Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The term “orthognathic” stems from the Greek words ortho , which is to straighten, and gnathic , which describes the jaw. Orthognathic surgery is a subspecialty practiced by numerous disciplines, including oral and maxillofacial, plastic and reconstructive, and ear, nose, and throat surgeons. It is defined as osteotomies performed to the midface and mandible to reposition the tooth-bearing bony segments.
The concept of orthognathic surgery has its roots in rural America, with a long and storied history beginning in the mid-1800s. After its inception, the subspecialty progressed in waves prior to and after the World Wars of the 20th century, as many surgeons developed new management strategies to care for wounded veterans. The field of craniofacial surgery was also involved to a lesser extent with orthognathic procedures, comprising the work of Gillies and Tessier in the mid-20th century. – Without a doubt their approaches and techniques provided vital insight to the management of jaw deformities.
Modern orthognathic surgery is said to have been rooted in Europe in the 1950s, led by Hugo Obwegeser. He went on to publish his techniques for the intraoral sagittal split osteotomy in 1955, followed by an extensive case series on Le Fort I osteotomies in 1969 and then his experience with concurrent bimaxillary surgery in 1970. , Obwegeser brought his techniques to the USA in the 1960s. In 1969, American plastic surgeon John Marquise Converse published numerous works with an orthodontist named Horowitz, further highlighting the importance of collaboration between the surgical and dental fields.
American oral surgeons, who had recently separated from plastic surgery in the period following World War II, latched onto orthognathic surgery and began making further strides. The first known textbook dedicated to orthognathic surgery was written by oral surgeons Hines and Kent in 1972, followed by numerous other texts that focused on corrective jaw surgery in the 1980s by the likes of Bell, Profitt, White, and Epker, to name a few. Modern day advancements have continued within the subspecialty, led by both oral and plastic surgeons. Additional developments and clinical evolution has further advanced orthognathic surgery to a procedure with less morbidity, greater predictability, and is safe and reliable.
A certain understanding of dental terminology is necessary in order to completely understand the concepts surrounding orthognathic surgery, as well as to communicate treatment plans efficiently and appropriately with orthodontic and other dental colleagues.
Beginning with the tooth, it is composed of various structures. The neurovascular component of it enters at the apex, an opening at the inferior portion of the tooth. These structures culminate at the dental pulp, which is surrounded by dentin. The dentin is subsequently encased by cementum, the outer tooth structure that provides attachments to the surrounding periodontal ligament and associated alveolar bone. Visible clinically, the enamel covers the superior portion of the dentin. The portion of the tooth including the enamel and dentin is considered the crown of the tooth, whereas the root of the tooth is comprised of the cementum, dentin, pulp tissue, and associated soft tissue attachments to the surrounding bone. The complete adult human dentition is composed of 32 teeth, 16 per jaw: 2 central incisors, 2 lateral incisors, 2 canines, 4 premolars, and 6 molars. The pediatric or deciduous dentition includes 20 teeth, 10 per jaw: 2 central incisors, 2 lateral incisors, 2 canines, and 4 molars.
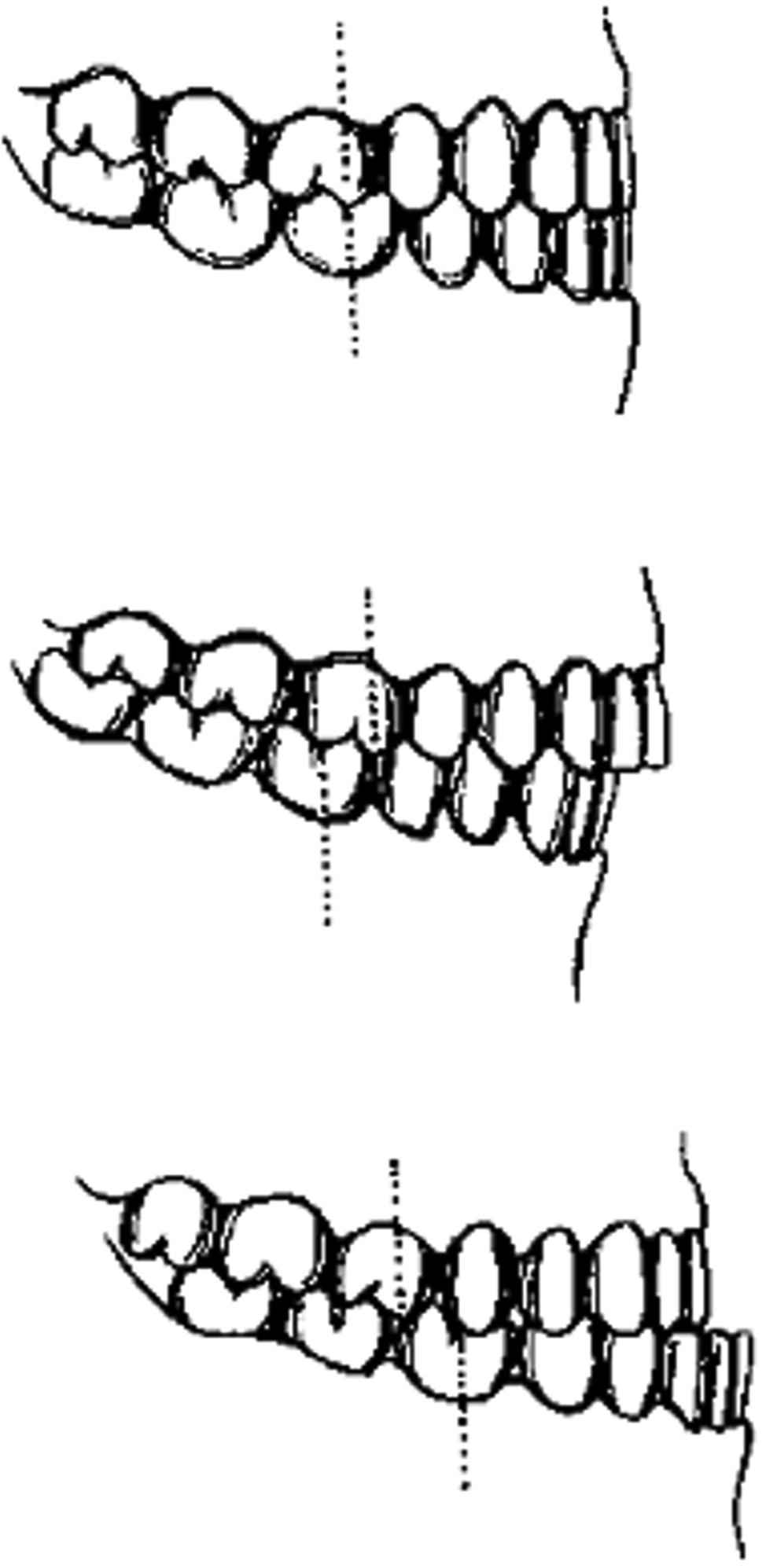
Directionality within the mouth and relative to the teeth also uses a different nomenclature. Rather than anterior, posterior, medial, and lateral, the cardinal directions when discussing teeth include mesial (toward the dental midline), distal (away from the dental midline), lingual or palatal (toward the tongue or palate, relative to teeth on the mandible or maxilla, respectively), and buccal/labial (toward the soft tissue of the cheek and lip, respectively). The dental midline is that between the maxillary and mandibular central incisors ( Fig. 21.1 ).

