Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The urogenital system has two major subdivisions: (1) the urinary tract, which is responsible for the production, storage, and elimination of urine, and (2) the genital tract, which is involved in reproductive activity. Many functions of the urogenital system are controlled by complex neural pathways in the brain and spinal cord. These central pathways in turn regulate the activity of peripheral autonomic (sympathetic and parasympathetic) and somatic nerves that innervate the smooth muscle, striated muscle, epithelial cells, and exocrine glands in the urogenital organs. Some urogenital functions (penile erection) are purely involuntary and mediated by reflex pathways in the spinal cord or brainstem; whereas others (micturition) are more complex involving voluntary control by the cerebral cortex. This article will review the innervation, central neural circuitry, and neurotransmitters controlling urogenital functions.
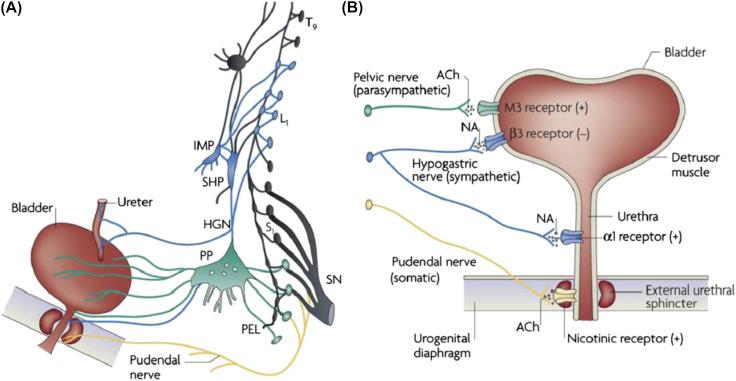
The lower urinary tract and sex organs are innervated by three sets of peripheral nerves that arise at the level of the lumbosacral spinal cord ( Fig. 121.1 ). Visceral structures (urinary bladder, urethra, cavernous tissue of the penis and clitoris, vas deferens, and exocrine glands) receive an innervation from both divisions of the autonomic nervous system. Parasympathetic efferent axons that originate in preganglionic neurons in the sacral spinal cord pass through the pelvic nerves to synapse with peripheral autonomic ganglion cells that in turn innervate the organs. Sympathetic efferent axons that originate in preganglionic neurons in the rostral lumbar segments of the spinal cord project to autonomic ganglion cells in the prevertebral and paravertebral ganglia which then send axons through various nerves to the target organs. Somatic efferent axons originate in motor neurons in the sacral spinal cord and pass through the pudendal nerves to striated muscles of the urethral sphincter ( Fig. 121.1B ) and periurethral striated muscles (bulbocavernous and ischiocavernosus) ( Table 121.1 ).
| Response | Afferent Nerves | Efferent Nerves | Central Pathway | Effector Organ |
|---|---|---|---|---|
| Penile erection | ||||
| Reflexogenic | Pudendal nerve | Sacral parasympathetic | Sacral spinal reflex | Dilatation of arterial supply to corpus cavernosum and corpus spongiosum |
| Psychogenic | Auditory, imaginative, visual, olfactory | Sacral parasympathetic, lumbar sympathetic | Supraspinal origin | |
| Glandular secretion | Pudendal nerve | Sacral parasympathetic, lumbar sympathetic | Sacral spinal reflex | Seminal vesicles and prostate |
| Seminal emission | Pudendal nerve | Lumbar sympathetic | Intersegmental spinal reflex (sacrolumbar) | Contraction of vas deferens, ampulla, seminal vesicles, prostate, and closure of bladder neck |
| Ejaculation | Pudendal nerve | Somatic efferents in pudendal nerve | Sacral spinal reflex | Rhythmic contractions of bulbocavernosus and ischiocavernosus muscles |
Afferent axons innervating the urogenital organs arise in the lumbosacral dorsal root ganglia and are contained in the three sets of peripheral nerves. The most important afferents for initiating micturition are those, which travel in the pelvic nerve to the sacral spinal cord ( Fig. 121.2 ). These afferents are small myelinated (A–δ) and unmyelinated (C) axons that convey impulses from tension receptors and nociceptors in the bladder wall ( ). Afferent activity arising from mechanoreceptors in the penis and clitoris is carried in the pudendal nerves ( Table 121.1 ).
