Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
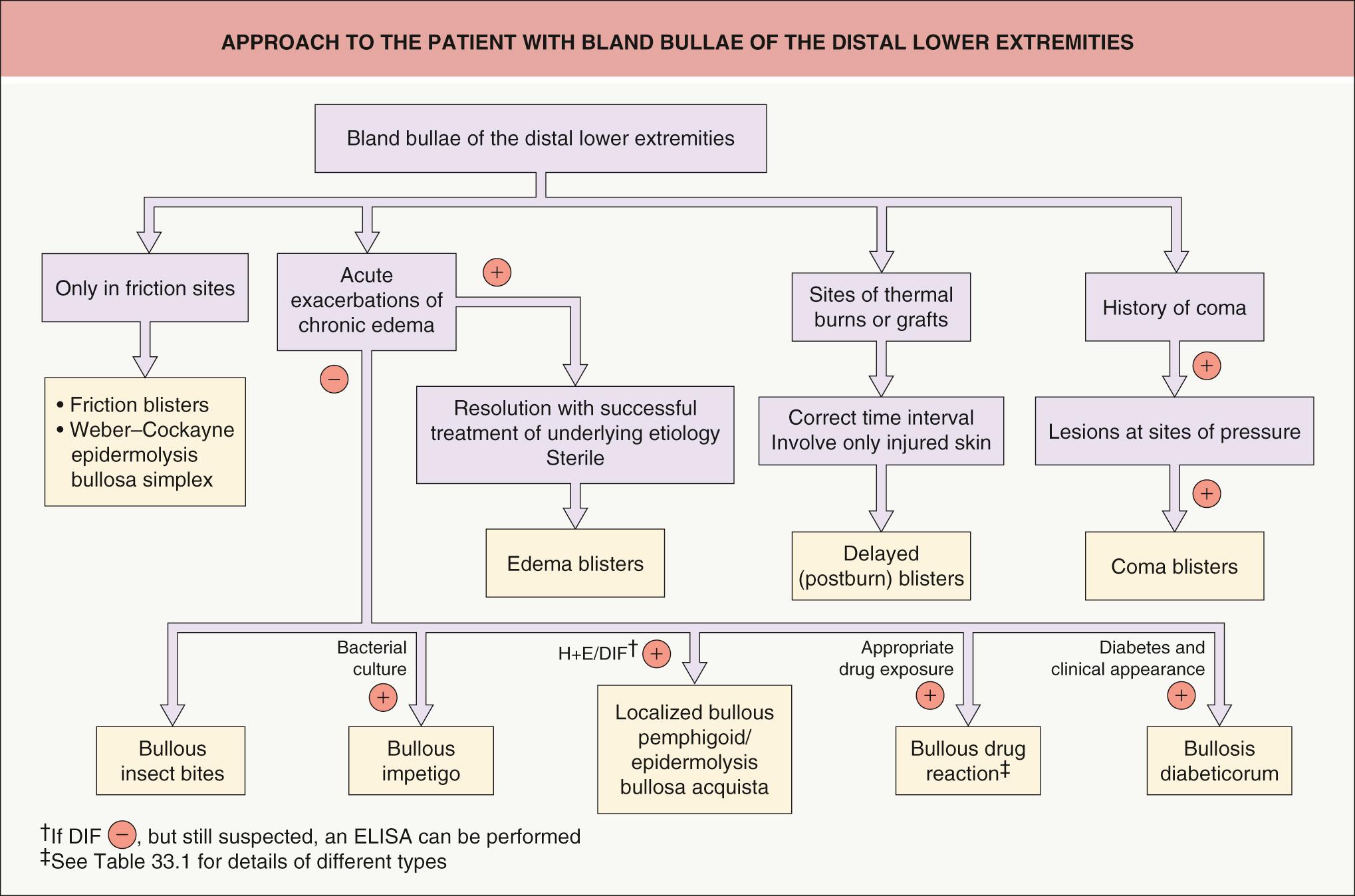
Vesiculobullous diseases of the skin encompass a wide range of entities, including autoimmune bullous diseases and inherited blistering disorders (see 28, 29, 30, 31, 32 ). This chapter focuses on the remaining non-infectious disorders in which cutaneous bullae develop and represent the primary clinical manifestation.
▪ Diabetic bullae ▪ Bullous eruption of diabetes mellitus
A rare condition associated with diabetes mellitus
Tense blisters develop on normal-appearing skin in acral sites (feet, lower legs, hands); there is often an association with peripheral neuropathy
Histologically, intraepidermal and/or subepidermal blisters are observed
Spontaneous healing usually occurs in 2 to 6 weeks
Bullosis diabeticorum was first described by Kramer in 1930. In 1967, Cantwell & Martz introduced the term ‘bullosis diabeticorum’.
The exact prevalence of bullosis diabeticorum is unknown. In a retrospective study of diabetic patients, the annual incidence was 0.16% . The age of onset ranges from 17 to 84 years, with a mean age of 55 years. A 2 : 1 male-to-female ratio has been reported, and it occurs more frequently in the setting of long-standing diabetes and neuropathy.
