Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In the practice of otology, the various surgical procedures extend along a spectrum from the clinic to the operating room. The procedures performed in the clinic recapitulate the same surgical techniques used in the operating room. For this reason, the process of refining one’s surgical techniques begins in the clinic. The methodology, preparation, and calming bedside manner while performing procedures in the clinic can lead to a trusting patient-physician relationship.
In an era of medicine that is highly focused on cost-containment, the ability to perform procedures in an outpatient setting is encouraged. There are, however, situations where an office-based approach is not suitable. Sedation-based or general anesthesia will likely be required for children, anxious or uncooperative adults, the patient with a narrow ear canal, and for complex or time-consuming procedures. A thorough discussion with the patient regarding expectations regarding the duration of the procedure, levels of pain, noise involved, and the possibility of vertigo will have a positive impact on overall satisfaction.
Prescient planning for an office procedure includes thorough attention to anesthesia considerations. A properly anesthetized surgical site will help maintain a calm patient and in turn, steady the surgeon’s hands. As the surgical site expands in size, the options for anesthesia advance from topical agents and local anesthesia to regional blocks.
A number of topical agents have been studied for use on the intact tympanic membrane (TM). There are several considerations when choosing a topical agent. The ear must be meticulously cleaned in order for a topical agent to be effective. A thickened TM related to acute otitis media may require an extended treatment time or make a topical anesthetic ineffective. A perforated TM will allow the anesthetic agent to contact the middle ear structures, which may contribute to temporary facial nerve paralysis or vertigo.
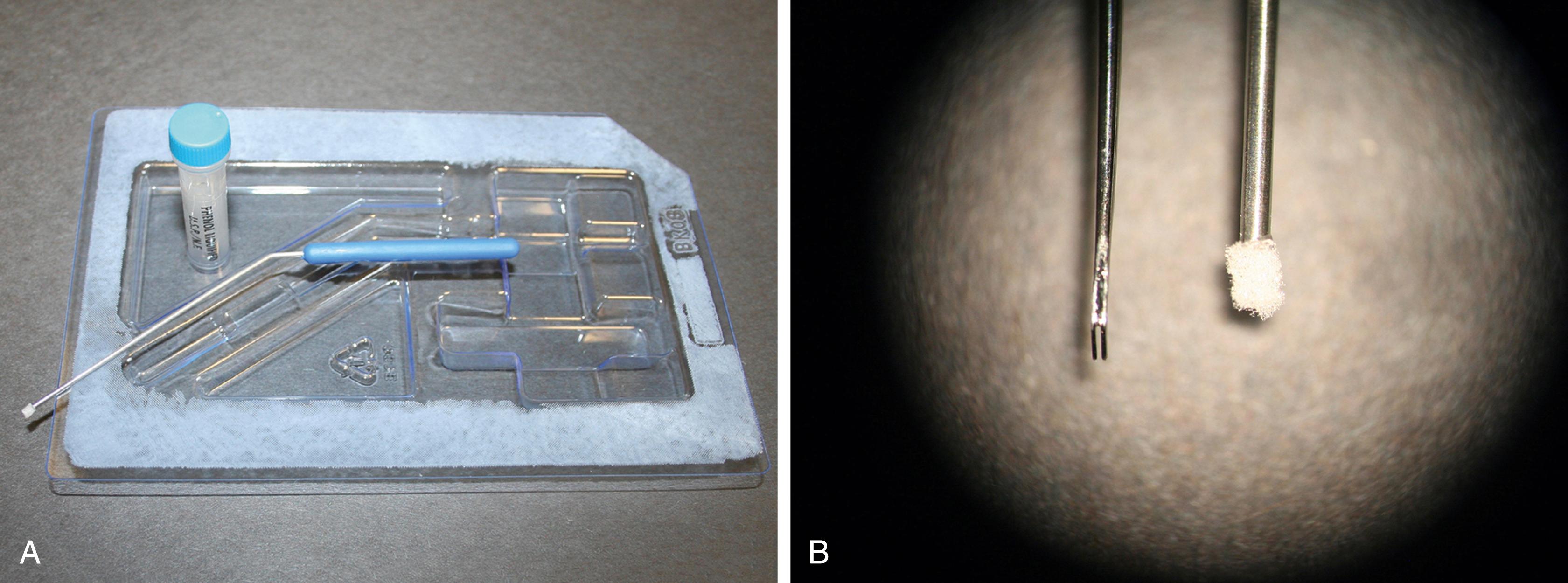
Phenol works as an effective topical anesthetic by creating a chemical burn that both anesthetizes the TM and provides hemostasis. This is the preferred topical anesthetic used for the TM. Excess use may contribute to scarring or irritation. It is used sparingly in a linear focal region for myringotomy and small focal regions for intratympanic injections. There are three options for application. A phenol applicator acts like a quill pen to deliver a precise amount of phenol. Other options include use of a small wisp of cotton on a metal applicator or via a disposable phenol kit with a sponge tipped applicator ( Fig. 125.1 ). Care must be taken to ensure that the TM is dry in order to maintain a focal application. The patient must be informed that this method will cause a temporary burning sensation lasting seconds. Blanching of the TM is noted as immediately indicating the expected effect.
