover the pancreatic and biliary anastomoses, and gastroduodenal arterial (GDA) stump, at the conclusion of the operation.
Careful dissection in the avascular plane between the hepatic flexure and the duodenum and extension of the Kocher maneuver separates the third part of the duodenum from the colonic mesentery. The avascular plane between the gastroepiploic and middle colic veins is divided as it leads to the superior mesenteric vein (SMV) at the inferior edge of the pancreas. Several small crossing vascular branches may be encountered and should be prospectively divided. The gastroepiploic vein may be ligated at this point; however, reserving this until after the pancreatic neck has been divided can make this maneuver more efficient. The SMV is now identified, and early development of the tunnel between the pancreatic neck and SMV and portal vein (PV) confluence should be achieved.
Once the inferior border of the pancreas and SMV have been identified, attention should be turned to the supraduodenal compartment. While retracting the stomach anteriorly and inferiorly, the gastrohepatic ligament should be incised from the lesser curve of the stomach to the origin of the right gastric artery (RGA). The RGA should then be retracted anteriorly and the avascular tissue between the GDA and RGA incised. This maneuver will expedite the division of the RGA. The common hepatic artery is reliably identified by removing the lymph node that sits anterior to it, known as the “common hepatic artery lymph node.” This node has been referred to by some as “the node of importance” because its involvement with disease may have some prognostic value in patients with pancreas cancer. , Regardless, it should generally be removed and sent for pathologic evaluation, but it should not be used as a determinant of proceeding with resection. The GDA can then be encircled and clamped to ensure a preserved pulse in the right and left hepatic arteries. This excludes misidentification of the GDA or a tight celiac artery stenosis that makes hepatic arterial inflow dependent on retrograde flow from the GDA. Once it is deemed safe to divide the GDA, it is ligated and divided.
There are two points worth emphasizing around the ligation of the GDA. First, one must be prepared for “what to do” if the pulse within the hepatic artery is lost, or diminished, when the GDA is clamped. Careful preoperative assessment of high-quality contrast enhanced imaging is essential (see Chapter 17 ). Clinically significant celiac stenosis and retrograde GDA flow is typically evident on preoperative imaging through arterial collateralization around the pancreatic head or an enlarged GDA. In this setting, attempts should be made to divide the fibrotic attachments resulting in the stenosis; however, in our experience, this rarely results in a normal pulse. Even after clamping (and subsequent division), intraoperative duplex ultrasound will generally identify continued flow in the hepatic artery, and in this setting we proceed with resection. The second consideration is how critically important GDA ligation is to minimizing the morbidity and mortality of PD. GDA stump blowout is a significant contributor to postoperative mortality and has been reported in as many as 6% of patients. Because of this, a variety of tissue coverage techniques (falciform ligament, omentum) to protect this site of ligation from infection and leak have been recommended. , In general, we perform triple ligation of the GDA stump (tie, suture ligation, and clip) and will attempt to place omentum over the stump at the end of the case.
Ligation of the GDA exposes the anterior surface of the PV lying below. The anterior surface of the PV is dissected free, and the lateral border is identified. The lateral portal lymph nodes are mobilized away from the bile duct and brought down toward the duodenum to be included in the specimen. With the PV in view, the bile duct is encircled. In 10% to 15% of patients, a replaced or accessory right hepatic artery will course just posterior and lateral to the bile duct. Attention must be paid to assessing for this, and it should generally be preserved if present. In the absence of jaundice, however, either an accessory or replaced right hepatic artery can typically be safely ligated and resected, if indicated for oncologic reasons. This, however, should be avoided in the setting of jaundice because of the possible complication of postoperative right liver necrosis.
