Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Anatomic anomalies of the female reproductive tract occur in 7% of females. They can be secondary to defects in fusion of the Müllerian ducts or abnormal development of the urogenital sinus or cloaca in which the vagina is involved. These abnormalities can be divided in two categories: obstructive and nonobstructive.
The obstructive anomalies of the Müllerian tract involving the vagina, which are typically diagnosed in puberty, include hymenal abnormalities, transverse or longitudinal vaginal septa, and segmental forms of vaginal agenesis. The nonobstructive abnormalities are represented by vaginal agenesis, incomplete transverse or longitudinal vaginal septa, and vaginal narrowing due to “vaginal bands.”
Imperforate or septate hymen is detected in 1:2000 girls and is usually asymptomatic until adolescence, when the accumulation of uterovaginal secretions and menstrual blood causes symptoms. Rarely, there is a familial occurrence or an association with Escobar syndrome. Patients typically present with cyclic lower abdominal or pelvic pain and no evidence of menses. Urologic (i.e., urinary retention, bilateral hydronephrosis, or bladder perforation) or gastrointestinal manifestations (i.e., changes in bowel habits or bowel obstruction), elevations of CA125 and CA 19-9, and peritonitis can also be seen. In newborns and infants, maternal estrogen may rarely stimulate uterovaginal secretions and cause hydrometrocolpos with secondary renal insufficiency with or without hydronephrosis. Physical examination demonstrates no hymenal opening or hymenal remnants usually associated with a hymenal membrane that is bulging or has a blue hue. If longstanding, an abdominal/pelvic mass may be palpated.
Hymenectomy is the standard treatment. Other therapeutic modalities include hymenotomy and the intravaginal use of a Foley catheter for 2 weeks after puncture of the hymen with a sterile injector needle. Treatment failure is seen in rare cases; therefore, follow-up is required.
A transverse vaginal septum can be located at any level of the vagina; however, 40% of the cases are in the upper third. The septum varies in thickness but is usually <1 cm. Congenital uterine anomalies can be associated with vaginal septa, more commonly the longitudinal type. When present, uterine abnormalities include septate uterus, bicornuate uterus, arcuate uterus, unicornuate uterus, and uterus didelphys. The combination of obstructed hemivagina due to a longitudinal vaginal septum attached to the vaginal sidewall, uterus didelphys, and unilateral renal agenesis, is known as Herlyn-Werner-Wunderlich syndrome. Clinically, patients with transverse vaginal septum often present with hematocolpos/hematometra soon after menarche while patients with longitudinal septum may remain asymptomatic. Pelvic magnetic resonance imaging (MRI) and ultrasound are used to diagnose these anomalies, which are surgically treated. Early recognition is important to avoid infertility.
These are usually designated as complete or partial atresia most commonly involving the lower vagina. If the vagina is absent, but the uterine cervix and corpus are developed, patients tend to present with pelvic pain occurring only a few months after obstructed flow. Physical examination demonstrates a normal hymen and a nonpatent vagina. The upper vagina may be present but is separate from the perineum. Pelvic MRI allows a definitive diagnosis. Cervical dysgenesis can also be present (uterus is normally developed, but the cervix is not present or not open to menstrual flow). Clinically, patients present with severe pain and primary amenorrhea. Fifty per cent of the cases of cervical agenesis or dysgenesis are associated with vaginal agenesis and 33% are associated with additional Müllerian abnormalities. These segmental forms of vaginal agenesis are surgically treated.
The absence of vagina can be seen in Müllerian aplasia syndromes occurring in 46 XX females, such as the Mayer-Rokitansky-Küster-Hauser syndrome or Müllerian-renal-cervical syndrome, or in conjunction with certain disorders of sexual differentiation, such as mixed gonadal dysgenesis, complete androgen insensitivity syndrome, or partial androgen insensitivity syndrome. The Mayer-Rokitansky-Küster-Hauser syndrome is characterized by the congenital absence of the uterus, cervix, and vagina. It occurs in 1:4500–5000 live female births. Patients present with primary amenorrhea (and this association represents the second most common cause following gonadal dysgenesis). Physical examination shows normal external genitalia and hymen. MRI is the gold standard to identify the absence of uterus and vagina. Once this abnormality is detected, renal, cardiac, hearing, and spine anomalies need to be excluded. In addition, chromosomal studies and testosterone levels are required. Treatment consists of creation of a neovagina through progressive use of vaginal dilators or surgery.