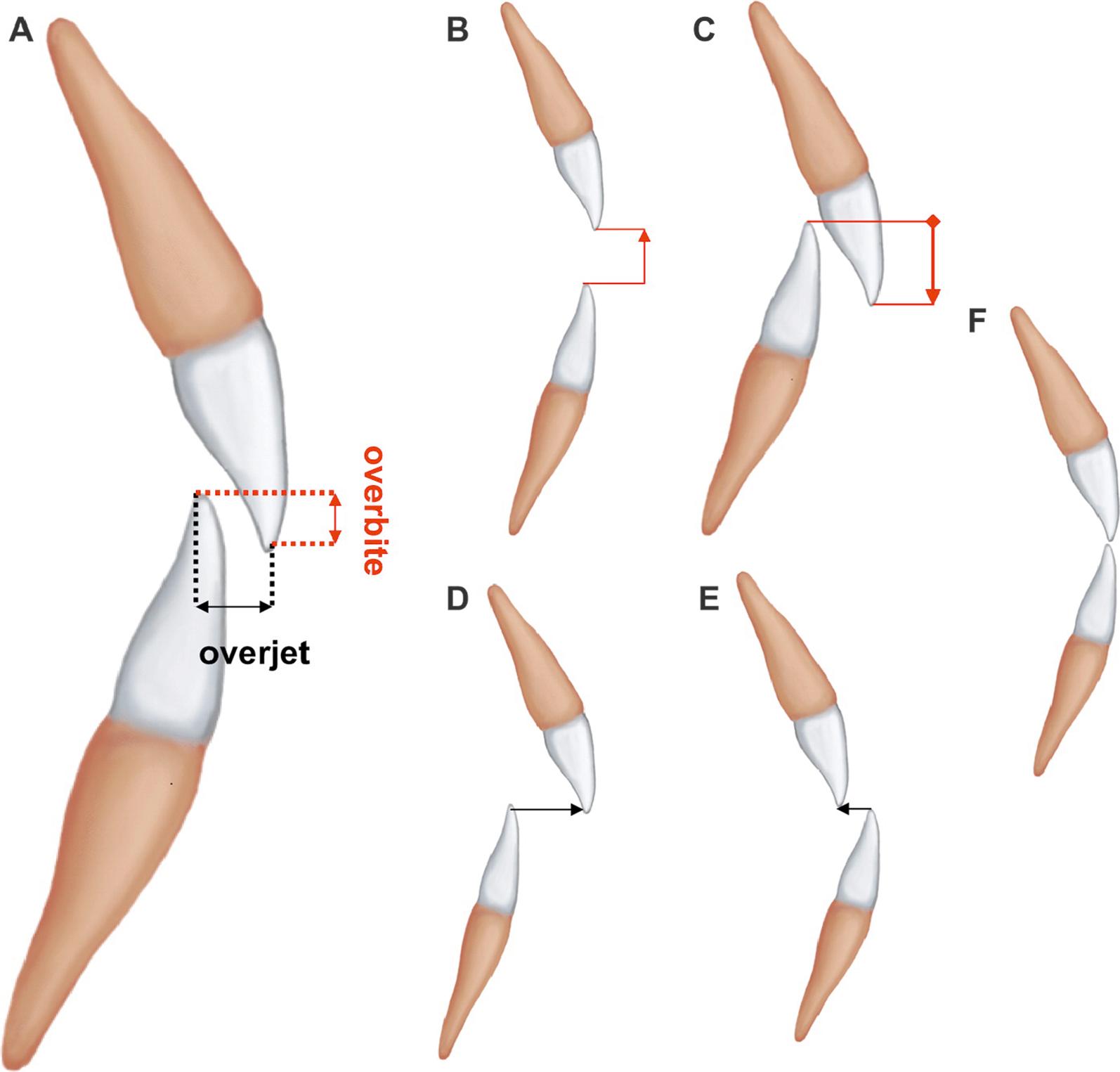
Dental relationships between the maxilla and mandible are also described in an organized fashion. The normal relationship of the maxillary to the mandibular teeth should include a slight buccal and labial displacement, with the lingual cusps of the maxillary teeth interposing with the buccal cusps of the mandibular teeth. A class I molar relationship is considered normal, and this is when the mesiobuccal cusp of the first maxillary molar is in occlusion with the buccal groove of the first mandibular molar. When this relationship is altered, and the maxillary molar is positioned mesially, this is termed class II occlusion, and when distally, is considered class III ( Fig. 21.2 ). There should be approximately 2 mm of overlap with the maxillary to the mandibular incisors in both the anteroposterior and vertical planes, termed overjet and overbite ( Fig. 21.3 ). When these relationships are reversed, the term crossbite is used, and it can be relative to an anterior or posterior location of the offending dentition. A crossbite can also be dental, skeletal, or a combination of both. This is relative to the position of the alveolar processes being centered over each other (skeletal) or the location of the teeth within these dental arches (dental). Also, crossbite can occur in a functional manner, whereas it is normal at rest and manifests with mastication.
An open bite, also termed apertognathia, is when teeth are not meeting along the occlusal plane. This can occur anteriorly, posteriorly, uni- or bilaterally. In certain occasions, often when the involved teeth are overly flared or impacted, these open bites can be corrected orthodontically. Oftentimes, though, this dental relationship is secondary to a skeletal abnormality, and must be corrected with a surgical intervention. It is important to note that when teeth are not meeting in occlusion, they will continue to over-erupt via appositional bone growth within the associated dental alveolus.