There are no standard concentrations of topical lidocaine or tetracaine. However, solutions of 4% to 10% lidocaine (amide) in saline or 8% to 10% tetracaine (ester) in isopropyl alcohol are the most commonly described preparations.
With the patient positioned supine with the head turned away, the medial half of the ear canal is filled with the predetermined anesthetic agent. The tympanic membrane must be treated for approximately 15 minutes for lidocaine and 60 minutes for tetracaine. Use of a cotton pledget or an oto-wick placed in the ear will allow the patient to ambulate while allowing the allotted time to lapse. Before commencing with the surgical procedure, the solution should be removed completely from the canal and the site should be tested to ensure proper anesthesia.
Eutectic mixture of local anesthesia (EMLA) cream is an emulsion containing lidocaine 2.5% and prilocaine 2.5%, which is pH buffered to 9. This is easily applied to the TM with minimal risk of entry to the middle ear; however, it does not always provide adequate anesthesia. Furthermore, at least 1 hour is required for EMLA to be absorbed and take effect.
Procedures involving the external ear generally can be performed in the outpatient setting. Depending on the site and extent of the procedure, topical, local, or regional anesthetics could be considered.
The benefit of providing an anesthetic without the need of a needle stick is favorable in children and in certain adults. EMLA or lidocaine-epinephrine-tetracaine (LET) can be used on intact or broken skin. LET is a combination of lidocaine (4%), epinephrine (0.1%), and tetracaine (0.5%) in an aqueous solution or gel.
These agents are applied directly to the surgical field and are covered with an occlusive dressing for a minimum of 30 minutes for LET and 60 minutes for EMLA. The site is then tested with a pinprick in order to ensure that an appropriate level of anesthesia has been achieved.
The hemostatic benefits of added epinephrine in injected local anesthetic agents are well recognized. Several studies have demonstrated the safe use of injectable lidocaine with epinephrine in the external ear. Diluting the solution with a 1:10 ratio of bicarbonate to lidocaine will reduce burning at the injection site.
The injection site is swabbed with an alcohol swab. A smaller syringe (1 to 3 mL) will facilitate ease of injection, and a 25-gauge needle or smaller is recommended. The pain associated with injection will be minimized by injecting slowly, through use of distracting measures, and by minimizing the total number of skin punctures. The maximum dose of 1% lidocaine with epinephrine is 7 mg/kg up to 500 mg or 50 mL. The maximum dose of lidocaine without epinephrine is 4.5 mg/kg. The desired effect is generally noted in 2 minutes and should last for 4 to 6 hours.