Parasympathetic pathways induce a bladder contraction, urethral relaxation, penile erection, clitoral engorgement, and glandular secretions. Sympathetic pathways relax the bladder, contract the bladder neck and urethra ( Fig. 121.1 ), produce seminal emission, and can elicit penile erection or detumescence ( Table 121.1 ). Motor axons in the pudendal nerves activate bulbocavernous and ischiocavernosus muscles and elicit ejaculation ( Table 121.1 ).
Parasympathetic neuroeffector transmission in the bladder is mediated by acetylcholine (Ach) acting on postjunctional muscarinic receptors ( Fig. 121.1B ). Both M 2 and M 3 muscarinic receptor subtypes are expressed in bladder smooth muscle; however, studies with subtype selective muscarinic receptor antagonists and muscarinic receptor knockout mice have revealed that the M 3 subtype is the principal receptor involved in excitatory transmission.
In bladders of various animals, stimulation of parasympathetic nerves also produces a noncholinergic contraction that is resistant to muscarinic receptor blocking agents. Adenosine triphosphate (ATP) elicits the noncholinergic contraction by acting on P2X 1 receptors. Although purinergic excitatory transmission is not important in the normal human bladder it has been identified in bladders from patients with pathological conditions such as idiopathic detrusor instability or interstitial cystitis ( ).
Smooth muscle contractions are initiated by an increase in intracellular Ca 2+ concentration, which can occur by intracellular release of Ca 2+ from the sarcoplasmic reticulum or by influx of Ca 2+ from the extracellular fluid ( ). The former mechanism is an essential step in the cholinergic activation of the detrusor muscle; while activation of P2X purinergic receptors causes the influx of extracellular Ca 2+ as well as depolarization of the cells leading to an opening of voltage gated Ca 2+ channels. This triggers intracellular Ca 2+ -induced Ca 2+ release from the sarcoplasmic reticulum. Activation of M 2 muscarinic receptors also appears to enhance contractions by suppressing β adrenergic inhibitory mechanisms by blocking adenylyl cyclase or K + channels.
Parasympathetic pathways to the urethra induce relaxation during voiding by releasing nitric oxide (NO). NO increases the levels of cyclic guanosine monophosphate (GMP) by stimulating guanylyl cyclase. Cyclic GMP in turn activates protein kinase G that produces smooth muscle relaxation by several mechanisms including activation of potassium channels and desensitization of the contractile machinery to Ca 2+ ( ).
Sympathetic postganglionic nerves that release norepinephrine provide an excitatory input to smooth muscle of the urethra and bladder base, an inhibitory input to smooth muscle in the body of the bladder ( Fig. 121.1B ), as well as inhibitory and facilitatory input to bladder parasympathetic ganglia ( ). The smooth muscle of the bladder base is richly innervated by adrenergic terminals, but the bladder body has a considerably weaker adrenergic innervation. α-adrenergic receptors are concentrated in the bladder base and proximal urethra, whereas β-adrenergic receptors are most prominent in the bladder body ( Fig. 121.1B ). These observations are consistent with pharmacological studies showing that sympathetic nerve stimulation or exogenous catecholamines produce β 3 -adrenergic receptor-mediated inhibition of the body and strong α 1 -adrenergic receptor-mediated contractions of the base and urethra as well as weaker contractions of the bladder body ( ). The α 1A -adrenergic receptor subtype is most prominent in the normal bladders but the α 1D -subtype is upregulated in bladders from patients with outlet obstruction due to benign prostatic hyperplasia. This finding raised the possibility that enhanced α 1 -adrenergic receptor excitatory mechanisms in the bladder body might contribute to irritative lower urinary tract symptoms in patients with prostate disease.
Activation of β-adrenergic receptors in bladder smooth muscle stimulates adenylyl cyclase and increases cyclic AMP which in turn activates protein kinase A. Protein kinase A is thought to act in part by inducing a hyperpolarization of the cells either by opening of K + channels or by stimulating an electrogenic ion pump. Excitatory responses in the urethra and bladder neck mediated by α 1 -adrenergic receptors are attributed to an increased release of Ca 2+ from intracellular stores.