This is the most common cause of vaginitis. It is the result of a change in the vaginal flora from the normally dominant lactic-acid producing bacteria, such as Lactobacillus spp., to a mixed flora with an increased number and diversity of obligate anaerobes, such as Gardnerella spp., Prevotella spp., Atopobium vaginae , Mobiluncus spp., and bacterial vaginosis-associated bacteriae (BVAB 1 to 3).
Bacterial vaginosis is a clinical diagnosis that requires at least three of the following features: (1) vaginal pH >4.5; (2) thin, watery, nonpurulent discharge; (3) wet mount showing >20% clue cells, and (4) positive “amine” odor test (performed by adding 10% potassium hydroxide to a drop of vaginal discharge on a slide and smelling the fishy odor that results from released volatilized amines). Risk factors include: black ethnicity, cigarette smoking, intrauterine device, oral sex, new or multiple sexual partners, female sexual partner, frequent douching, sexual activity during menses, and lack of hydrogen peroxide-producing lactobacilli.
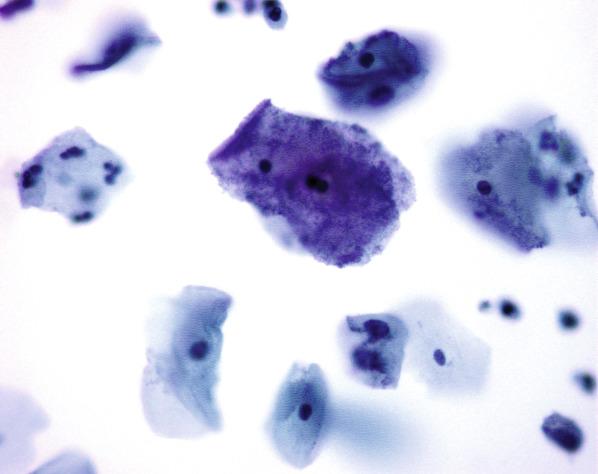
No specific histopathologic changes have been described. Wet mount shows >20% clue cells (i.e., squamous cells with numerous adherent coccobacilli) and an altered background vaginal flora with numerous cocci, bacteria of different shapes, and few, if any, lactobacilli. This abnormal vaginal flora can also be seen on Gram stain. Clue cells can also be detected on Papanicolaou smears ( Fig. 5.1 ). Fluorescence in situ hybridization shows a characteristic dense biofilm in confluent or patchy layers covering at least 50% of the vaginal epithelial surface in vaginal biopsies. These biofilms are polymicrobial and dominated by Gardnerella vaginalis.
Bacterial vaginosis is treated with a 7-day course of oral metronidazole, a 5-day course of vaginal metronidazole gel, or a 7-day course of vaginal clindamycin cream. This infection is associated with an increased risk of upper genital tract infections and sexually transmitted diseases, and adverse pregnancy outcomes including increased risk for preterm birth and late miscarriage.
Clinical diagnosis requiring at least three of the following features:
Vaginal pH>4.5
Thin, watery, noninflammatory discharge
Wet mount showing >20% clue cells
Positive “amine” odor test
Most common cause of vaginitis
Thin, watery, nonpurulent discharge
7 days of oral metronidazole, 5 days of vaginal metronidazole gel, or 7 days of vaginal clindamycin cream
Increased risk of upper genital tract infections or sexually transmitted diseases, and adverse pregnancy outcomes
No specific histopathologic changes
Clue cells (i.e., squamous cells with numerous adherent coccobacilli) on wet mount or Papanicolaou smear
Altered vaginal flora with numerous cocci, bacteria of different shapes, and few, if any, lactobacilli on wet mount or Gram stain
Biofilm covering the vaginal epithelium by fluorescence in situ hybridization
This represents the second most frequent cause of acute vaginitis after bacterial vaginosis. The term “vulvovaginal candidiasis” is frequently used as the vulva is commonly affected and causes most of the patient’s symptoms. The majority (85% to 90%) are caused by Candida albicans but the number of cases caused by non– Candida albicans species is increasing, especially Candida glabrata. In asymptomatic patients, prevalence has been reported in up to 10%. Therefore, identification of vulvovaginal Candida is not necessarily indicative of vaginitis.