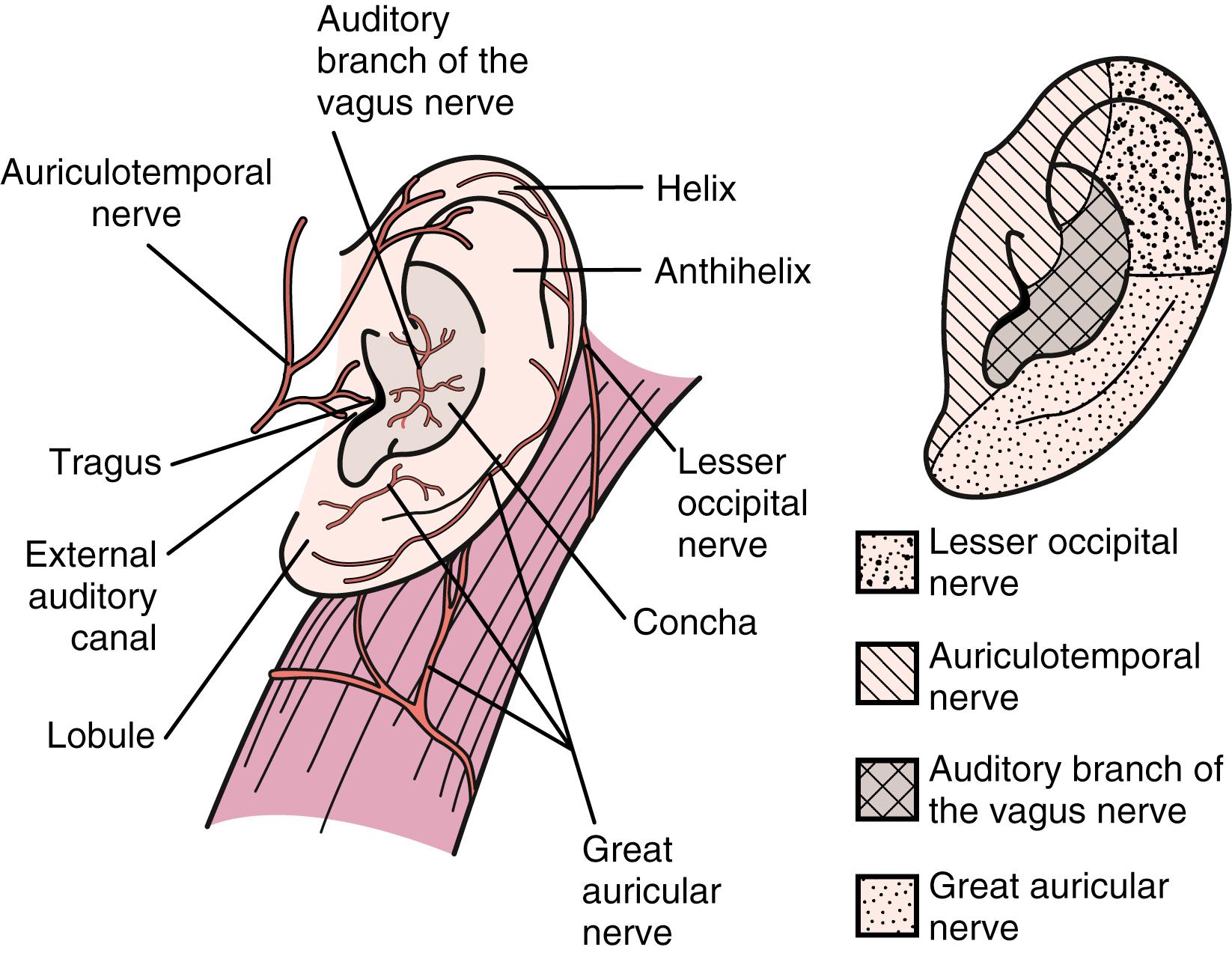
Regional anesthesia can be employed for procedures involving the TM, the external auditory canal (EAC), and the pinna. The pinna and meatus of the EAC receive their sensory innervation from the third cervical nerve and from the trigeminal, facial, and vagal nerves ( Fig. 125.2 ). The great auricular nerve and the lesser occipital nerves are branches of the third cervical nerve and cervical plexus. The great auricular nerve provides sensory innervation to the skin overlying the mastoid process and the inferior pinna. The lesser occipital nerve provides sensation to the middle section of the pinna. The auriculotemporal nerve, which is a branch of the mandibular branch of the trigeminal nerve, innervates the superior portion of the pinna. The auditory branch of the vagus supplies the concha and EAC. The EAC also receives innervation from the trigeminal and facial nerves and from the cervical plexus.
There are two regional blocks that are frequently used in order to facilitate procedures of the pinna, EAC, and TM. A four-quadrant EAC block will provide anesthesia to the canal and TM but not the pinna. An outer ear block will provide anesthesia to the pinna but not the EAC or TM.