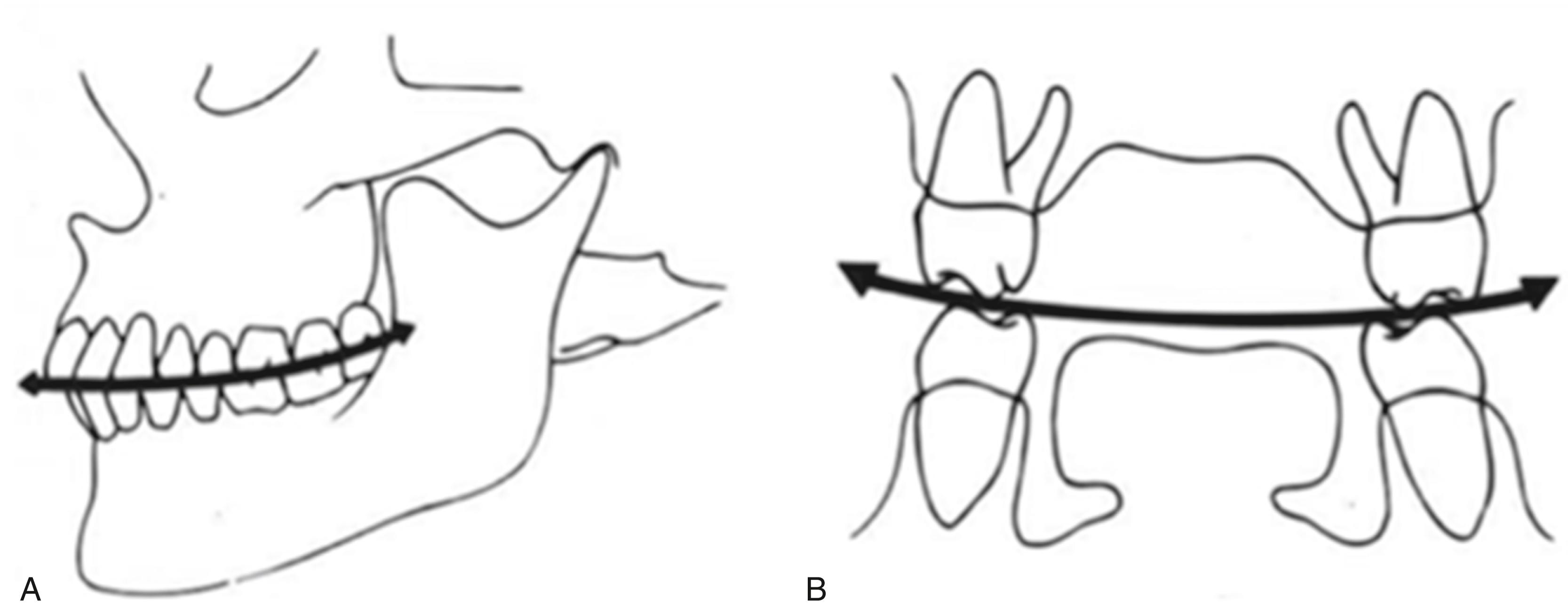
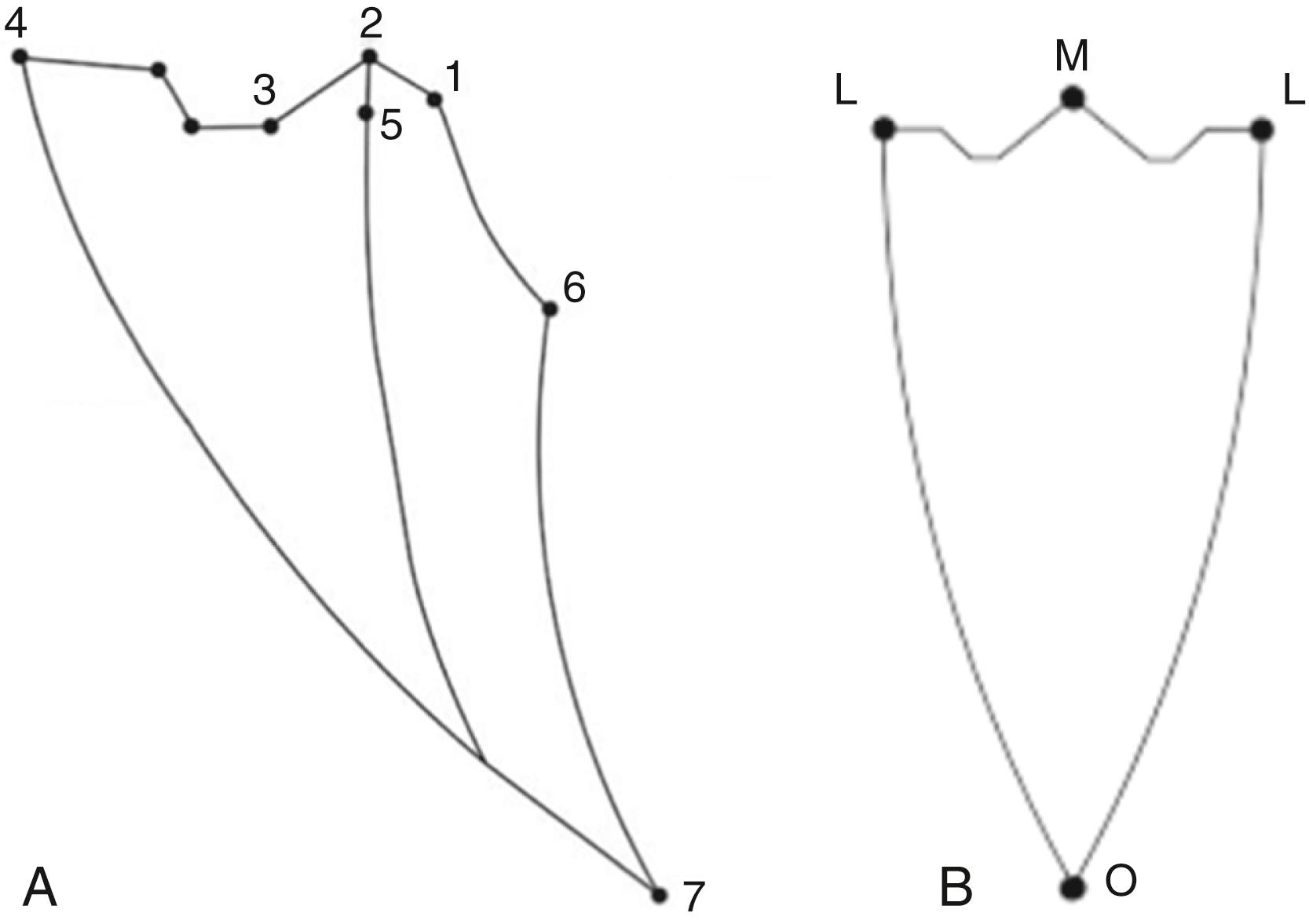
Another way to study the maxillary and mandibular dental relationships is to view them in both the sagittal and coronal planes. In the sagittal plane, the teeth should follow a gentle arc connecting from the mandibular condyle through the occlusal plane. This is referred to as the curve of Spee. In the coronal plane, a similar gentle arc can be drawn relative to the occlusal relationship created by the buccal inclination of the maxillary teeth with the lingual inclination of the mandibular teeth. This arc is termed the curve of Wilson ( Fig. 21.4 ).
