Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
An unexplained pancreatic mass and a bile duct stricture are the major indications for cytologic evaluation of the pancreas and bile ducts. Imaging studies contribute useful information on the location, distribution (solitary, multiple, or diffuse), and nature (cystic vs solid) of a lesion, but a cell sample is usually necessary for definitive diagnosis. In the case of a potentially resectable mass that is malignant by imaging, however, the value of preoperative aspiration or brushings is still debated. For clearly operative candidates, increased cost, potential delay in diagnosis, and imperfect negative predictive value attributed to aspiration and brushings are cited as arguments to proceed with surgical resection without preoperative cytology in this scenario. Still, many clinicians request a tissue diagnosis, even in this circumstance, because radiologic accuracy is not 100%. Despite improvements in surgical technique, the morbidity of pancreatic surgery is significant, and not all malignancies are surgically managed (e.g., lymphoma). Moreover, nonsurgical management of patients with a benign neoplasm or premalignant disease is increasingly common. The more-recent advent of neoadjuvant treatment of borderline resectable and nonresectable disease, however, has made pretreatment diagnosis imperative.
Fine-needle aspiration (FNA) of the pancreas can be performed percutaneously (by a radiologist) or endoscopically (by a gastroenterologist). A percutaneous pancreatic FNA is performed using computed tomography (CT). Percutaneous needle placement techniques vary depending on the location of the lesion and the trajectory of the needle. The tandem technique involves placing a guide needle to serve as a reference point for the second, a biopsy needle, and is most useful in CT-guided FNA where real-time visualization of needle insertion is impossible. The coaxial technique involves inserting a larger-caliber needle to localize the lesion. A smaller-caliber needle is then inserted through the larger needle to sample the lesion. This method permits multiple sampling attempts without the increased risk to local structures created by repeated needle passes.
Percutaneous FNA of the pancreas has been largely replaced by endoscopic ultrasound (EUS)–guided FNA because it provides real-time visualization of the needle tip, better visualization of small lesions than CT, and the ability to identify local metastases or invasion of local structures, thus permitting simultaneous diagnosis and staging. EUS equipment consists of an image guidance system and an echoendoscope placed into the stomach or duodenum. A high-frequency ultrasound transducer on the tip of the echoendoscope guides a 19- to 25-gauge needle through the gut wall into the pancreatic mass or cyst. Pancreatic head masses benefit from a transduodenal approach, and body and tail masses from a transgastric approach. The pathologist should be aware of the approach so that contaminating normal gastric or duodenal mucosa is recognized and not misinterpreted as lesional. Once in the lesion, the stylet is removed and the needle oscillated with or without suction to dislodge cells and pull them into the needle.
With cystic lesions, as much fluid is drained as possible. Depending on volume, cyst fluid can be submitted for routine cytology, biochemical, and molecular analysis. Any visible mural nodule or solid component should be separately sampled.
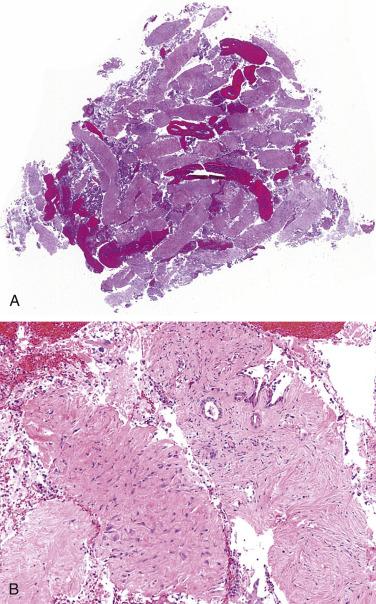
Next-generation needles have greatly improved diagnostic yield by producing histologic tissue fragments and mini-core biopsies ( Fig. 14.1 ). A micro forceps biopsy needle that can be thread through a 19-gauge needle allows sampling of the cyst wall. These enhanced biopsy techniques have increased the quality and quantity of tissue, improving definitive and specific diagnoses of pancreatic lesions.