Although bullosis diabeticorum has been related to trauma and the microangiopathy of diabetes, little is known about its cause. Diabetic patients can develop blisters after minimal trauma, and some authors have found a reduced threshold for inducing suction blisters in these patients . There is no evidence of an infectious etiology.
Bullosis diabeticorum is characterized by a sudden and spontaneous appearance of vesicles and bullae within normal-appearing, non-inflamed skin of the distal extremities of diabetics. The most frequent locations (in decreasing order) are the feet, distal legs, hands, and forearms. Bullae are rarely seen on the trunk. The lesions are usually asymptomatic, but occasionally there is a mild burning sensation. Blisters often develop “overnight” and in the absence of known trauma. The vesicles and bullae are tense and vary in diameter from 0.5 to several centimeters ( Fig. 33.1 ). They contain a clear, sterile fluid that can be more viscous than that found in friction blisters.

Most patients have longstanding diabetes, but occasionally bullosis diabeticorum is a presenting sign of diabetes. It is associated with both insulin-dependent and non-insulin-dependent diabetes mellitus. Many patients have an associated polyneuropathy, retinopathy or nephropathy.
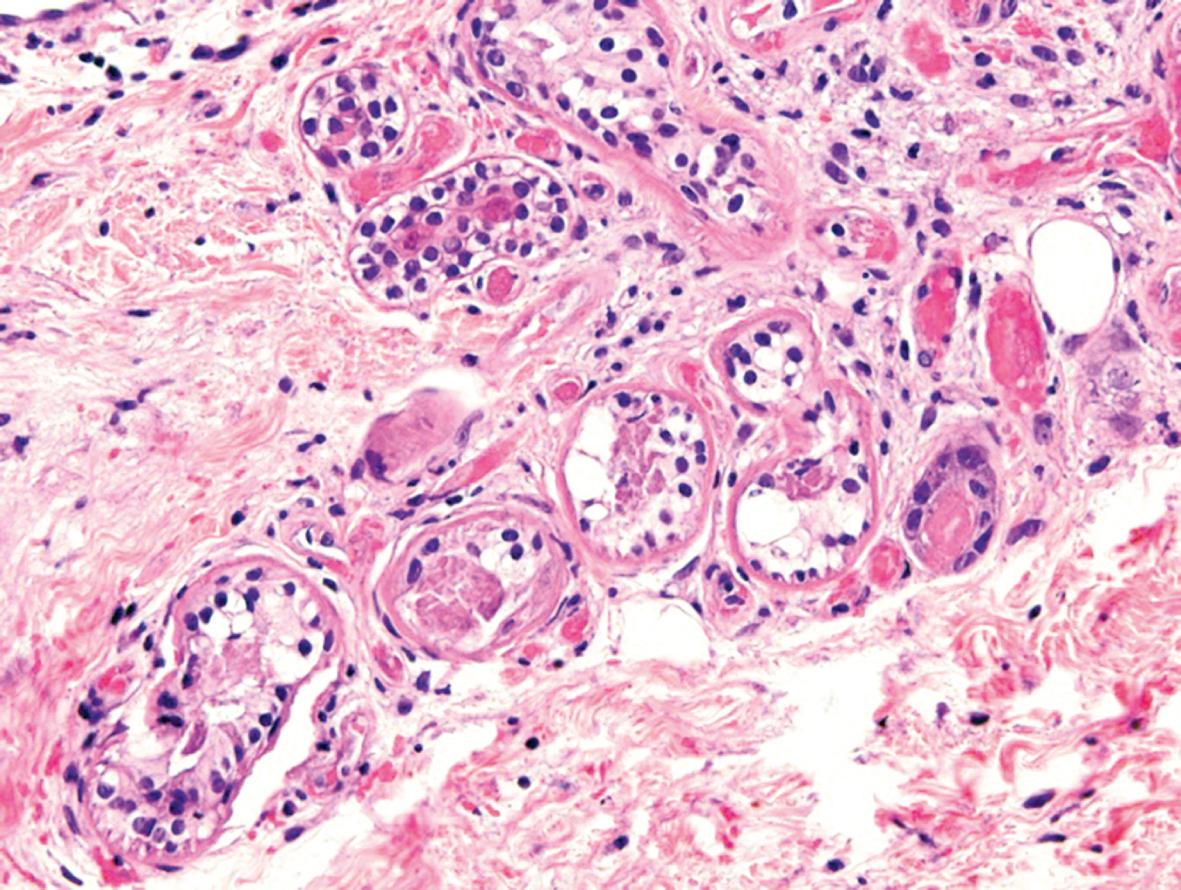
The histologic findings are heterogeneous. Initial reports described intraepidermal blisters, whereas recent publications have usually described subepidermal bullae. It has been suggested that the level of cleavage is subepidermal, and that intraepidermal blisters represent older lesions undergoing re-epithelialization. Direct immunofluorescence (DIF) examination is usually negative, although one report described IgM and C3 deposits within dermal blood vessel walls. By electron microscopy, subepidermal blisters with a separation at the level of the lamina lucida or below the lamina densa have been described .