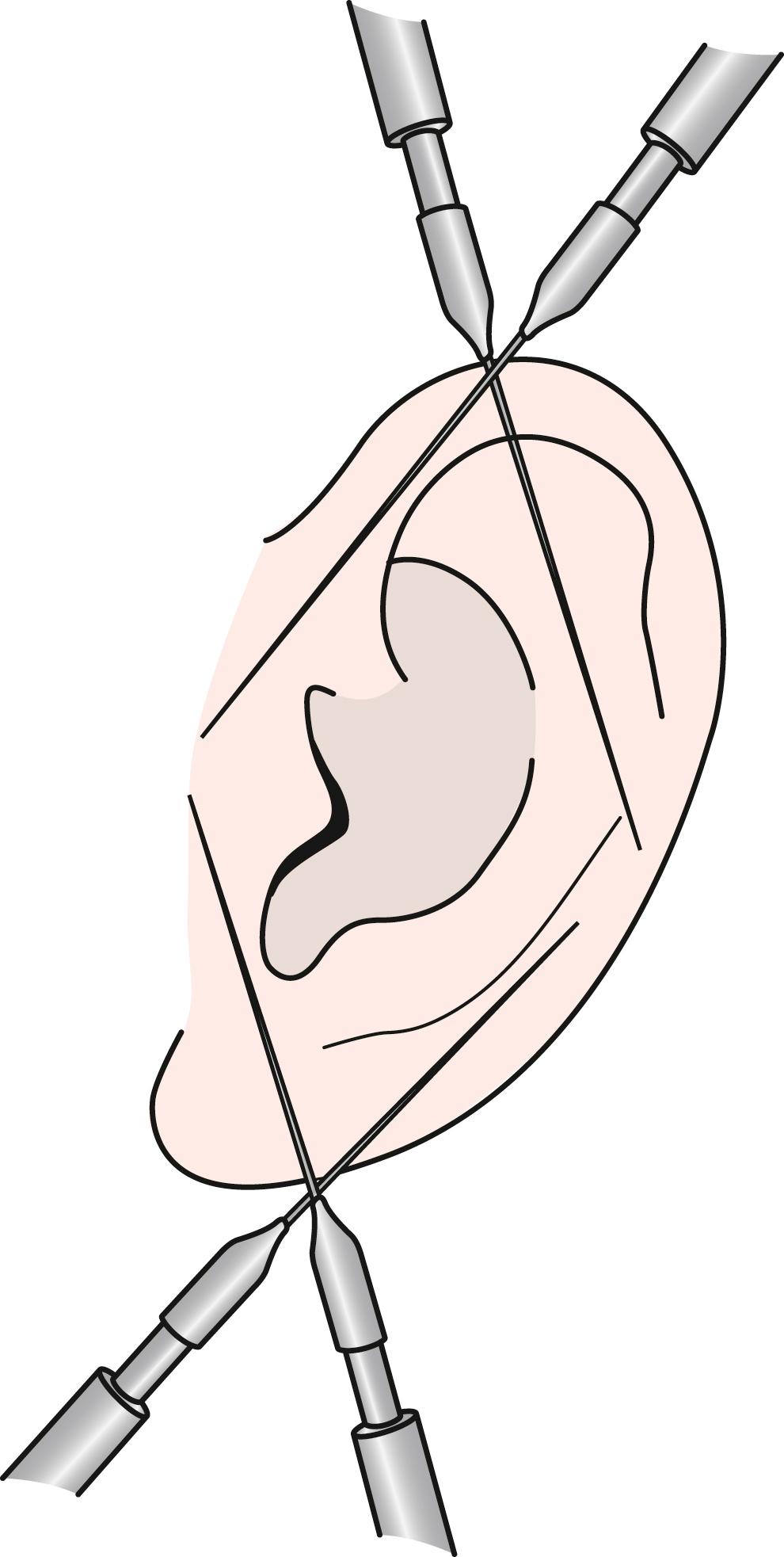
Providing anesthesia to the entire pinna may be helpful for treatment of large auricular hematomas, laceration repairs, or excisions. This may be performed with only two injection entry sites, one each at the superior and inferior junction of the attachment of the pinna to the head ( Fig. 125.3 ). A 10-mL syringe is filled with 1% lidocaine with epinephrine, and a 25-gauge needle is attached. The injection sites are swabbed with alcohol. The needle is advanced fully in a subcuticular plane while drawing back on the syringe in order to ensure that the injection is not administered intravascularly. While the needle is withdrawn, approximately 2 to 3 mL is injected. Without removing the needle completely from the injection site, the direction of the needle is altered to treat the posterior aspect of the pinna. Again, 2 to 3 mL is injected. This same procedure is repeated for the inferior pole of the pinna.