At this point, there should be a final assessment of the pancreatic neck and overall resectability. Before proceeding, many surgeons will create a tunnel behind the pancreatic neck to ensure that the vein is uninvolved, or if it is involved, that safe resection can be performed (see section on transection). Our approach is to attempt creation of the tunnel when the vein does not appear to be involved on preoperative imaging. Nevertheless, when PV resection and reconstruction is either possibly or definitely going to be required, it may not be safe to complete this tunnel without some division of the pancreas. In this latter circumstance, one must often determine whether PC reconstruction can be safely performed without creating a complete tunnel. This assessment of the pancreatic neck, and PV, is critical and can be subtly difficult. Intraoperative consultation with senior partners should be considered when there is not complete clarity on the extent of vascular involvement. Good decisions come from experience, and experience comes from making bad decisions.
Once deemed resectable, a cholecystectomy is performed, usually in an anterograde fundus-down technique. In patients with preoperative biliaryobstruction, the gallbladder can be distended and inflamed. Sometimes emptying the gallbladder of its contents can facilitate its dissection and removal. As the gallbladder is separated from the liver, the cystic artery and duct are identified and ligated. Care should be taken to avoid any iatrogenic injury to the right hepatic artery, which usually runs posterior to the common hepatic duct (see Chapter 2 ). Some will leave the gallbladder attached and divide the common hepatic duct, whereas others will ligate the cystic duct and later divide the common bile duct. In the setting of pancreatic cancer, where a positive bile duct margin is generally not an issue, our approach is to ligate the cystic duct and then later divide the bile duct. In the setting of cholangiocarcinoma of the distal bile duct, however, our approach is to leave the gallbladder attached and later divide the common hepatic duct to achieve a negative margin.
Once the gallbladder is removed, the stomach is transected with two fires of a gastrointestinal stapler (GIA stapler) just distal to the incisura. Whether or not to resect or preserve the pylorus is a question that has resulted in more than eight clinical trials over three decades with over 1000 patients being prospectively evaluated. These studies have demonstrated no difference in outcome, and therefore any debate over an advantage or disadvantage to pylorus preservation is an exercise of opinion rather than an exercise in evidence-based medicine. , If preservation of the pylorus is planned, the right gastric and right gastroepiploic arteries are divided 2 cm beyond the pylorus, and the duodenum is skeletonized. The duodenum is divided and the stomach, along with the omentum, is packed away in the left upper quadrant.
At this time, attention is directed toward dividing what remains of the ligament of Treitz and jejunal transection. The body wall retractors are adjusted to expose the ligament of Treitz and the jejunum is then transected. The location of transection chosen, particularly the distance from ligament of Treitz, is partly affected by the planned route of the biliary-pancreatic limb for reconstruction, namely, via the ligament of Treitz or through the transverse mesocolon. The site of transection should allow for ample mesenteric mobility to enable a tension-free anastomosis for biliary and pancreatic reconstruction. Once the jejunum is transected, the mesentery is divided close to the bowel on the specimen side down to the level of the root of the mesentery and the uncinate process of the pancreas. Because of the potential for postoperative hemorrhage from the proximal jejunal mesentery, it is our practice to control these vessels with the LigaSure device in combination with clips. The ischemic jejunal limb is then rotated under the ligament of Treitz to the right upper quadrant.