Lastly, there exist specific associations between the mandible and maxilla that also involve positioning within the temporomandibular joint. One such relationship is called centric relation. Centric relation is the reproducible maxillomandibular relationship whereby the mandibular condyles are seated within the anterior- and superior-most position of the glenoid fossa. It is independent of tooth contact. Centric occlusion, on the other hand, is the first tooth contact when in centric relation. Maximal intercuspation is the contact between the maxillary and mandibular dentition, independent of condylar position, and it may or may not coincide with centric occlusion. This terminology is demonstrated on Poselts diagram ( Fig. 21.5 ).
The evaluation of a patient who is appropriate for orthognathic surgery should always follow in a stepwise approach. There are two main reasons as to why a patient may be considering such a procedure, mostly to correct a functional or cosmetic abnormality. Functional issues can further be categorized based on dental malocclusion, masticatory difficulty, or an upper airway abnormality. Cosmetic abnormalities involve malposition of the maxilla or mandible causing facial disharmony and/or asymmetry.
Beginning with an overall appreciation of the facial form, the surgeon can view the face in the frontal plane by way of the vertical fifths. As such, the face is divided into fifths corresponding with the distance from medial canthus to medial canthus, medial canthus to lateral canthus (each side, respectively), and lateral canthus to helix of the ear (also, respective to each side of the face). These fifths should be equal. To further evaluate these measures, the distance between the medial canthi should coincide with the alar base, and the nasal dorsum width should be half of this value. The angle of the mouth should fall in line with the medial limbus of the eye, and the lateral canthus should coincide with the gonial angle. In the lateral view, the face can then be divided into horizontal thirds. The upper third is measured from trichion to glabella, middle third is glabella to subnasale, and lower third is subnasale to pogonion. These thirds should be equal. The lower third can further be subdivided into an upper third from subnasale to labii superioris, and a lower two-thirds from labii inferioris to pogonion ( Fig. 21.6 ).