Motor axons innervating the periurethral striated muscles, pelvic floor muscle, and the striated muscles mediating ejaculation release acetylcholine which activates nicotinic cholinergic receptors.
Postganglionic axons which control erectile tissue in the penis and secretion from seminal vesicles, prostate, and urethral glands synthesize and release several transmitters including NO, ACh, vasoactive intestinal polypeptide (VIP), and ATP. NO is the major transmitter mediating neurally induced erections ( Table 121.1 ); whereas ACh appears to be involved in stimulating glandular secretion. The functions of VIP and ATP are uncertain.
Penile erection is a vascular phenomenon resulting from neurally mediated increase in blood flow to the penile erectile tissue (corpora cavernosa and corpus spongiosum). The erectile tissue consists of large venous sinuses that contain very little blood when the penis is flaccid, but distend considerably when blood flow is increased. Dilation in the arterial supply to the cavernous tissue coupled with a relaxation of the sinusoidal smooth muscle in the trabecular tissue is responsible for erection.
Activity in both sacral (parasympathetic) and the thoracolumbar (sympathetic) preganglionic axons can activate postganglionic neurons that express neuronal nitric oxide synthase (nNOS) and release NO which elicits erections ( ). The endothelial cells in the penis also express endothelial nitric oxide synthase (eNOS) and can release NO in response to mechanical stimuli (shear stress) associated with changes in blood flow ( ). NO directly activates soluble guanylyl cyclase in the penile smooth muscle to increase the formation of cyclic GMP which in turn induces smooth muscle relaxation via activation of cyclic GMP-dependent protein kinases. The effects of NO are terminated by the enzymatic breakdown of cyclic GMP by phosphodiesterase. Pharmacologic studies in animals have shown that erections elicited by stimulation of autonomic nerves are reduced by NOS inhibitors and enhanced by phosphodiesterase (PDE) inhibitors ( ).
eNOS has also been implicated in neurally mediated erections. While erections are initiated by NO synthesized in nerves by nNOS, this mechanism triggers a transient increase in blood flow and expansion of the penile vasculature and sinusoidal spaces. However, the resulting shear force on the endothelium activates a phosphatidylinositol 3-kinase pathway that in turn stimulates a serine/threonine protein kinase, causing direct phosphorylation of eNOS and synthesis of NO ( ).
The sympathetic noradrenergic innervation of the penis that provides an excitatory input to penile blood vessels is thought to be involved primarily in detumescence ( Table 121.1 ). Electrical stimulation of sympathetic axons in either the hypogastric or pudendal nerves in various species produces a substantial reduction in penile blood flow. The effect is blocked by α-adrenergic receptor blocking agents. Several mechanisms have been implicated in the noradrenergic vasoconstrictor effect including: (1) prejunctional inhibition of parasympathetic nitrergic nerve terminals mediated by α 2 adrenergic receptors; (2) activation of postjunctional α 2 adrenergic receptors which then inhibits adenylate cyclase and formation of cyclic AMP; (3) activation of postjunctional α 1 adrenergic receptors stimulates phospholipase C activity followed by formation of IP 3 and diacylglycerol, leading to release of intracellular Ca +2 as well as sensitization of contractile mechanisms to Ca +2 ( ).
Afferent pathways that initiate the sensation of bladder fullness, the desire to void, and pain are small myelinated (Aδ) and unmyelinated (C) fibers that pass through the pelvic nerve to the sacral spinal cord ( ). Aδ bladder afferents in the cat respond in a graded manner to passive distension as well as active contraction of the bladder and exhibit pressure thresholds in the range of 5–15 mmHg, which are similar to those pressures at which humans report the first sensation of bladder filling. These fibers also code for noxious stimuli in the bladder. On the other hand, C-fiber bladder afferents in the cat have very high thresholds and commonly do not respond to even high levels of intravesical pressure. However, mechanosensitivity in some of these afferents is unmasked or enhanced by chemical irritation of the bladder mucosa. These findings indicate that C-fiber afferents in the cat have specialized functions, such as the signaling of inflammatory or noxious events in the lower urinary tract. C-fiber afferents are responsive to the neurotoxins, capsaicin, and resiniferatoxin, which have been used to desensitize the afferents and to treat bladder pain and afferent-evoked bladder overactivity. In the rat, A-fiber and C-fiber bladder afferents are not distinguishable on the basis of stimulus modality; thus both types of afferents consist of mechanosensitive and chemosensitive populations ( ). . Nociceptive and mechanoceptive information is also carried in the hypogastric nerves to the thoracolumbar segments of the spinal cord. Recent anatomical tracing studies in rats have also identified an additional afferent innervation of the bladder passing through the vagus nerves from sensory neurons in the nodose ganglion ( ). The function of this afferent pathway is not known.