Suspicious pancreatic and extrapancreatic biliary lesions can be sampled by brushing the pancreatic and common bile ducts , which is particularly useful when there is a duct stricture without a discernible mass. Brushings are obtained endoscopically, sometimes in conjunction with endoscopic retrograde cholangiopancreatography; they can also be obtained during percutaneous transhepatic cholangiography. Because pancreatic ductal adenocarcinoma tends to invade the main pancreatic or common bile ducts, this sampling method is highly effective. Brushings can also diagnose an accessible cholangiocarcinoma and hepatocellular carcinoma.
The most common major complication of FNA is acute pancreatitis, with an incidence of 1% to 3%; mortality is less common. Other, rare major complications include pancreatic duct leaks, massive hemorrhage, and septic shock. Perforation associated with a malignant luminal stenosis is a specific complication of EUS-guided FNA. EUS-FNA is safe, and aspiration needle tract seeding by tumor cells or mucin is exceedingly rare. Complications of bile duct brushing are minor and include cholangitis and mild pancreatitis.
Rapid on-site evaluation (ROSE) of the specimen by a cytologist provides feedback to the operator on the adequacy of individual passes, allowing the operator to obtain additional passes until the sample is judged adequate. It has potential utility with solid masses, where some have found that ROSE reduces the rate of nondiagnostic results ; others have questioned its value when experienced operators perform the procedure, finding no difference in nondiagnostic rates with and without ROSE. The more recent addition of core needle biopsy to EUS-FNA has decreased the need for ROSE. ROSE offers little benefit with cysts because smearing a small drop of cyst fluid results in a paucicellular sample poorly suited for rapid examination.
Aspirates and brushings can be prepared as smears, a liquid-based preparation (e.g., ThinPrep, SurePath), a CytoSpin, a cell block, or some combination. If smears are used, proper smear technique is vitally important; even the most cellular sample is useless if the cells cannot be evaluated due to a preparation-related artifact. Clotted tissue (“worms”) should be gently lifted from the glass slides and placed into formalin for a cell block. (Small formalin vials such as those used for bone marrow cores are recommended.) Smears can be air-dried and Romanowsky-stained or alcohol-fixed and Papanicolaou-stained, depending on the preference of the laboratory.
Bile duct brushings are best prepared by a liquid-based method (e.g., ThinPrep, SurePath), cytocentrifugation (i.e., CytoSpin), or cell block because a liquid collection method, used by all these methods, allows for less mechanical artifact when dislodging the cells from the brush. Furthermore, the residual liquid-based sample can provide cells for fluorescence in situ hybridization (FISH) or genetic sequencing.
A cell block from the sedimented fluid can be invaluable for immunohistochemical and molecular studies. An aliquot for microbiologic cultures or flow cytometry might be considered based on the on-site evaluation findings.
Biochemical and molecular analysis can help in classifying cyst fluids ( Table 14.1 ). For this reason, fresh, unfixed cyst fluid is often apportioned among cytology, biochemical, and molecular studies to establish whether the cyst is mucinous and, if so, whether it is malignant. The gross finding of a thick, viscous, white fluid; cytologic evidence of colloid-like extracellular mucin; and an elevated carcinoembryonic antigen (CEA) level all support a mucinous cyst. Cytomorphologic assessment, however, is required to establish malignancy. The two most useful biochemical tests are CEA and amylase (see Table 14.1 ). Because CEA levels can be low in mucinous neoplasms, KRAS molecular testing is helpful, but it adds no value if CEA is elevated, which by itself supports a mucinous cyst (with only rare exceptions). GNAS mutations are seen in intraductal papillary mucinous neoplasms (IPMN) but not mucinous cystic neoplasms (MCN). For this reason, finding a GNAS mutation may add value by identifying an IPMN and distinguishing it from a MCN, given that the latter is resected irrespective of grade. The presence of a KRAS or GNAS mutation does not distinguish benign from malignant neoplasms. Late mutations in the adenoma to carcinoma progression, such as TP53 mutation or deletion of SMAD4 or p16/CDKN2A, lend support to the interpretation of a cyst at high-risk for malignancy.