Symptoms include vulvovaginal pruritus, soreness, irritation, dyspareunia, and a white, thick, nonmalodorous vaginal discharge. There is vaginal erythema and edema, and sometimes excoriation or fissure formation of the vulva. Host risk factors include pregnancy, diabetes mellitus, immunosuppression, systemic antibiotics, glucocorticoid use, and genetic predisposition. Behavioral risk factors include use of oral contraceptives, intrauterine device, hygiene and clothing habits, and sexual preferences.
The vaginal mucosa frequently appears erythematous.
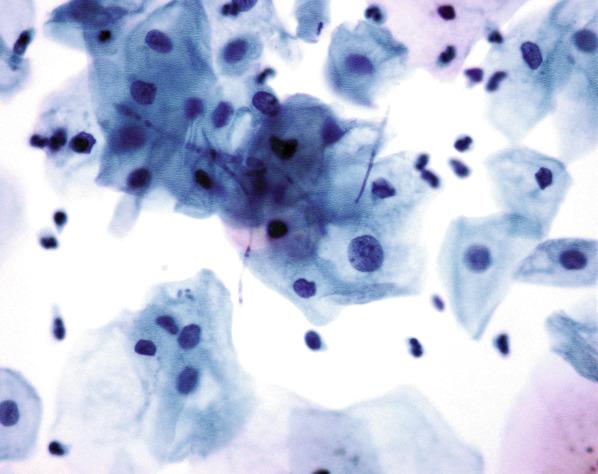
Hyphae or spores are visible on a potassium hydroxide wet mount or Papanicolaou smear ( Fig. 5.2 ). Tissue sections show marked acute inflammation, reactive changes in the squamous epithelium, and fungal forms within the superficial layers of the squamous epithelium or within the detached squamous cells. A vaginal culture is useful if a wet mount is negative. Although polymerase chain reaction (PCR) to detect Candida genus is more sensitive than culture, it is not necessary in routine practice.
Uncomplicated vaginal candidiasis (defined as three or fewer episodes per year) with mild to moderate symptoms, caused by C. albicans , and occurring in an immunocompetent host, is treated with a single dose of oral fluconazole or other topical antifungal agents. If complicated (i.e., pregnant patients, immunocompromised or debilitated patients or those who have uncontrolled diabetes, severe symptoms, infections by species other than C. albicans , or four or more episodes in 1 year), treatment may involve stronger and more prolonged antifungal regimens.
Second most common cause of acute vulvovaginitis
White, thick, nonmalodorous vaginal discharge
Pruritus, soreness, irritation, and dyspareunia
Single dose oral fluconazole or topical antifungal agents, if uncomplicated
Tailored treatment, if complicated (immunosuppressed patients)
Mucosal erythema
Marked acute inflammation and reactive changes of squamous epithelium
Hyphae or spores identified in surface epithelium or within detached squamous cells in potassium hydroxide wet mount or Papanicolaou smear
Vaginal culture (if wet mount negative)
This intracellular parasite is the most common nonviral sexually transmitted infection worldwide. Prevalence rates vary greatly and depend on the affected population’s risk factors. In the United States, the highest prevalence of this infection is in African American women (rates of 13–51%). Other risk factors include older age, intravenous drug use, incarceration, multiple sexual partners, and bacterial vaginosis.
Eighty-five per cent of women with T. vaginalis infection are asymptomatic. The remaining 15% present with yellow-green, malodorous vaginal discharge, pruritus, vulvar irritation, dysuria, and/or abdominal pain. On colposcopic examination, the vaginal mucosa is erythematous with variable punctate hemorrhages. If the cervix is involved, the term “strawberry cervix” has been applied.