Mechanosensitive afferents with receptors in the wall of the urethra and which detect urine flow pass through the pudendal nerves to the sacral spinal cord. Nociceptive afferents innervating the urethra pass through pudendal, pelvic, and hypogastric nerves to the lumbosacral spinal cord.
Afferents release rapidly acting excitatory transmitters (glutamic acid and ATP) which are involved in synaptic transmission in the spinal cord and also slowly acting neuropeptide transmitters (CGRP, VIP, pituitary-adenyl cyclase activating peptide [PACAP], tachykinins, and opioid peptides) which can be released at central as well as peripheral afferent terminals ( ). Many of these substances as well as others such as NO, prostaglandins, and neurotrophic factors released in the bladder by urothelial cells and inflammatory cells can modulate afferent sensitivity and change the response to mechanical stimuli.
The urothelium not only functions as a passive barrier at the bladder luminal surface but also appears to have specialized sensory and signaling properties that allows it to respond to chemical and mechanical stimuli and to engage in reciprocal chemical communication with nerves in the bladder wall ( ). These properties include: (1) expression of nicotinic, muscarinic, tachykinin, adrenergic, and capsaicin (TRPV1) receptors; (2) close physical association with afferent nerves and responsiveness to transmitters released from these nerves; (3) ability to release chemical mediators that can regulate the activity of adjacent nerves ( ) and thereby trigger local vascular changes and/or reflex bladder contractions.
The role of ATP in urothelial-afferent communication has attracted considerable attention because bladder distension releases ATP from the urothelium and intravesical administration of ATP induces bladder hyperactivity, an effect blocked by administration of P2X purinergic receptor antagonists that suppress the excitatory action of ATP on bladder-afferent neurons. Mice in which the P2X 3 receptor was knocked out exhibited hypoactive bladder activity and inefficient voiding, suggesting that activation of P2X 3 receptors on bladder-afferent nerves by ATP released from the urothelium is essential for normal bladder function ( ). It has also been reported that urothelial cells obtained from patients or cats with a chronic painful bladder condition (interstitial cystitis) released significantly larger amounts of ATP in response to mechanical stretching than urothelial cells from normal patients ( ). This raises the possibility that ATP-mediated signaling between the urothelium and afferent nerves is involved in the triggering of painful bladder sensations.
The mechanosensitive afferent receptors in the glans penis are primarily free nerve endings with a density higher than in any other area of the body ( ). In humans, most of the afferents innervating the penis are of the A-fiber and C-fiber type.
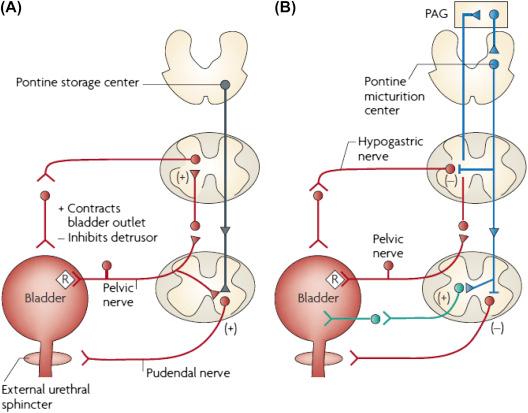
The reflex circuitry controlling the urogenital organs consists of four basic components: primary afferent neurons, spinal efferent neurons, spinal interneurons, and neurons in the brain that modulate spinal reflex pathways.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here