Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
|
|
|
|
|
|
|
|
The literature shows that sound biomechanical constructs of the cervical spine decrease the percentage of nonunions and implant failures. Therefore, it is essential that the surgical procedures selected increase the biomechanical strength of a construct while addressing the cervical spine dysfunction. The most common failures occur when treating cervical dysfunction with multilevel anterior corpectomy reconstructions and the least common occur with single-level anterior cervical corpectomy procedures.
When developing a surgical plan for the management of spinal disorders, the goals of the intervention should include obtaining adequate decompression, restoring sagittal balance, and creating long-lasting stability by achieving solid fusion. Inherently, one should attempt cervical reconstruction to create a biomechanically desirable construct with as minimal an operation as possible. Regardless, all operations should also minimize causes of implant failure. The purpose of this chapter is to review the causes, diagnosis, and management for pseudarthrosis and implant failures in the cervical spine.
Most commonly, implant failure is either caused by the development of pseudarthrosis or is secondary to excessive biomechanical loads. Multilevel cervical corpectomy has a reported rate of failure of 9% and 50% for two-level and three-level anterior cervical corpectomy plated reconstructions, respectively. Other studies have demonstrated a failure rate of 6% with two-level corpectomy and anterior plating increasing to a 71% failure rate with three-level corpectomy and anterior plating. Regardless, the failure rate of cervical anterior corpectomy appears to increase as the number of corpectomy levels increases. Furthermore, the addition of an anterior cervical plate has not eliminated this complication.
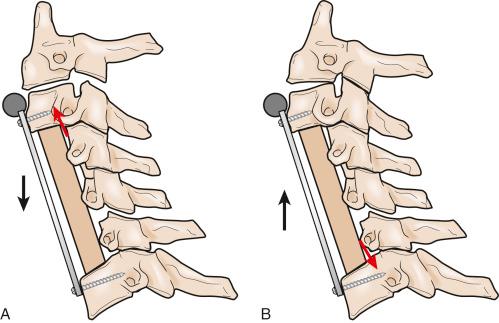
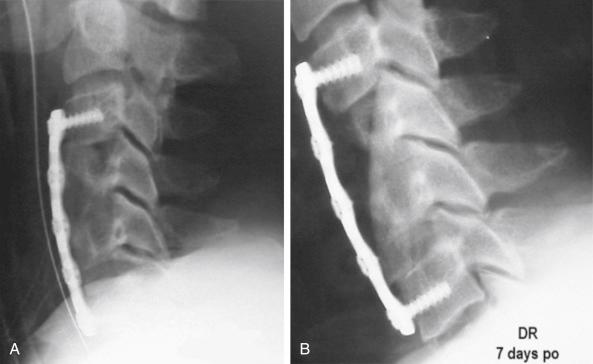
Biomechanically, the addition of an anterior cervical plate moves the instantaneous axis of rotation anteriorly in a long graft construct. The resulting forces cause reversal of the loading pattern when compared with what is seen in the uninstrumented constructs. The addition of an anterior cervical plate leads to paradoxical unloading of the graft in flexion and increased compression of the graft in extension ( Fig. 56-1 ). Theoretically, this motion can result in graft cavitation through the caudal vertebral body and loosening of the plate from the lowest vertebral body. Loose anterior cervical plates are at risk for kicking out anteriorly, typically at the lowest level. Conversely, the proximal portion of the graft is at risk for dislodgment posteriorly into the spinal canal, with resulting spinal cord compression ( Fig. 56-2 ).
Junctional (buttress) plates span only the superior, inferior, or both ends of the strut graft and act as a buttress plate against graft kick-out. However, attempts at using an anterior cervical junctional plate alone in multilevel reconstructions with strut grafts without posterior instrumentation have been shown to increase the risk of failure. Complications associated with strut graft dislodgment can be devastating and include, among other things, catastrophic neurologic compromise and tracheal and esophageal injury. As a result, junctional plates are no longer routinely used alone and are typically used in conjunction with posterior fixation.
The presence of cervical strut or interbody graft pseudarthrosis does not always lead to symptoms. However, if fusion fails to occur, then implant failure is possible. Although uncommon, even long strut grafts that heal at their cephalad and caudal ends can still fracture in the body of the strut graft itself ( Fig. 56-3 ). Other reported complications include plate and screw breakage or dislodgment. The decision to proceed with operative revision of these implant failures is determined by the patient’s symptoms and should be individualized to the patient’s need and the surgeon’s preference and experience.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here