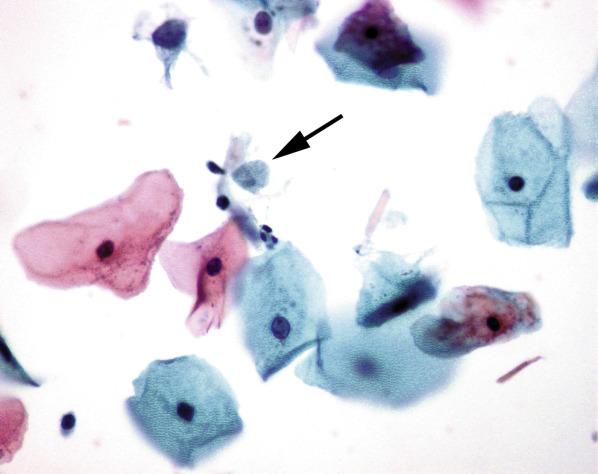
On biopsy, the vaginal squamous epithelium is usually spongiotic with numerous neutrophils that can form intraepithelial abscesses; the organism is not usually seen. The diagnosis is made by identifying pear-shaped cyanophilic organisms, 10–20 μm in diameter, showing polar flagellae associated with numerous neutrophils in a saline preparation (sensitivity ranging from 50% to 70%; specificity approaches 100%). Trichomonas can also be detected on a Papanicolaou smear (∼70% sensitivity), where they are also pear-shaped and show a “lancet”-shaped axostyle (microtubular structure that runs across the longer axis of the microorganism), an eccentrically placed nucleus and red cytoplasmic granules ( Fig. 5.3 ). Diagnosis by nucleic acid probe techniques are highly (95%–100%) sensitive and specific, but expensive and not easily accessible.
Most common nonviral sexually transmitted infection
Patients typically asymptomatic (85%)
Yellow-green, malodorous vaginal discharge, pruritus, dysuria, vulvar irritation, and abdominal pain, if symptomatic
Oral nitroimidazole or tinidazole
Treatment of patient’s partner
Mucosal erythema +/- variable punctate hemorrhage
Spongiotic squamous epithelium with numerous neutrophils that may form intraepithelial abscesses but without visualization of organism on biopsy material
Trichomonas appear as pear-shaped organisms on saline preparation or Papanicolaou smear
Infection by this organism is uncommon. Risk factors include a household or personal history of dermal or respiratory infection by Group A Streptococcus (GAS). It typically affects prepubertal girls but can also be seen in adult women, mostly in association with lactational and menopausal vaginal atrophy. GAS vulvovaginitis is a common cause of vaginal and/or perineal pain in contrast to most other types of vaginitis. In addition, patients have dyspareunia, burning sensation, or pruritis. Vaginal discharge is often copious and may be watery, yellow or purulent but is typically non-malodorous. Physical examination reveals marked erythema, edema, and tenderness of the vagina, vulva, and perineum that may be accompanied by excoriations secondary to scratching. Wet mount and Gram stain of vaginal smears typically show abundant leukocytes, gram positive cocci in singlets, duplets, or chains, and a lack of lactobacilli. GAS overgrowth on culture is required to confirm the diagnosis. Treatment includes penicillin or topical clindamycin. In cases of marked vaginal atrophy, topical estrogen may be necessary to prevent recurrences.
This Gram-positive bacterium is present in the digestive and vaginal tracts of 25% of the female population. Patients with symptoms and a positive culture should be treated with antibiotics. In asymptomatic patients, vaginal group B Streptococcus does not require treatment except during pregnancy. As group B Streptococcus represents the leading cause of early-onset neonatal sepsis in the United States, universal screening, using both vaginal and rectal swabs, is recommended for pregnant women at 35 to 37 weeks’ gestation. Identification of group B Streptococcus in these samples, by routine cultures or using sensitive nucleic acid amplification tests, will prompt therapy which includes penicillin G, cefazolin, clindamycin, or vancomycin depending on allergies and antibiotic resistance.
These are Gram-positive, non-acid-fast, anaerobic bacteria that are part of the normal flora of the oral cavity and rectum, but can also be occasionally found in the female genital tract. Vaginal colonization and secondary overgrowth may occur in the presence of a foreign body (e.g., permanent suture material or synthetic mesh to correct genital prolapse). In the upper genital tract, infection is typically associated with an intrauterine device. Their detection in asymptomatic individuals without a foreign body does not appear to require treatment. Symptoms related to Actinomyces infection include malodorous vaginal discharge, vaginal bleeding, or abdominopelvic pain due to abscess formation. Microscopically, these bacteria are seen as blue delicate filamentous organisms typically radiating from a central core in a background of neutrophils. A positive Grocott-Gomori methenamine silver nitrate (GMS) stain and gram stain is used to distinguish actinomycotic from noninfectious pseudoactinomycotic radiate granules; the latter typically also have thicker filaments. Treatment is warranted in symptomatic cases and involves removal of the foreign body and use of penicillin.