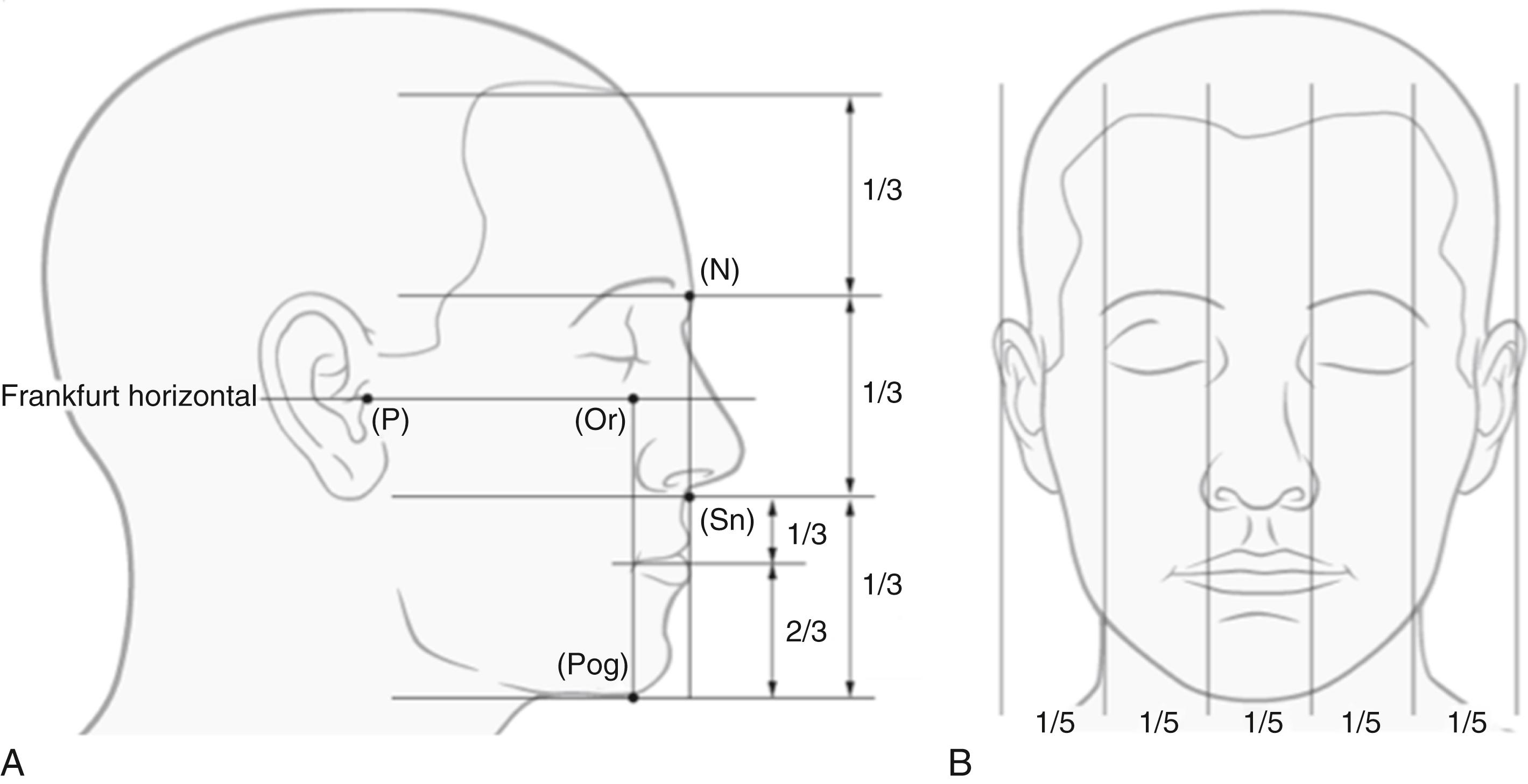
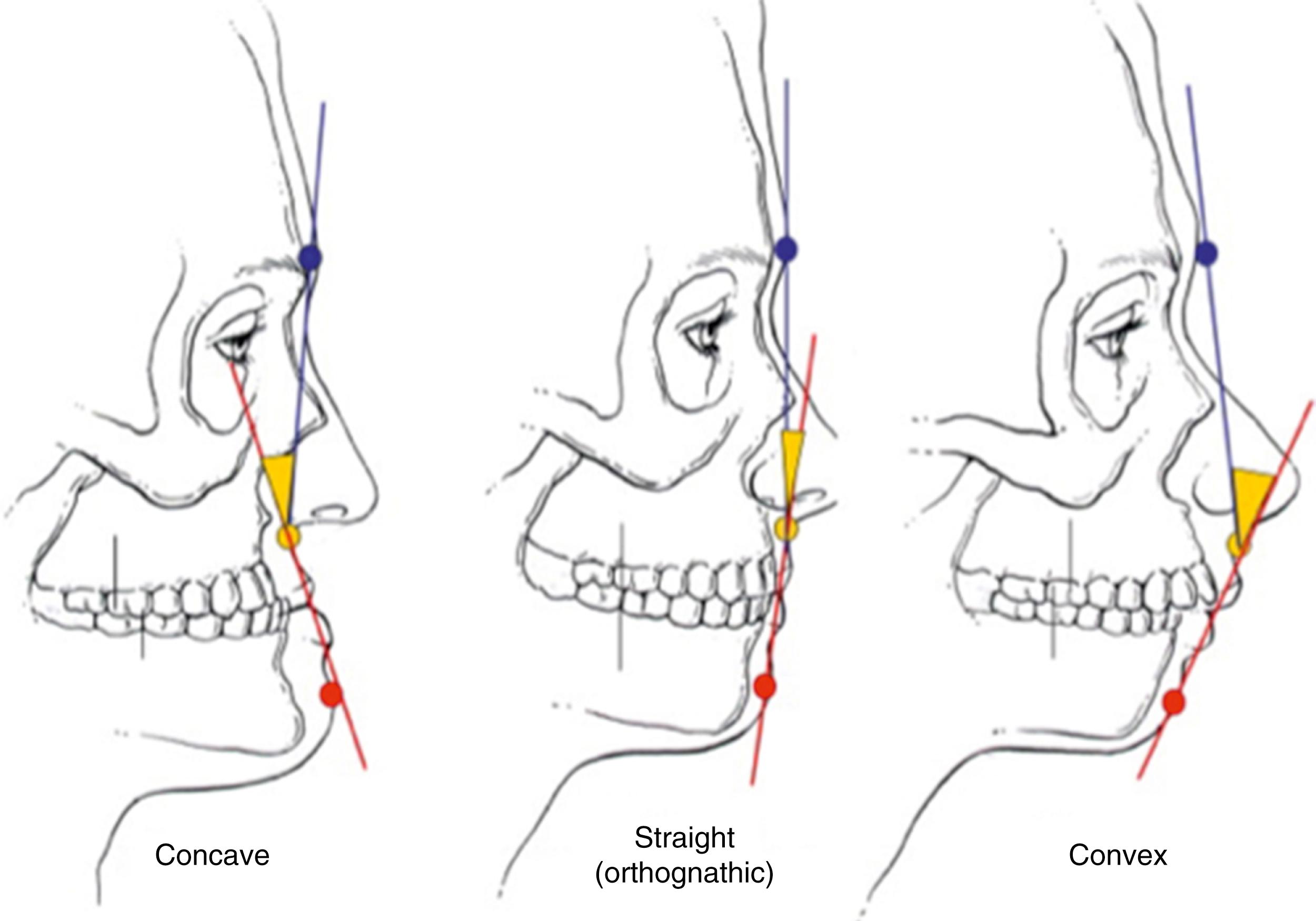
Skeletal profiles are studied by evaluating the patient in the lateral view. A class I skeletal profile is considered the norm, with a slightly convex profile and a smooth transition from upper to middle to lower facial thirds. A class II skeletal profile is overly convex, whereas a class III profile is concave. Reasons for a class II profile can be due to a hyperplastic maxilla, or hypoplastic mandible, and a class III profile may be due to a hypoplastic maxilla or hyperplastic mandible ( Fig. 21.7 ).
Individual measurements should be documented in the initial preoperative planning period. In the frontal view, the horizontal thirds and vertical fifths should be documented as described above. Interpupillary distance (65 mm ± 4), alar base width (32 mm ± 3), length of the upper lip (23 mm in males, 20 mm in females) and lower lip (40 mm in males, 44 mm in females), vermilion show, interlabial gap (2–4 mm), incisal show at rest (2 mm), tooth/gingival show upon smiling (gingiva should not be visible), chin point (relative to facial and dental midlines), and dental midline. In the profile view, a general comment on the skeletal profile should be documented as explained above. Presence of malar or perialar hollowing, nasal dorsum projection as per Goode’s criteria (dorsal length 55%–60% greater than tip projection), nasolabial angle (90–95 degrees in males, 100–105 degrees in females), labiomental angle (120 degrees ±10, female more obtuse than male) and chin-to-throat distance (42 mm ± 6, or 4 fingerbreadths). The dental occlusion should then be closely evaluated, measuring overbite, overjet, Angle’s classification, any discrepancy in centric relation – centric occlusion, maximal incisal opening, and any associated temporomandibular joint symptoms (clicking, crepitus, tenderness). The mandible should be viewed in animation with notice of any deviation on opening/closing, and the presence of any occlusal instability.
