Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Noninvasive advanced technology liposculpting treatments are increasingly supplanting, complimenting, and preliminary to excisional body contouring surgery.
For optimal patient care and to maintain dominance in the body contouring market, a plastic surgeon needs to embrace reliable and safe technology, particularly for success in the office setting.
Formidable barriers are a vast array of options, high capital purchase, costly disposables, maintenance fees, lack of experience, conflicting anecdotal reports, energy-related complications, marketing hyperbole, and rapid obsolescence.
Competing marketed technologies have been rejected by plastic surgeons as being relatively ineffective, cost prohibitive, unsafe, or redundant compared to excisional surgery.
Non–plastic surgeons are usurping patients through marketing of energy-based technologies. Their advanced technology offers scarless, rapid recovery and safer and less-expensive alternative to surgery. Having only machines, these clinics oversell their limited therapeutics beyond appropriate indications.
Overweight and obese patients are encouraged to lose weight and are offered an alternative diet of human choriogonadotropin (HCG)/500 calorie-a-day 6-week program. Goal body mass index (BMI) for patients for realistic results using noninvasives in the office setting are in the 25 to 30 kg/m 2 range. Patients in the 30 to 35 kg/m 2 range may see results when combined with more aggressive liposculpting and are better suited to the outpatient surgery center setting.
Energy-based technologies may supplant invasive surgery for mild to moderate skin laxity; often referred to as the gap deformity, that is, not bad enough for major surgery, but bad enough to do something about. They are also available to those who refuse excisional surgery.
Energy-based technologies have a reasonable return on investment by high patient satisfaction, increased variety of therapeutic alternatives, and can lead to traditional body contouring surgery.
Traditional vacuum and syringe with cannula liposuction are used for limited liposuction, and fat harvest for small lipoaugmentation.
VASERlipo (Solta Medical, Bothell, WA) is used for moderate to large volume liposuction, and adipose harvest for grafting to minimize residual tissue trauma and maximize connective tissue and dermal shrinkage.
Bipolar radiofrequency in the form of skin surface Morpheus8 microneedling and subcutaneous fat, vessel coagulation, and collagen fiber shrinkage through FaceTite, BodyTite, and AccuTite shrink tissues reliably and safely rejuvenates and shrinks skin.
Major body contouring operations are being modified to permit detailed sculpturing by ancillary procedures are the same time.
Topical electromagnetic, laser, and radiofrequency therapies such as EmSculpt, TruSculpt, and SculpSure reliably and safely rejuvenate skin, subcutaneous tissue, and muscle.
As experts in body contouring surgery, plastic surgeons are ideally positioned to provide and refine new technology as it emerges in the marketplace. This combination is clearly in the interest of our patients, particularly since many practitioners who cannot offer invasive body contouring may not present ideal and clear alternatives to patients who are not strong candidates for noninvasives. Based on a conscientious effort to sift through competing manufacturers’ claims and our clinical cases, the authors present our chosen technologies and how we apply them to those concerned about their appearance.
Patients presenting for noninvasive or minimally invasive procedures vary widely, ranging anywhere from thin and wrinkled to obese with a hanging pannus. Naturally, these patients abhor their size, shape, bulges, unsightly scars, stria, and loose skin. In addition, larger patients are frequently concerned about oversized flanks and back, and sagging poorly shaped mons pubis, buttocks, and thighs. However, not all these patients will qualify for minimally invasive approaches. Overweight patients are encouraged to lose weight on their own or accept our preoperative 500-calorie-a-day diet/HCG injection 6-week program, but even after significant weight loss many will exceed the capacity of noninvasives. We discuss with the patient gender-specific contouring through artistic emphasis of shape to those both aware and ignorant of the differences.
As plastic surgeons, most patient discussion will involve invasive surgical options of removal of excess skin and fat, with patients’ responses ranging from disapproval of invasive surgery to acceptance of whatever operation and resulting scars it takes to obtain optimal result. Nevertheless, most inquirers for torso contouring not only welcome but are intrigued by non- and minimally invasive technology to supplant or augment recommended surgery. Even when they elect complex excisional operations, patients appreciate our experience and explanation of the alternatives, but, for them, ultimately inadequate procedures.