In porphyria cutanea tarda (PCT) and pseudoporphyria associated with dialysis and medications, the blisters are usually <1 cm in diameter and favor the hands rather than the feet and ankles. Complications of diabetes include both chronic renal failure and atherosclerotic cardiovascular disease and, as a result, patients may be receiving dialysis and/or diuretics. The distal extremity is also a common site for fixed drug eruptions, but the bullae develop on an inflammatory base. Localized bullous pemphigoid and epidermolysis bullosa acquisita (EBA) are differentiated by histologic examination and DIF, as well as by an accentuation of lesions at sites of friction in patients with EBA. If there is surrounding erythema, warmth and tenderness, the possibility of bullous cellulitis must be considered.
Most patients have spontaneous healing of their lesions within 2 to 6 weeks. Treatment focuses on aspiration of blisters or placement of a small window in the blister roof and application of topical antiseptics or antibiotics to reduce discomfort and prevent secondary infections, respectively. Occasionally, a secondary soft tissue infection does develop, requiring systemic antibiotics or surgical intervention .
▪ Coma bullae ▪ Drug-induced coma blisters ▪ Barbiturate blisters ▪ Neurologic blisters
Associated with loss of consciousness, neurologic diseases, or prolonged immobilization
Tense blisters develop on normal-appearing skin
Histologically, intraepidermal or subepidermal blisters are observed, with a characteristic necrosis of sweat glands
Spontaneous healing occurs within 1 to 2 weeks
In some comatose patients, blisters will develop within 48–72 hours of loss of consciousness, primarily at pressure sites. Although classically associated with barbiturate overdose, they can be seen in the setting of coma due to other medications (e.g. opioids), infections (e.g. viral encephalitis), metabolic disturbances (e.g. hypoglycemia), and neurologic dysfunction (e.g. cerebrovascular accidents).
Coma blisters were first described in 1806 by Dominique Larrey, Napoleon's surgeon, who noticed these lesions in soldiers who had been comatose from carbon monoxide intoxication.
In 1952, Holten reported the appearance of coma blisters in 4% of a series of 501 patients with barbiturate poisonings . In another study, blisters were found in 6.5% of barbiturate overdoses . Although most reported cases have been associated with barbiturate overdose, blisters have also been observed in those whose comas were induced by overdosage of other medications, such as benzodiazepines, tricyclic antidepressants, opioids, hypnotics or antipsychotics, as well as alcohol intoxication . Similar lesions have also been described in patients with non-drug-induced coma, i.e. coma resulting from carbon monoxide poisoning, head trauma, cerebrovascular accidents, viral encephalitis, hypoglycemia, diabetic ketoacidosis, or hepatic encephalopathy . In addition, bullous lesions have been observed following surgical procedures requiring general anesthesia and in non-comatose patients, in particular those with severe neurologic disease or prolonged immobilization (e.g. secondary to accidents) .
The pathogenesis is unclear. A direct toxic drug effect has been implicated, particularly because of the association with drug intoxication and the frequent finding of eccrine gland necrosis (many drugs are thought to be excreted by sweat glands). However, this would not explain the non-drug-induced cases. Therefore, pressure, friction, and local hypoxia have been implicated as etiologic factors. The pressure/ischemic hypothesis is currently favored and is supported by the observation that most (if not all) lesions appear at sites of pressure.
Lesions develop at body sites exposed to maximum pressure during unconsciousness or immobilization. They first appear 24 hours after the onset of coma as blanchable erythematous patches or plaques that progress to violaceous plaques. Blisters or erosions then develop within 48–72 hours after the onset of coma at these sites ( Fig. 33.2 ). If the patient survives, the erosions usually heal spontaneously over 1 to 2 weeks. In some individuals, residual scarring can result. Compression neuropathies and non-traumatic rhabdomyolysis are additional complications seen in patients with coma bullae . As mentioned previously, the same type of blisters can occur in patients with prolonged immobilization or neurologic diseases ( Fig. 33.3 ).


The blisters are predominantly subepidermal. However, intraepidermal blisters are also observed as the result of re-epithelialization of older lesions or epidermal spongiosis. There is a variable degree of epidermal necrosis. Sweat gland necrosis is a characteristic finding ( Fig. 33.4 ), and focal necrosis of the epithelium of the pilosebaceous follicles can also be seen. There is only a sparse inflammatory cell infiltrate. DIF is usually negative, but deposits of IgG, IgM and/or C3 have been found within the walls of dermal blood vessels .
In most patients, the clinical setting alone is sufficient to make the diagnosis ( Fig. 33.5 ). A cutaneous biopsy will allow differentiation from friction blisters. An intraepidermal blister cavity just below the granular layer is seen in friction blisters, whereas a subepidermal split with sweat gland/follicular necrosis is characteristic of coma bullae. Based upon the distribution pattern, clinical appearance and histologic findings, multiple fixed drug eruption can be excluded.
Coma blisters heal spontaneously over 1 to 2 weeks. In non-comatose patients, frequent postural changes help to resolve and prevent the disorder.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here