| Cyst | CEA | Amylase | Genetic Alterations |
|---|---|---|---|
| Pseudocyst | ↓ | ↑↑ | None |
| Lymphoepithelial cyst | ↑ | ↓ | None |
| Serous cystadenoma | ↓ | ↓ | 3p25 deletion |
| Intraductal papillary mucinous neoplasm | ↑↓ | ↑ | KRAS, GNAS ( p53, SMAD4, or p16 supports HR cyst) |
| Mucinous cystic neoplasm | ↑↓ | ↓↑ | KRAS ( p53, SMAD4, or p16 supports HR cyst) |
To best guide patient management, the cytologic diagnosis should be correlated with clinical findings and radiologic and ancillary laboratory test results. Given the technical challenges in obtaining an adequate sample and the cytomorphologic interpretive challenges, the sensitivity of EUS-FNA of the pancreas is variable, averaging 80%. Specificity ranges from 60% to 100%. Sensitivity improves with increasing technical expertise. Diagnostic accuracy for solid pancreatic masses is greater than 90% but lower for cystic lesions.
Brush cytology has almost 100% specificity but only about 50% sensitivity because of false-negatives due to sampling and interpretation. Indeterminate (i.e., atypical or suspicious) interpretations result not only from preparation artifact but also from the high threshold needed for an unequivocal malignant interpretation, given that marked atypia on brush cytology is often associated with an inflamed or stented duct.
The terminology recommended by the Papanicolaou Society of Cytopathology (PSC) is shown in Table 14.2 . This classification has six major categories that include a “Neoplastic” category that is divided into benign and “other” (premalignant and low-grade malignant) neoplasms.
|
A negative for malignancy sample is one that contains adequate cellular or extracellular tissue to define a nonneoplastic lesion identified on imaging. An atypical diagnosis reflects a mild degree of cytologic atypia, often in the setting of inflammation, prior duct instrumentation, or sparse cellularity. A bile duct brushing with mucinous or papillary epithelium suggestive of intraductal neoplasia is interpreted as atypical rather than “Neoplastic: Other.” Additionally, aspirates with insufficient tissue for a definitive diagnosis of a neuroendocrine tumor (NET) or a solid-pseudopapillary neoplasm (SPN) are interpreted as atypical rather than suspicious for malignancy. (“Atypical” is to “Neoplastic: Other” as “Suspicious” is to “Malignant.”) The neoplastic category is divided into benign neoplasms ( Neoplastic: Benign ), comprised mostly of serous cystadenoma, and premalignant and low-grade malignant neoplasms ( Neoplastic: Other ), which includes IPMN, MCN, NET, and SPN. A suspicious interpretation implies a strong concern for malignancy, usually for ductal adenocarcinoma, but a definitive interpretation is not possible, usually because the cytologic features are quantitatively or qualitatively insufficient. A second opinion can be helpful before issuing a report in such cases; without a definitive diagnosis, an additional procedure might be needed. Aspirates insufficient for a definitive diagnosis of a high-grade, aggressive malignancy such as ductal adenocarcinoma or acinar cell carcinoma are interpreted as suspicious. A positive interpretation indicates that the cytologic features meet the criteria for the diagnosis of a malignancy of some type, most commonly ductal adenocarcinoma. A nondiagnostic specimen is one that provides no useful information about the lesion sampled. Any cellular atypia precludes a nondiagnostic report.
