Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In overdose, any of the oral anticoagulants will elevate the international normalized ratio (INR), although not always in a direct dose-dependent manner.
Activated charcoal decreases the absorption following the ingestion of apixaban and is probably also effective following the ingestion of warfarin, dabigatran and rivaroxaban.
There are clear guidelines for the management of warfarin anticoagulation and these should continue to be followed.
Prothrombinex-VF will reverse the effects of warfarin and rivaroxaban. It does not reverse those of dabigatran but may be effective in apixaban over-coagulation.
Idarucizumab is the reversal agent of choice for major bleeding due to dabigatran.
Limited data on acute rivaroxaban poisoning suggests that it may be relatively benign due to its rate-limited absorption.
The currently available oral anticoagulants are warfarin, dabigatran, apixaban, and rivaroxaban ( Table 25.24.1 ). The direct thrombin inhibitors and factor Xa inhibitors have the advantage of standard dosing without the need for coagulation monitoring.
| Anticoagulant class | Specific drugs | Mechanism of action | Indications a : prevention of venous thromboembolism | Kinetics |
|---|---|---|---|---|
| Vitamin K antagonist | Warfarin | Inhibits synthesis of vitamin K–dependent clotting factors Synthesis of proteins C and S |
VTE Prosthetic heart valves Stroke in patients with previous MI and increased embolic risk AF and a high risk of systemic embolism |
Elimination: hepatic T½: 36–48 h Onset: 3–5 days |
| Direct thrombin inhibitors | Dabigatran | Inhibits fibrin production and thrombin-induced platelet aggregation |
VTE after THR or TKR Recurrent VTE AF and a high risk of systemic embolism |
Onset: 0.5–2 h Elimination:
T½: 12–14 h |
| Factor Xa inhibitors | Apixaban | Inhibits thrombin and fibrin production | VTE after THR or TKR AF and a high risk of systemic embolism |
Onset: 1–3 h Elimination:
T½: 8–15 h |
| Rivaroxaban | VTE after THR or TKR Recurrent VTE AF and a high risk of systemic embolism |
Onset: 2–4 h Elimination:
T½: 7–13 h |
a All agents are indicated for the treatment of thromboembolism.
With experience in the practical use of novel oral anticoagulants (NOACs), also referred to as direct oral anticoagulants (DOACs), their risks and advantages compared with warfarin have been studied. In a meta-analysis of studies of patients with atrial fibrillation, the therapeutic effect of apixaban was marginally superior to that of warfarin for thromboembolic events but not for stroke risk. Apixaban was non-inferior to dabigatran for a therapeutic effect but rivaroxaban was marginally superior for thromboembolic events. The risk of major bleeding was significantly lower for apixaban compared with warfarin, dabigatran, and rivaroxaban.
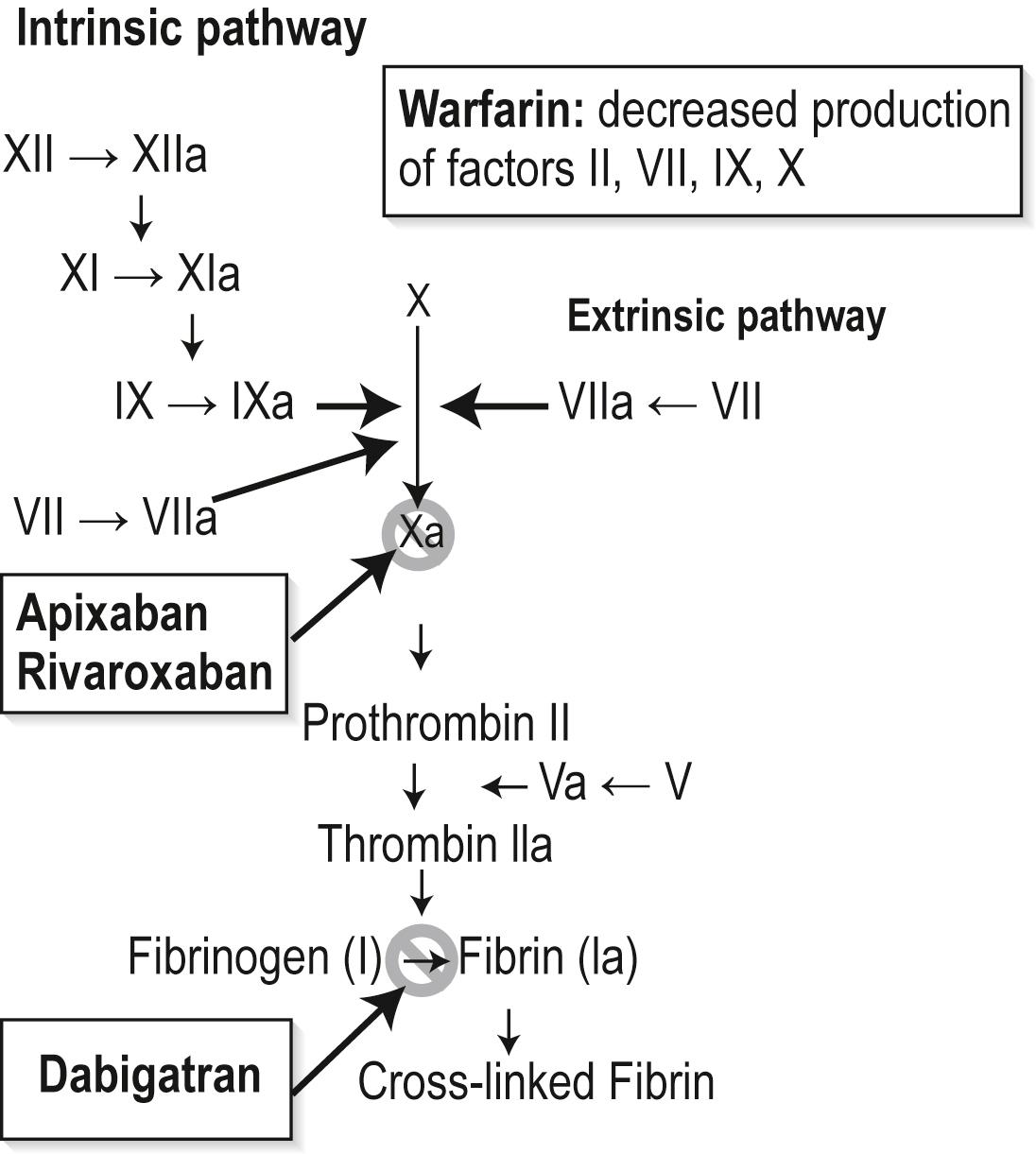
All the oral anticoagulants act on the final common pathway of the intrinsic and extrinsic coagulation pathway; this commences with the production of activated factor X towards a stabilized fibrin clot ( Fig. 25.24.1 ). Additionally, warfarin affects the production of factors VII and IX of the intrinsic pathway.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here