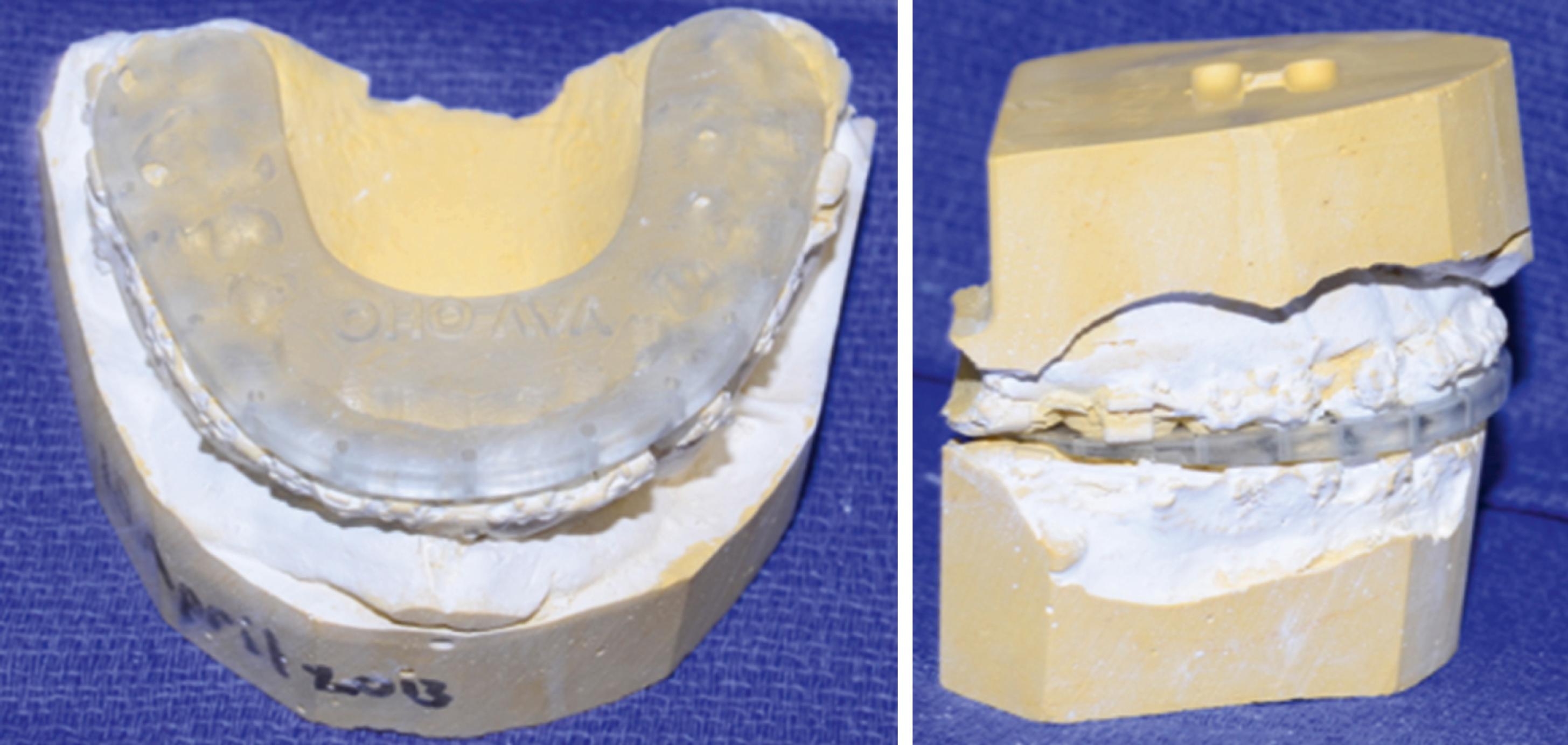
Upon completion of the measurements and record keeping, including a detailed medical/surgical/family history to determine whether the patient is fit to undergo such a procedure, a set of dental impressions should be taken. This is typically performed with an alginate material and appropriately-sized maxillary and mandibular impression trays. The entirety of the dentition, alveolar processes to the depth of the maxillary and mandibular buccal and lingual sulci, hard palate and maxillary tuberosity should be captured in the impression. A dental stone can then be poured into the tray, thus capturing a model of the maxillary and mandibular occlusal relationship for further study. A bite registration should also be taken in the patient’s most reproducible occlusal pattern. The dental models and occlusal bite registration can then be combined with a facebow transfer (an apparatus used to accurately capture the relationship of the maxillary position relative to the skull base and Frankfort horizontal) to mount the exact dentofacial pattern on an articulator. This method is excellent for record keeping and can be used to perform traditional model surgery, although, with the advent of medical modeling and virtual surgical planning, it has become more of an educational tool used to allow trainees to formulate a better idea of the surgical treatment plan.