The pancreas is rich in parenchyma and poor in stroma. Exocrine acinar tissue is arranged in lobules around a ductal system that increases in caliber as it progresses toward the ampulla. Acinar cells secrete digestive enzymes into this excretory ductal system, which is lined by epithelium that progressively increases in size from cuboidal (in the smaller intralobular ducts) to tall columnar cells (in the larger interlobular ducts). The epithelial cells lining the pancreatic ductal system are generally nonmucinous, although goblet cells are occasionally noted in the main pancreatic duct. Mucinous differentiation, therefore, is evidence of pancreatic intraepithelial neoplasia. Loose connective tissue separates the lobules and a zone of connective tissue surrounds the ducts and islets.
Cohesive, grape-like aggregates, isolated and attached to fibrovascular stroma
Few stripped naked nuclei and isolated cells
Eccentrically placed, round nucleus
Evenly distributed, finely granular chromatin
Small nucleolus; larger in reactive acinar cells
Abundant granular cytoplasm
Indistinct cell borders in clusters
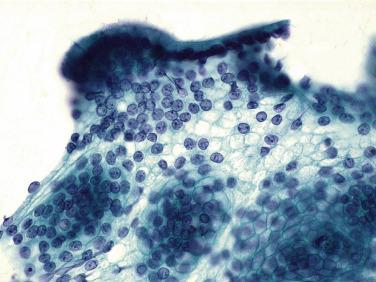
Acinar cells are normally arranged in small rounded (“grape -like”) groups (acini) with a small lumen. They are polygonal, with ample dense, blue-green cytoplasm when seen with a Papanicolaou stain ( Fig. 14.2A ) and punctate and purple with a Romanowsky stain. Nuclei are round, with finely textured, evenly distributed chromatin and a small nucleolus that enlarges markedly with reactive changes. Nucleoli help to distinguish naked acinar cell nuclei from lymphocytes.
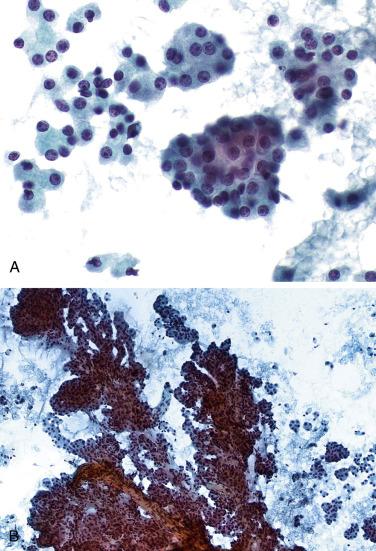
Aspirates of benign pancreatic tissue are often very cellular, which can result in a mistaken impression of a neoplasm. Isolated acini (“grapes”) and clusters of acini attached to fibrovascular tissue (“grapes on a vine”) ( Fig. 14.2B ) are characteristic of benign pancreatic acinar tissue. Isolated cells are also present, but they are less prominent than in acinar cell carcinoma.
Flat, cohesive sheets (few isolated cells)
Even nuclear spacing within sheets
Round to oval nucleus
Evenly distributed, finely granular chromatin
Inconspicuous nucleolus
Well-defined cytoplasmic borders
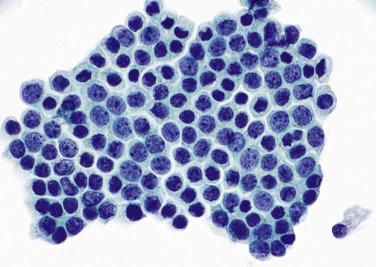
An FNA of normal pancreas displays fewer ductal cells than acinar cells, whereas pancreatic and bile duct brushings consist mostly of ductal cells, and acinar cells are absent. Ductal cells are cuboidal or columnar and usually arranged as monolayer sheets or strips of cells with a luminal edge of non-mucinous cytoplasm. Monolayer sheets have a uniform, lattice-like (“honeycomb”) appearance, with evenly spaced round, regular nuclei and well-defined cytoplasmic borders ( Fig. 14.3 ). Nuclei have evenly distributed, finely granular chromatin and inconspicuous nucleoli that enlarge significantly in reactive conditions. The cytoplasm varies in amount from scant to moderate and is dense and nonmucinous with routine stains. Any visible cytoplasmic mucin is pathologic; overtly mucinous ductal cells from the pancreas represent either pancreatic intraepithelial neoplasia or ductal adenocarcinoma. With liquid-based preparations, nuclei of benign ductal cells may appear crenated, a common artifact that is easily recognized with experience. Normal islet cells are rarely identified because of their relative paucity and fragility.