This technique again uses 1% lidocaine with 1:100,000 epinephrine. A smaller syringe, 1 to 3 mL, is used in order to provide greater dexterity and visibility with a 27-gauge needle. The needle is inserted at the bony cartilaginous junction with the needle advanced a few millimeters along the bone. An aural speculum is held with slight pressure applied to the canal wall lateral to the injection site in order to encourage medial diffusion of the anesthesia. The injection is performed with direct visualization of the medial canal in order to watch for blanching. Careful observation is employed to detect early signs of bleb formation, which is to be avoided.
Obstruction of the ear canal with cerumen is the most likely cause of a conductive hearing loss in adults. The ear canal is naturally self-cleaning. Excess cerumen, dirt, dust, hair, and exfoliated squamous cells are expelled through gradual outward migration of the epithelium of the TM and external auditory canal. This process of self-cleaning can be interrupted by a narrow ear canal, use of a hearing aid, use of cotton swabs, and a prior history of radiation therapy to this region. If the self-cleaning process is not effective, physical débridement of cerumen by a clinician may be required. The task of removing cerumen generally falls on primary care physicians; however, there are instances where these techniques may not be effective or appropriate. Flushing the ear canal in the face of a perforated, retracted, or atrophic TM is not recommended.
Under microscopic vision, cerumen is removed with suction, wax curettes, Hartman forceps, or picks. In a large canal with a favorable shape, cerumen may be grasped easily with Hartman or small alligator forceps. In a narrow canal or if the canal is occluded by cerumen, the interface between the cerumen and canal wall should be identified. The contour of the canal is followed to the medial aspect of the cerumen or TM. The consistency of the cerumen will dictate the choice of suction, picks, alligator forceps, or curettes. A small right angle pick is helpful in identifying the interface between the canal and the cerumen and for removal of cerumen impacted against the TM. For wet or soft cerumen, aspiration of cerumen is generally the most efficient method of removal. Generally, 5F suction is employed. The size of suction device should be reduced to 3F when working adjacent to the TM. A 7F suction device should be limited to the onset of the procedure if the canal is completely obstructed and should be quickly replaced with a 5F device in order to minimize noise exposure. Treating the cerumen with Colace may facilitate removal. To do this, the lateral canal is filled with Colace solution (docusate sodium liquid, 100 mg/10 mL) and should remain for 15 minutes prior to proceeding with removal.
Mastoid cavity débridement employs similar principles. Review of the prior operative note is helpful in order to determine the status of the TM, middle ear structures, horizontal semicircular canal, facial nerve, and tegmen. The degree of difficulty noted with mastoid cavity care is greatly dependent on the postoperative anatomy of the meatus and mastoid. It is important to remove all squamous and ceruminous debris. Some moisture medial to the debris may be revealed, which may be dusted with Boric acid powder in order to prevent infection. Excessive moisture may be cleared with suctioning; however, this commonly leads to complaints of dizziness. Swabbing the mastoid cavity with cotton held by an alligator forceps or metal applicator may limit the need for suction. The use of a smaller diameter suction device will minimize dizziness.
Hematoma of the auricle is most commonly noted in wrestlers but is also seen in other sports such as boxing and rugby. Hematoma of the auricle is formed by a shearing force, which separates the skin and perichondrium from the underlying cartilage. Wrestling headgear and rugby scrum caps help reduce the incidence of auricular hematomas.
Cartilage receives its blood supply from the overlying perichondrium. A shearing injury will cause a collection of blood separating the vascular supply from the cartilage, which will result in cartilage necrosis. “Cauliflower ear” is the term used to describe the altered appearance of the pinna related to subsequent fibrosis, contracture, and formation of reactive or calcified perichondrium. The urgent treatment of auricular hematoma is encouraged in order to reestablish the blood supply to the cartilage and avoid this sequela. The resulting deformity of the pinna is primarily a cosmetic concern; however, thickening of cartilage in the conchal region may lead to a collapsing ear canal and hearing loss.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here