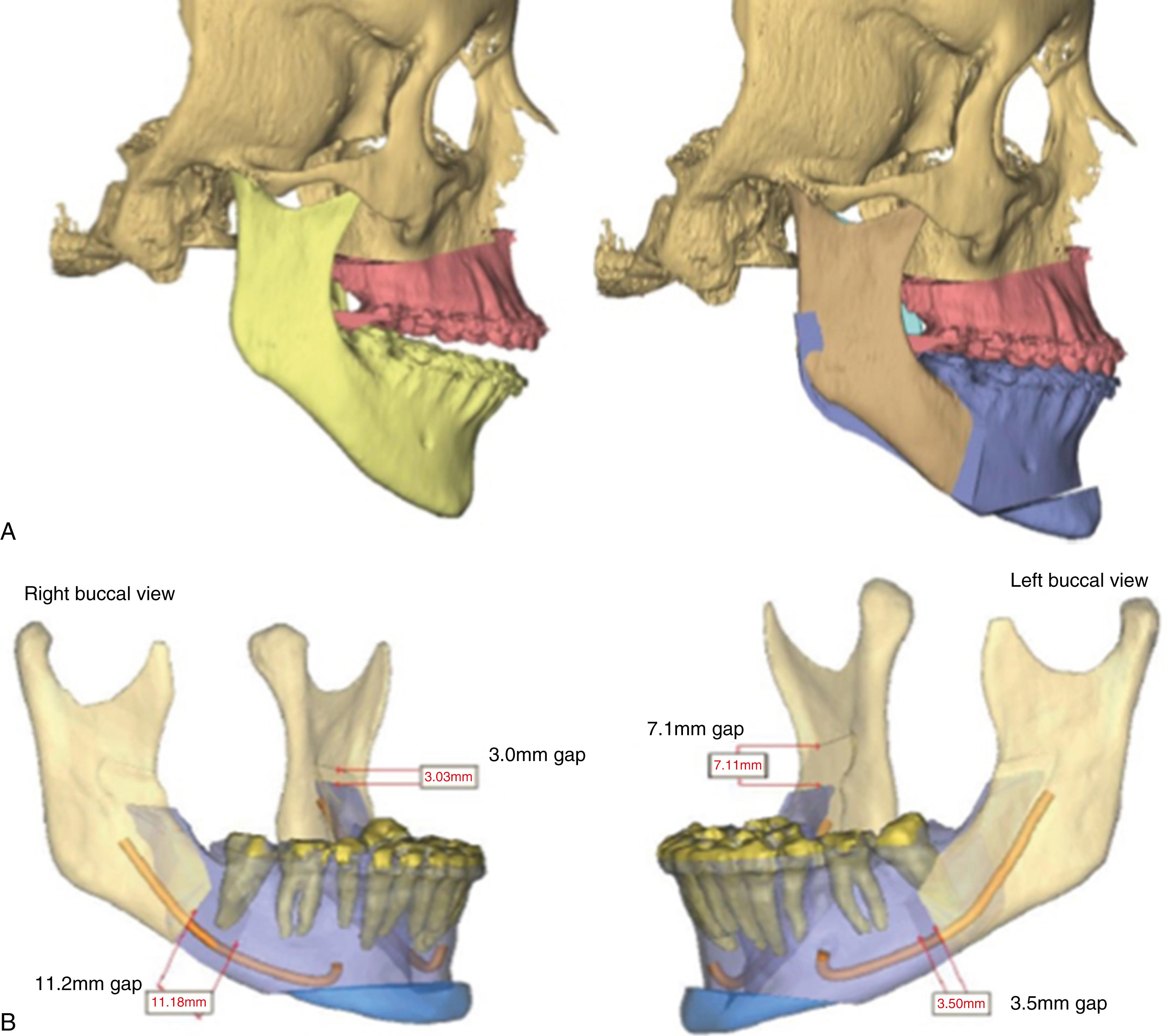
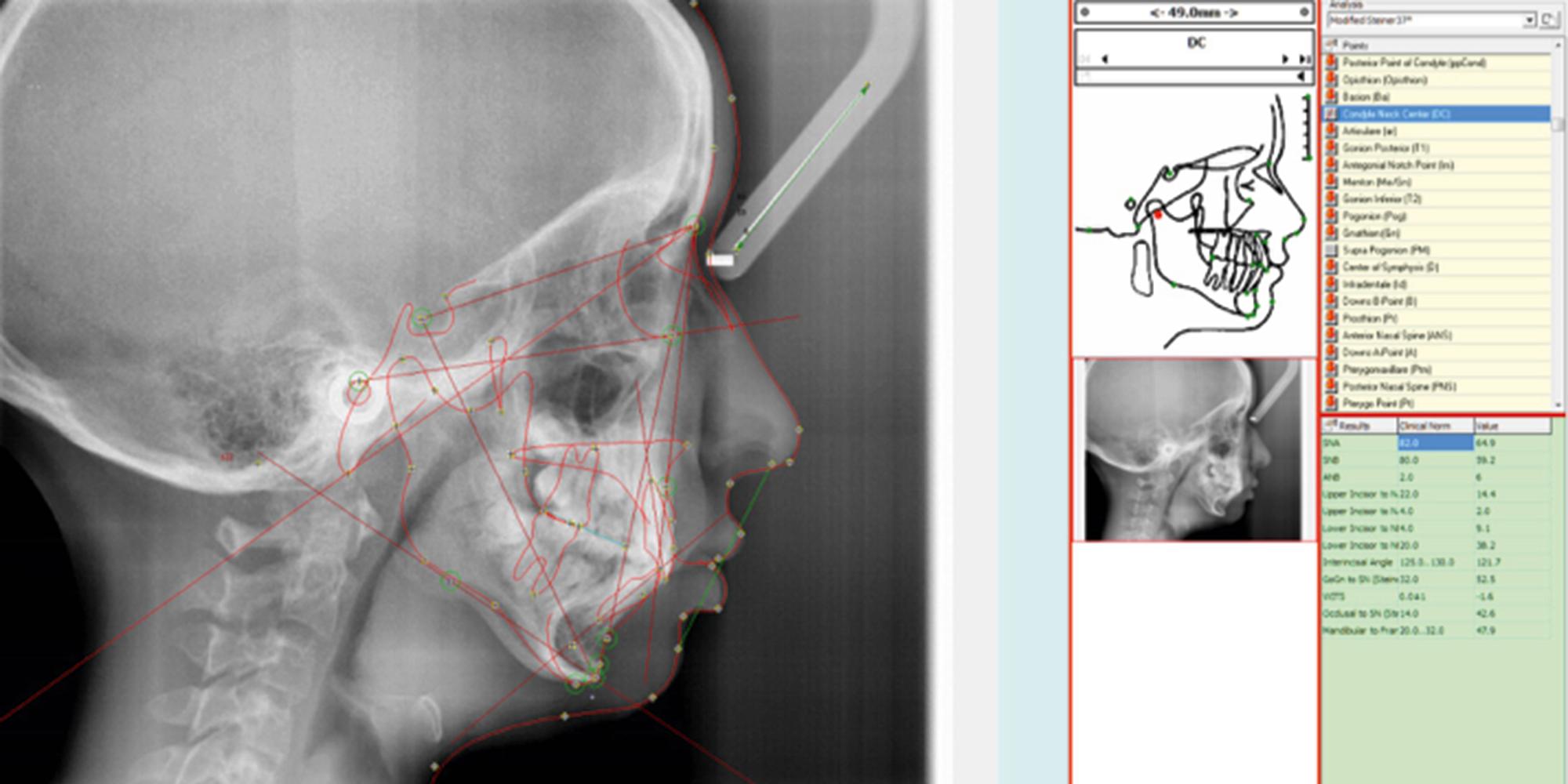
Routine radiological examination is a necessary part of the orthognathic workup. In past times the standard was to perform a lateral cephalogram, as well as plain AP films. This was later supplemented with the panograph, and finally supplanted by the cone beam computed tomography (CT) scan. More so in the present day than previously, three-dimensional imaging has become the standard in many centers with the advent of cone beam CT scans. These cone beam scans subject the patient to a much lower dose of radiation than traditional CT imaging while maintaining adequate image quality. The three-dimensional scans also allow for virtual surgical planning to be performed, thus planning surgical movements expediently as compared to what was previously a time-consuming, multistep process of model surgery that was fraught with small errors that could further be amplified with each step of the process ( Figs. 21.8 and 21.9 ). Virtual surgical planning has greatly streamlined the workflow process, eliminating the tedious steps involved with model surgery and allowing for preoperative visualization of each step in the surgical process. Osteotomies with subsequent bony movements can be planned and visualized in all dimensions, making fine-tuned adjustments to the yaw (i.e., rotation on the Z axis), pitch (rotation on the X axis), and roll (rotation on the Y axis) that were previously difficult to do with traditional model surgery. Intermediate and final surgical splints are also fabricated during these planning sessions. Studies have also shown increased accuracy with virtual planning when compared to traditional methods ( Fig. 21.10 ).