This acute disease is characterized by hypotension and multisystemic involvement (including two or more of the following: renal impairment, coagulopathy, hepatic or central nervous system dysfunction, acute respiratory distress syndrome, gastrointestinal symptoms—such as vomiting or diarrhea, or muscular involvement—as severe myalgia or creatinine phosphokinase level at least twice the upper limit of normal) with or without erythematous macular rash that may desquamate. TSS may be associated with tampon use in which secondary vaginal ulcerations or erosions serve as an entry point for the organism. Withdrawal of highly absorbent tampons and polyacrylate rayon-containing products from the market partially explains the decrease in TSS; however, tampon use is still a risk factor. It may also occur postpartum, after a medical or missed abortion, C-section, surgical procedure, or carbon dioxide laser treatment, or skin, bone, or respiratory infections. Tampon-associated TSS is caused by Staphylococcus aureus , whereas S. aureus , Streptococcus pyogenes (group A Streptococci) , Clostridium sordellii , or Clostridium perfringens may be implicated in other settings.
In infections secondary to S. aureus the diagnosis is primarily clinical as blood cultures are positive in only approximately 5% of the cases. In contrast, in infections due to GAS, blood cultures are typically positive. Microscopically, mucosal hyperemia and/or ulceration can be noted. A Gram stain can demonstrate Gram-positive cocci (staphylococcal or group A streptococcal infections) or Gram-positive bacilli (clostridial infection). In clostridial infections, besides anaerobic culture, immunohistochemical studies using commercial polyclonal anti- Clostridium spp. antibody or PCR targeting a Clostridium specific gene have been used in formalin fixed tissue. Treatment includes clindamycin with or without penicillin and intravenous immunoglobulin G therapy.
Parasitic infections are rare in the United States, being more common in countries where the infection is endemic. Vaginal amebiasis is caused by Entamoeba histolytica ; patients usually present with bloody vaginal discharge and ulcerated and friable lesions. Microscopically, ulcerated squamous epithelium is associated with fibrinopurulent exudate containing trophozoites measuring 15–60 μm in diameter that stain with periodic acid-Schiff (PAS). Trophozoites can also be identified on wet smears from vaginal discharge. Metronidazole is the treatment of choice.
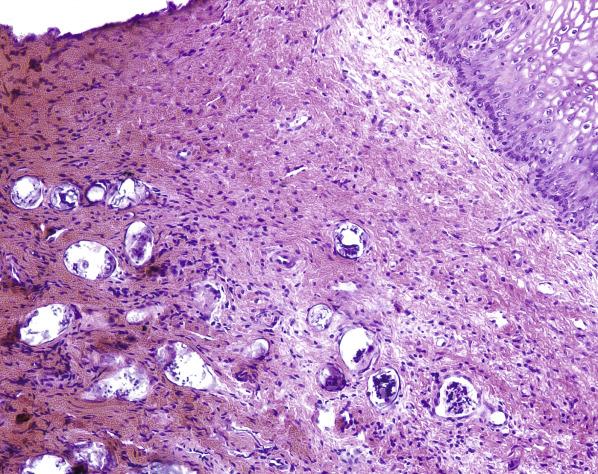
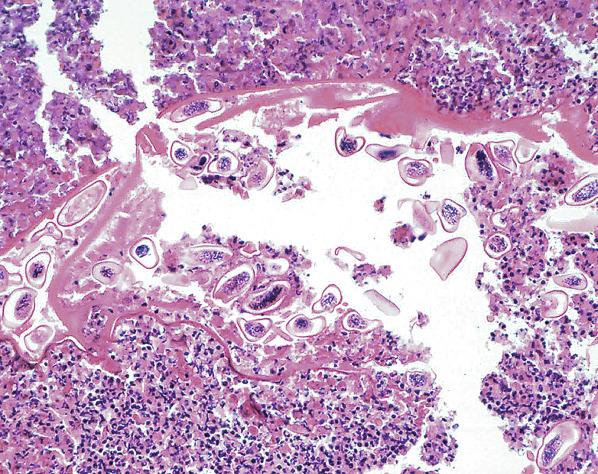
Infection by Schistosoma mansoni and Schistosoma haematobium commonly results in vaginal discharge, pruritus, and dyspareunia. Clinical examination may show polyps, ulcers, or “sandy patches” of the mucosa. The latter are visible by colposcopy. Microscopically, viable or nonviable eggs are usually seen in the submucosa, associated with a prominent inflammatory response (including eosinophils) that ultimately results in marked fibrosis ( Fig. 5.4 ). Praziquantel is the treatment of choice.