Patients readily grasp that in the process of correcting their perceived localized contour deformity, their entire torso could be recontoured. A common example is request for correction of gynecomastia. Beyond addressing the residual chest skin laxity, further masculinization can be achieved through liposuction with etching of torso musculature and lipoaugmentation of the pectoralis and deltoid muscles ( Fig. 8.1 ).

With or without excisional surgery, minimally invasive technology such as ultrasonic-assisted liposuction, bipolar radiofrequency skin tightening, and electromagnetic energy muscular enhancement remove adipose, damage collagenous support, and induce regeneration of connective tissue septi, dermis, and muscle. These patients may present primarily to the office requesting these technologies, particularly during effective office advertising campaigns, but this is often the exception and not the rule. Know when to integrate these technologies with precision to enhance or supplant other techniques.
Looking at the big picture, comprehensive contouring of the torso involves eight interactive tools. Complex and lengthy excisions may be complimented by preoperative weight reduction and intraoperative energy-based technologies. Items pertinent to non- or minimally invasive approaches are discussed in detail.
HCG/500-calorie-a-day diet to reduce excessively high BMI. ,
VASER ultrasound-assisted lipoplasty to debulk fat, undermine flaps or excision sites, and harvest adipose tissue. ,
BodyTite, FaceTite, bipolar radiofrequency to subcutaneous tissue for mild to intermediate surgical tissue laxity. ,
Morpheus8 Body with Burst bipolar radiofrequency microneedling to dermis and subdermis to tighten and rejuvenate skin.
Lipoabdominoplasty with or without lower body lift when flank/transverse laxity is absent.
Oblique flankplasty with lipoabdominoplasty (OFLA) to narrow a sagging waist, tighten the torso, and lift the buttocks and lateral thighs in cases of greater laxity, particularly in the female torso.
Oblique flankplasty with TULUA abdominoplasty allows for VASERlipo abdominal etching and lipoaugmentation, especially in the male. ,
J Torsoplasty with breast/chest reshaping to compliment OFLA or lower body lift.
High-frequency ultrasound (HFUS) for intraoperative tomographic guidance: autologous augmentation of positive contours and targeted peripheral nerve nonnarcotic pain control.
EmSculpt high-frequency electromagnetic energy (HIFEM) for natural muscular development and toning.