Radiographs are also useful when determining the appropriate time to operate on a growing, peripubertal patient. Serial cephalograms can be taken 6–12 months apart and compared for growth changes, as well as cervical spine radiographs ( Fig. 21.11 ). AP hand and wrist films can be used to demonstrate whether the epiphyseal plate has closed, thus predicting cessation of maxillomandibular growth.

A baseline understanding of cephalometric analysis is also prudent for the operating surgeon. Various studies and analyses exist to examine the relationships of the maxilla, mandible, and skull base when viewing these structures on a lateral cephalogram. Looking at overall facial proportions, the upper facial height can be approximated measuring the distance from nasion to A point, whereas for lower facial height it is from A point from menton. The ideal facial plane is viewed by creating a vertical line, perpendicular to the Frankfort horizontal (orbitale to porion), from nasion to soft tissue pogonion. The anterior cranial base is identified as a line drawn between sella and nasion. The mandibular plane is a line drawn between gonion and menton, whereas the occlusal plane is created with a line between the maxillary and mandibular central incisors and first molars.
Other important cephalometric measurements can be evaluated when comparing the maxilla to the cranial base. This is best viewed with an angle created between the sella, nasion, and A point (SNA). The normal SNA value is 82 degrees ±3, with values greater than 85 degrees signifying a prognathic maxilla, and less than 79 degrees showing a retrognathic maxilla. The mandible is related to the cranial base by the angle between the sella, nasion, and B point (SNB). The normal SNB value is 79 degrees ±3, with a value greater than 82 degrees being consistent with a prognathic mandible, and less than 76 degrees signifying a retrognathic mandible. Chin position is evaluated by looking at the angle between sella, nasion, and pogonion (SNPg). The normal value for SNPg is 80 degrees ±3, with a value greater than 83 degrees being consistent with a protruded chin, and less than 77 degrees showing a retruded chin. A relative measure of the positioning of the maxilla to the mandible is the angle between the A point, nasion, and B point (ANB). The normal ANB value is 1–5 degrees, thus often coinciding with a class I skeletal profile. An ANB value greater than 5 degrees often coincides with a class II skeletal profile, and less than 1 degree with a class III profile , ( Fig. 21.12 ).
The upper airway can also be analyzed using cephalometric landmarks, and these values are useful when considering the potential for treating or creating obstructive airway issues with orthognathic surgery. The length of the soft palate is noted to be from PNS to P point, with a normal value of 37 mm. Values greater than this can be significant for a lengthened soft palate, and possibly naso-/oropharyngeal airway obstruction. Evidence of upper airway obstruction can also be elucidated when measuring the posterior airway space, which can be approximated with a line between the gonion to posterior pharyngeal wall (11 mm), as well as the distance from the mandibular plane to hyoid (15 mm). Lower than normal values for posterior airway space and higher than normal for mandibular plane to hyoid are consistent with airway obstruction , ( Table 21.1 ).
| Cephalometric Landmarks | Normal Values (Range) |
|---|---|
| SNA | 82 degrees (±3) |
| SNB | 79 degrees (±3) |
| ANB | 1-5 degrees |
| SN-MandP | 32 degrees (±5) |
| OcclusalP-FH | 9 degrees (±5) |
| Interincisal angle | 135 degrees (±11) |
| SNPg | 80 degrees (±3) |
| PNS-P | 37 mm |
| PAS | 11 mm |
| MP-H | 15 mm |
It cannot be overstated the importance of developing a comfortable working relationship with an orthodontist who is well versed in surgical cases. Oftentimes the orthodontist will initiate the discussion with a patient about any potential surgical correction of their dentofacial deformity. Important points to note include the estimated length of presurgical orthodontics, or if it is possible to perform surgery prior to initiating orthodontic therapy. The concept of surgery first requires that the maxillary and mandibular dentition is in a position where it can be tripoded (anteriorly and posteriorly) into a stable condition after they have been repositioned. In this new postoperative relationship, the orthodontist must feel comfortable applying orthodontic movements to achieve an appropriate class I occlusal pattern.
Traditionally, an orthodontist will propose a treatment plan and alert the operating surgeon if any necessary teeth (often impacted or supernumerary) need to be removed to optimize the occlusal relationship. After this stage, the orthodontist will decompensate any previous misalignment of the dentition due to the pathological skeletal pattern present. The teeth are then leveled and aligned, often creating a malocclusion that appears worse to the patient than their premorbid condition. If interarch spacing is lacking to align the teeth appropriately, the orthodontist may plan for the surgeon to perform segmental osteotomies (traditionally of the maxilla) so that the arch form can be expanded. Once orthodontic movements are deemed appropriate by the orthodontist, a final surgical wire is often placed to maintain the teeth in their current position (as this dental pattern is used to create the surgical splints and final maxillomandibular relationship). After the surgery is performed, final orthodontic refinements are often necessary for a few months to fine-tune the new occlusal pattern. If third molars are present, it is often left to the discretion of the surgeon whether they will remove them at the time of surgery or prior. If removed prior, at least 6 months of bone healing and consolidation should be allowed prior to performing osteotomies, particularly of the mandible.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here