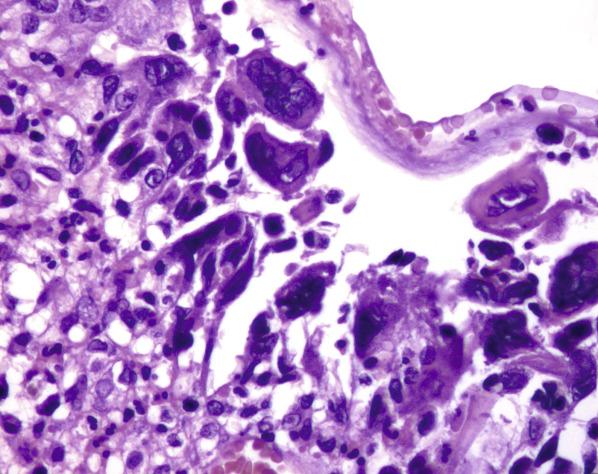
Eggs and worms of Enterobius vermicularis have also been found in the vagina, where they elicit a granulomatous reaction associated with central necrosis ( Fig. 5.5 ). Finally, eggs of Trichuris trichiura can be seen in the vagina as contamination in cases of intestinal infestation.
Vaginal involvement by tuberculosis is usually secondary to spread from pulmonary or renal disease with rare cases exclusively confined to the lower female genital tract. It tends to affect women of reproductive age, although it can also occur in postmenopausal women or in association with immunosuppression. Grossly, it may be seen as nodules or ulcers. Microscopically, it shows caseating granulomas containing acid-fast positive bacilli. Antituberculosis quadruple regimen is standard for this infection.
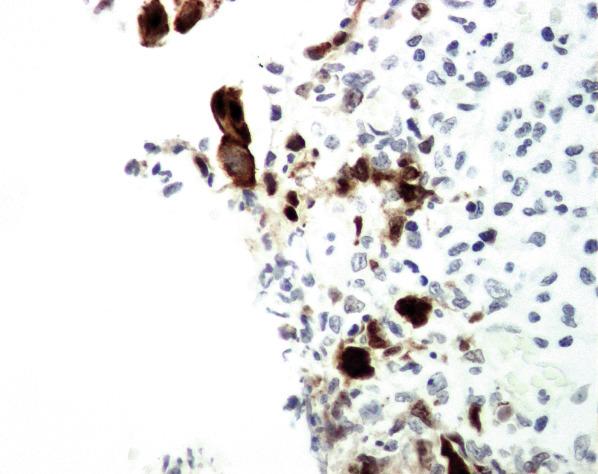
Genital infection by herpes simplex virus (HSV) often involves the vagina. The most common causative agent is herpes simplex virus type 2 (HSV-2) and, less frequently, herpes simplex virus type 1 (HSV-1). “Classic” outbreaks begin with a prodrome lasting 2–24 hours that includes regional pain or a burning sensation. In addition, patients may have fever, headache, malaise, lymphadenopathy, and anorexia. Subsequently, papules, vesicles, and erosions/ulcers appear over hours to days and can last from 2–6 weeks. The vesicles are usually asymptomatic, whereas the ulcers are very painful. Some patients can have intermittent bleeding and vaginal discharge. Recurrent HSV episodes are usually milder than the initial episode, typically with fewer lesions, and viral shedding occurs at a lower concentration and with shorter duration. Microscopically, there is prominent intracellular ballooning and reticular degeneration of the keratinocytes leading to intraepidermal vesicles, which may rupture and secondarily form ulcers. Acantholytic keratinocytes show nuclear molding, “ground-glass” or marginated chromatin, and sometimes multinucleation. Large eosinophilic nuclear inclusions surrounded by a pale halo (Cowdy A bodies) are less frequently seen ( Fig. 5.6 ). The characteristic viral cytopathic changes are more commonly identified at the edge of the ulcer. The diagnosis is based on histologic findings or cytology preparation of the scraping of the base and edges of a fresh ulcer (by Tzanck preparation, Diff-Quik, Papanicolaou or thin-prep, Wright). Immunohistochemistry (HSV1 and HSV2), in situ hybridization, or PCR for HSV can be used to confirm the diagnosis ( Fig. 5.7 ). Acyclovir and related compounds such as valacyclovir and famciclovir are used in the control of the outbreaks.