Topical but limited therapies for those who refuse minimally invasive procedures and invasive surgery such as TruSculpt, SculpSure.
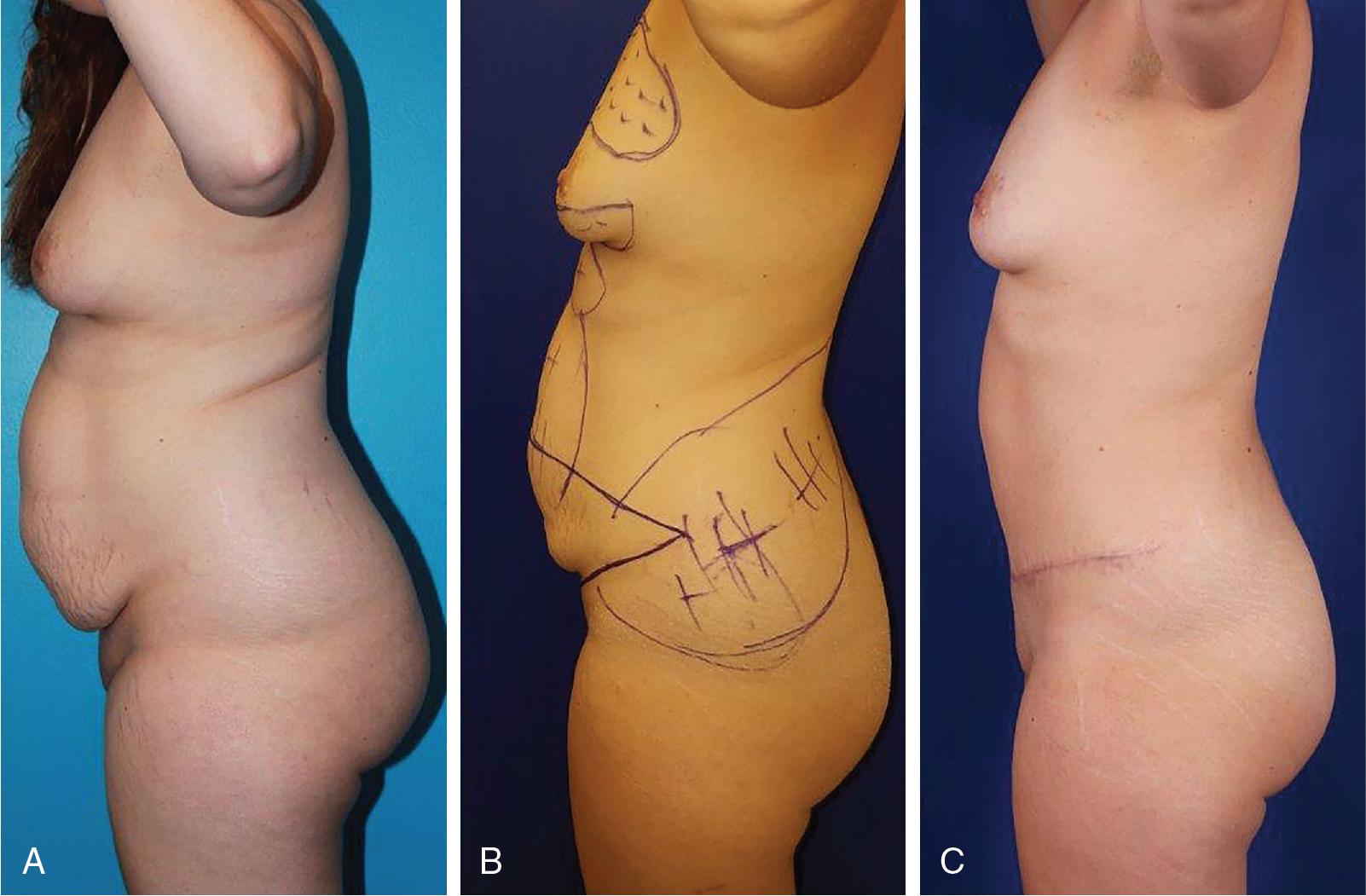
Overweight individuals, especially those with prominent intraabdominal girth, requesting body contouring are at increased risk for delayed healing and poor aesthetics. Rather than rejecting them, for the past 14 years Hurwitz center has offered a 500-calorie-a-day diet with daily injections of HCG that the senior author learned directly from plastic surgeon Hassan Tazia in Casablanca, Morocco. This high-protein, HCG-injection 6-week program was originated by Internist Alfred Simeon in Italy. , The HCG hormone induces visceral fat metabolism and reduces hunger for a weight loss of nearly a pound a day. Preoperatively treated, about 80% of the last 300 patients have lost enough weight to successfully proceed with extensive body contouring operations. Our demonstrative patient is a 32-year-old woman who lost 30 pounds on the HGC program to lower her BMI from 32 to 27 kg/m 2 ( Fig. 8.2 ). Her lipoabdominoplasty included imbrication of her diastasis recti and umbilical herniorrhaphy, plus VASERlipo of the flanks and lipoaugmentation of her breasts. Two years later, she has gained only 5 pounds, maintained her new figure with no recurrence of the hernia or diastasis recti. While significant rapid weight loss can precipitate significant tissue laxity that may transition a patient from minimally invasive to more invasive procedure, HCG is an important tool that can assist a patient to meet their final goal before a procedure.
Because of poor compliance, approximately 20% of users are unable to lose to goal weight. We have avoided patients with unstable endocrine disorders but have often treated patients with stable diabetes and patients on hypertensives without adverse sequalae. About 10% of successfully treated patients request a repeat 6-week diet to treat their postsurgical weight gain.
Limiting to no more than two consecutive 6-week treatments, there have been no metabolic or medical adverse events. The visceral fat target has led to loss of intraabdominal fat, which explains no recurrence of repaired diastasis recti. While patients on HCG/500-calories-a-day diet have increased energy and libido, they are being starved and should not undergo surgery until 1 week after completing the program to avoid delays in wound healing.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here