Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The diagnosis of disorders of the neuromuscular system involves localizing the lesion anatomically and then weighing the validity of specific diagnostic hypotheses. Symmetry and rapidity of the disease process are major diagnostic considerations. Pure motor syndromes localize to the anterior horn cells, neuromuscular junctions, or muscles, though, rarely, neuropathies can also produce pure motor deficits. Combinations of motor and sensory deficits suggest radiculopathy, plexopathy, or neuropathy.
A diagnostic strategy complementary to the aforementioned approach employs pattern matching. Neuromuscular diseases present with one of five basic patterns ( Table 60-1 ). Weakness is usually a more prominent feature of demyelinating than axonal neuropathies.
| Acute Generalized Weakness |
| Guillain–Barré syndrome |
| Botulism |
| Necrotizing myopathy |
| Tick paralysis |
| Severe electrolyte imbalance |
| Periodic paralysis |
| Subacute or Chronic Generalized Weakness |
| Amyotrophic lateral sclerosis |
| Demyelinating motor neuropathies |
| Myopathy |
| Myasthenia gravis |
| Slowly Progressive, Generalized Weakness More Than Numbness |
| Demyelinating polyneuropathy |
| Slowly Progressive, Distal Numbness More Than Weakness |
| Axonal polyneuropathy |
| Numbness, Weakness, or Pain Limited to One Limb |
| Radiculopathy |
| Plexopathy |
| Entrapment neuropathy |
| Initial nerve involved by vasculitic neuropathy |
In general, electromyography (EMG) and nerve conduction studies (NCSs) are essential for confirming the anatomic localization, differentiating axonal from demyelinating neuropathies, and making prognostic statements. Decisions concerning the need for muscle or nerve biopsies should be deferred until electrodiagnostic testing is completed.
Amyotrophic lateral sclerosis (ALS) is the most common and prototypic motor neuron disease. It presents with flaccid weakness and atrophy of muscles without associated pain or sensory disturbances. Degeneration of upper motor neurons also occurs, producing spasticity and hyperreflexia in wasted limbs. Most cases are sporadic, but approximately 10 percent are inherited in autosomal-dominant or -recessive patterns. The pathogenesis of ALS is not known, but it is possible that multiple pathogenic mechanisms are at play, including impaired cellular handling of oxidative stress, neuroinflammation, neurotrophic factor deficiency, glutamate-induced excitotoxicity, and defects in protein metabolism and autophagy. There is no cure for ALS, although riluzole and edavarone modestly slow progression of disease. Noninvasive ventilation, careful nutritional monitoring and supplementation, and multidisciplinary care can improve the quality of life. A sporadic clinical variant characterized by solely lower motor neuron involvement (progressive muscular atrophy) is managed similarly.
Hereditary anterior horn cell diseases include spinal muscular atrophy (SMA), Kennedy syndrome, and hexosaminidase A deficiency. Biallelic mutations or deletions in the SMN1 gene cause SMA. The copy number of a nearly identical gene, SMN2 , on the same chromosome as SMN1 determines the disease severity and age of onset. Intravenous SMN1 gene replacement using a viral vector and an intrathecally administered antisense oligonucleotide therapy have been approved for this condition. Kennedy disease (spinal and bulbar muscular atrophy) is an X-linked disease characterized by proximal muscle weakness, muscle atrophy, and fasciculations, especially periorally. Affected individuals often have gynecomastia and testicular atrophy with reduced fertility. Expansion of a CAG repeat in the androgen receptor gene is responsible.
Compression of the spinal cord may result in segmental loss of anterior horn cells. In cervical spondylosis, combined injury to both the anterior horn cells and descending corticospinal tracts may occur, leading to atrophy and weakness in the hands combined with spastic paraparesis; such a presentation mimics that of ALS.
Many viruses have central nervous system (CNS) tropism, but only a few strains cause acute and selective loss of anterior horn cells. Poliovirus is an enterovirus spread via a fecal–hand–oral route. Most patients are either asymptomatic or develop only mild constitutional symptoms. More severe signs and symptoms may occur in nonparalytic poliomyelitis, and the cerebrospinal fluid (CSF) findings are often indicative of aseptic meningitis. Individuals developing acute paralytic poliomyelitis experience constitutional symptoms but also develop rapidly progressive weakness over the course of one to a few days. Weakness is often focal and asymmetric in the limbs or bulbar muscles, but may be symmetric or generalized. It frequently improves over several weeks to months. Rarely, the live-attenuated oral poliovirus vaccine can cause paralytic poliomyelitis. In the United States, an inactivated poliovirus vaccine is used, which does not carry the risk of vaccine-associated poliomyelitis.
Postpolio syndrome consists of slowly progressive new or worsened weakness, together with fatigue or pain in the muscles or joints, typically occurring many years after acute paralytic poliomyelitis in about 20 to 40 percent of individuals. The pathogenesis may involve late denervation of previously reinnervated muscle fibers or musculoskeletal abnormalities.