The pancreas is nestled in the retroperitoneum, with its head surrounded by the second portion of the duodenum. It is close to the liver, transverse colon, stomach, spleen, and both kidneys; thus it is not unusual for a CT-guided needle to procure normal tissue elements from adjacent organs on its way to the pancreas. Mesothelial cells, hepatocytes, and renal tubular cells are occasionally encountered. Mesothelial cells resemble benign ductal cells; they have a similar flat, monolayer sheet-like arrangement. Because they are relatively large cells that vary in size, they are prone to misinterpretation as adenocarcinoma. Recognizing the characteristic slit-like spaces (“windows”) between adjacent mesothelial cells helps identify them as such.
Flat, cohesive monolayer sheets with a honeycomb pattern; occasionally papillary groups (intact villi), smaller groups, isolated cells
Nonmucinous glandular cells with brush border
Sporadically placed goblet cells appear as “fried eggs” within the sheet
Lymphocytes (“sesame seeds”) in the epithelium
Small sheets and strips; occasional isolated cells and gastric pits
Visible mucin (foveolar cells)
Grooved naked nuclei
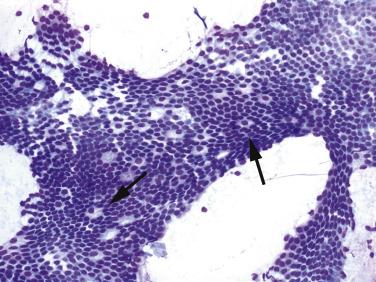
With EUS-FNA, cells from the stomach or duodenum are ever-present contaminants. Both duodenal and gastric epithelial cells appear as flat, monolayer sheets with a honeycomb pattern. Duodenal enterocytes are nonmucinous epithelial cells in large sheets studded with goblet cells, which have the appearance of a fried egg on alcohol-fixed preparations because the centrally placed goblet cell nucleus is surrounded by a clear halo ( Fig. 14.4 ). Intraepithelial lymphocytes (“sesame seeds”) are sprinkled among the enterocytes. Because most branch-duct IPMNs are lined by gastric-foveolar type cells, the absence of visible mucin and the presence of intraepithelial lymphocytes and a brush border help identify the fragment as duodenal in origin.
Gastric surface foveolar cells appear as sheets of cells with mucinous cytoplasm; larger groups contain intact crypts ( Fig. 14.5 ). Stripped naked nuclei with grooves are also seen. The distinction from low-grade neoplastic mucinous epithelium, particularly that seen in branch-duct cysts that are typically lined by gastric-foveolar type cells, is virtually impossible. A specimen consisting exclusively of epithelial contaminants should be interpreted as nondiagnostic; misinterpreting epithelial contaminants as a benign lesion can result in a false-negative interpretation. It is often unclear, however, whether the cells are lesional or contamination. In this circumstance, if there is no supporting evidence for a mucinous cyst (e.g., thick colloid-like mucin or an elevated CEA level, classifying it as Neoplastic: Other ), then negative for malignancy is a reasonable interpretation, with the descriptor “nonspecific cyst fluid without high-grade epithelial atypia.” Although nonspecific, it provides important information about the absence of high-risk cytology, which may be sufficient for patient care when, for example, imaging features support the diagnosis of a branch duct cyst.
Gastrointestinal epithelium is readily distinguished from high-grade adenocarcinoma and high-grade dysplasia of mucinous cysts. Reactive pancreatic ductal cells with atypia, however, resemble adenocarcinoma and can lead to a false-positive interpretation, but the cells are usually few in number, which should prompt caution in interpretation (see following section).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here