Cytomegalovirus (CMV) infection causes vaginal, cervical and vulvar ulcers in immunocompromised patients, in particular those with human immunodeficiency virus (HIV). Ulcers, either single or multiple, may be confined to the lower genital tract or coexist with oroesophageal ulcers. They are painful, range in size from 1 to 6 cm, are often deep, and occasionally progress to form fistulas. Infected epithelial and/or endothelial cells are typically enlarged and contain intranuclear and intracytoplasmic inclusions. Peripheral clearing of the chromatin imparts an “owl’s eye” appearance. Confirmation of CMV infection by immunohistochemistry can be performed. Patients tend to respond to topical or systemic steroids.
HSV type 2>type 1
Pain or burning sensation, vaginal discharge, or intermittent vaginal bleeding
Fever, malaise, lymphadenopathy, and anorexia may be seen
CMV-associated ulcers are painful
Acyclovir and related compounds if herpes
Topical or systemic steroids for ulcers in AIDS patients if CMV
Herpes virus infection: papules, vesicles and erosions/ulcers
CMV infection: ulcers in immunocompromised patients
HSV: Prominent intracellular ballooning and reticular degeneration of keratinocytes with intraepidermal vesicles
Nuclear molding, “ground-glass” chromatin +/- multinucleation
Large eosinophilic nuclear inclusions surrounded by pale halo (Cowdry A bodies) Confirmation by immunohistochemistry (HSV and HSV2) and PCR
CMV: Enlarged epithelial and/or endothelial cells
Intranuclear (“owl-eye”) and intracytoplasmic inclusions
Confirmation by immunohistochemistry
This is a rare, benign, self-limited disease of unknown cause that typically involves the vagina, although occasionally can also affect the ectocervix.
Patients range in age from 17 to 77 years. Symptoms, when present, include vaginal discharge or bleeding, pressure, pruritus, and a “popping” sound with intercourse or physical examination due to rupture of the gas-filled cysts.
The lesions, which range in size from a few millimeters to 2 cm, usually involve, but are not limited to, the upper two-thirds of the vagina. They are often evenly distributed but may form clusters. Individual lesions are tense, smooth, and discrete, although as they aggregate, the vaginal mucosa acquires a pebbled or granular appearance.
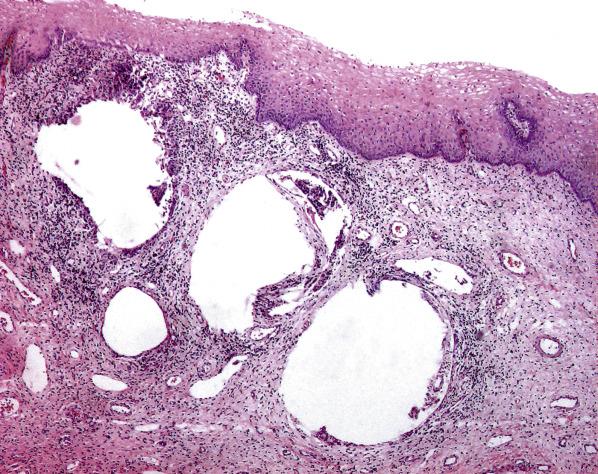
The hallmark of emphysematous vaginitis is the presence of variably sized pseudocystic spaces within the lamina propria. The walls are composed of fibroconnective tissue that may or may not contain multinucleated giant cells ( Fig. 5.8 ). The pseudocysts are usually empty but may occasionally contain eosinophilic material. The overlying squamous epithelium is intact but may show acanthosis. On occasion, there is associated chronic inflammation.
This benign lesion usually regresses spontaneously. However, superimposed infection (usually trichomoniasis or G. vaginalis ) requires treatment.
This is an uncommon form of chronic purulent vaginitis that may be immune-mediated.
It typically affects white women over a wide age range, with a peak in the perimenopause. Patients are typically symptomatic and have long standing complaints (usually >1 year before diagnosis) including purulent vaginal discharge, vulvovaginal burning sensation, dyspareunia, malodor, and vulvar pruritus. The vaginal pH is typically elevated (>4.5).
There is mucosal erythema and ecchymoses; the latter can also involve the vulva and cervix. Occasionally, erythematous papules with a pale center can be seen.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here