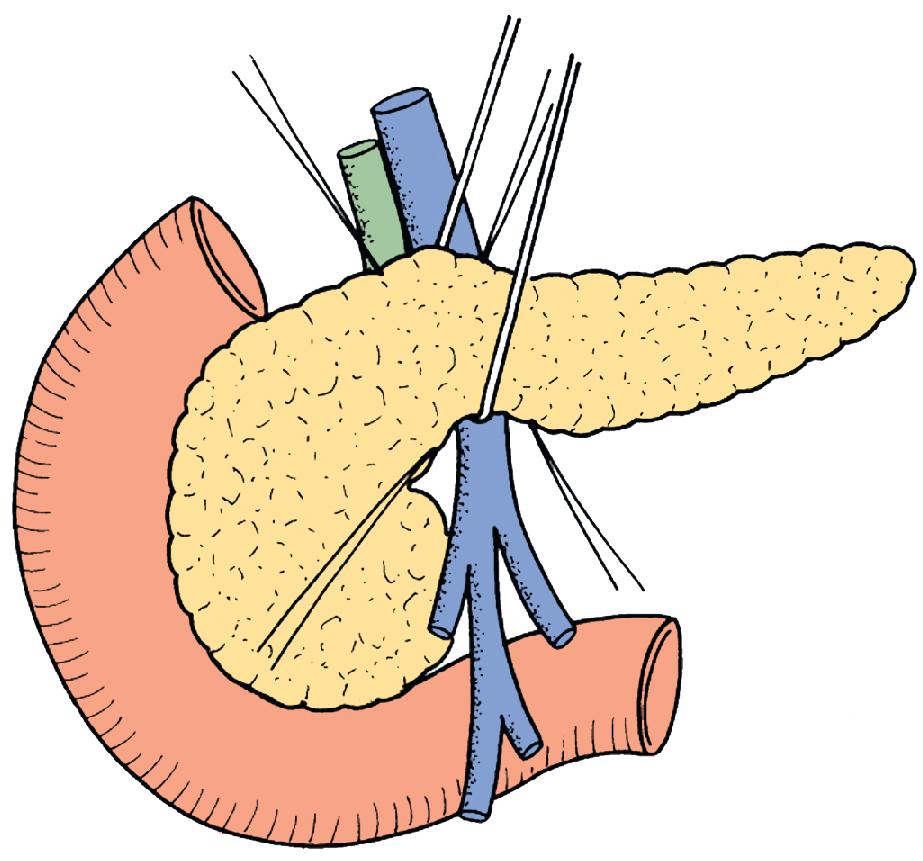
In preparation for pancreatic neck transection, the tunnel over the PV is fully developed. A Penrose drain or vessel loop can be placed into this tunnel to encircle the neck when possible ( Fig. 117A.3 ); alternatively, a renal pedicle clamp can be used to guide the transection. Hemostatic sutures are placed at the superior and inferior borders of the pancreas on each side of the planned transection plane, being careful not to include the pancreatic duct. These sutures serve to ligate the superior and inferior pancreatic vessels running longitudinally in the pancreatic parenchyma and to decrease bleeding from the cut surface after transection. The superficial portions of the pancreas can be divided with electrocautery to minimize bleeding, but the deeper gland, especially the pancreatic duct, should in general be divided sharply with a scalpel. Division of the bile duct is typically reserved for this point in the operation to minimize the duration of bile drainage into the right upper quadrant, especially in preoperatively stented patients. Some will place a clamp on the distal bile duct to further minimize the spillage of bile. At this time, the SMV-PV is dissected away from the pancreas and tumor. Any small venous branches are controlled with clips, ties, or a coagulation device.
Once the vein is completely freed, attention is directed toward the SMA dissection. Releasing posterior attachments of the specimen to the retroperitoneum facilitates the dissection along the right lateral plane of the SMA. Once the specimen’s attachments are isolated to the lateral aspect of the SMA, the dissection is completed along this plane to remove the specimen. During this step, the specimen that comprises the pancreatic head, duodenum, and proximal jejunum is retracted to the patient’s right, and the position of the SMA is continuously assessed to avoid any injury. Aided by gentle retraction of the SMV toward the patient’s left, the anterolateral aspect of the SMA is completely skeletonized of its investing tissues. This can be done by making small windows in the tissue and sealing it with either ties, clips, or a coagulation device, such as the LigaSure. Clips can be used in combination with a coagulation device as well, especially on the inferior pancreaticoduodenal artery. A stapled transection should typically be avoided, particularly when there is concern regarding the oncologic margin.
If venous resection is required, the dissection along the SMA should be performed first to leave the venous resection as the last step. This minimizes clamp time on the PV and allows for more expeditious proximal and distal venous control. Also, control and often ligation of the inferior mesenteric vein, splenic vein, and left gastric vein is necessary to isolate the SMV-PV before doing a venous resection. Once the specimen is removed, hemostasis is ensured, and the operative field is washed with warm fluid before proceeding to the reconstruction phase.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here