Viruses other than poliovirus, such as West Nile virus (WNV), echovirus, coxsackievirus, herpes zoster virus, and Epstein–Barr virus may also cause loss of motor neurons. Only about 20 percent of WNV infections are symptomatic, usually manifesting as a febrile illness. A maculopapular rash is common. About 1 percent of infected individuals develop neurologic symptoms that may include meningoencephalitis, flaccid paralysis, or both. As in poliovirus infection, the weakness is often proximal and asymmetric, with no significant sensory abnormalities. The CSF shows a lymphocytic or neutrophilic pleocytosis (30 to 150 cells/mm 3 ) and high protein content. CSF and serum should be screened for IgM antibodies to WNV. Adding WNV polymerase chain reaction (PCR) testing of both the serum and CSF can increase the diagnostic yield. Treatment is supportive. Rarely, WNV may present with brachial plexopathy, rhabdomyolysis, or a predominantly demyelinating polyneuropathy similar to Guillain–Barré syndrome (GBS).
Paraneoplastic lower motor neuron involvement may occur rarely with lymphoproliferative disorders, thymoma, and various cancers (bronchial, ovarian, renal, and prostate). Patients may have anti-Hu (ANNA-1) and anti-Yo (PCA-1) antibodies, CSF protein level is often elevated, and there is a variable CSF pleocytosis. The weakness may improve after treatment of the cancer.
Pain or numbness in a dermatomal pattern accompanied by weakness in a segmental pattern suggests a radiculopathy. External compression is the most frequent cause of nerve root injury, by either intervertebral disc herniation or spondylosis. Radiculopathy resulting from degenerative spine disease is discussed further in Chapter 22 . Other causes of radiculopathy may include gouty spine disease, Paget disease, Tarlov cysts, and methylacrylate extrusion during spine surgery. Extradural tumors such as schwannomas, neurofibromas, and meningiomas may also produce a radiculopathy. A radiculopathy sometimes results from epidural or spinal anesthesia; the injury may result from direct trauma to the nerve or from chemical injury related to the injected substance.
Diabetic thoracoabdominal radiculopathy (diabetic truncal neuropathy) is a common cause of noncompressive radiculopathy. Patients present with pain and hyperalgesia in a region along the chest or abdomen. The pattern of involvement may be clearly dermatomal, but often the changes span more than one segment. Segmental weakness may manifest as an outpouching of the abdominal wall. The pathophysiology is unclear, but an inflammatory vasculopathy may be responsible.
Compression of multiple lumbosacral nerve roots produces a cauda equina syndrome, which may lead to permanent urinary and fecal incontinence and lower extremity weakness and numbness and thus constitutes a neurosurgical emergency. The usual cause is a large, midline disc herniation. Chronic cauda equina syndrome may be caused by a developmental anomaly, such as a tethered spinal cord.
Spondylosis is the most common cause of polyradiculopathy, although metastatic spinal disease should also be considered. Cancers of the breast, lung, prostate, or kidney, or multiple myeloma metastasize most frequently to the spine. Polyradiculopathy results from direct tumor compression or from leptomeningeal infiltration of the roots by tumor cells (neoplastic meningitis). Treatment of spinal bony metastases often involves external beam irradiation, although decompressive surgery may be necessary in radiation-resistant tumors.
Carcinomatous meningitis often affects the caudal roots first. Cranial neuropathies, meningeal signs and symptoms, and a myelopathy may be associated features. CSF analysis typically shows a pleocystosis, hypoglycorrhachia, elevated protein level, and malignant cells on cytologic analysis. The yield of positive cytology for malignant cells is increased significantly by repeating the lumbar puncture. Treatment is usually palliative and includes radiation therapy and intrathecal chemotherapy. The median survival of patients with leptomeningeal metastases is 4 months.
Infectious causes of polyradiculopathy include cytomegalovirus (CMV), Borrelia burgdorferi (Lyme disease), Epstein–Barr virus, herpes simplex virus, Mycobacterium tuberculosis , and Treponema pallidum . CMV polyradiculopathy usually presents as a late complication of acquired immunodeficiency syndrome (AIDS), but it can be a presenting manifestation of human immunodeficiency virus (HIV) infection. The onset of flaccid paraparesis, lower extremity numbness, and urinary retention may be acute or subacute. A neutrophilic pleocytosis on CSF analysis is a clue to the diagnosis; the diagnosis is confirmed by a culture or CMV DNA PCR assay on CSF. Treatment includes ganciclovir, foscarnet, or both.
Arachnoiditis is a nonspecific term for inflammation of the spinal leptomeninges. Historically, arachnoiditis has been associated with tuberculous and syphilitic meningitis and with obsolete oil-based contrast agents for myelography. Currently, the term often refers to the appearance of thickened meninges and clumping of the nerve roots on magnetic resonance imaging (MRI) of the spine, usually in patients who have undergone lumbar spine surgery. There is controversy about the association of the imaging findings, clinical findings, and symptoms. Arachnoiditis has also been described in association with toxoplasmosis and subarachnoid hemorrhage; sometimes the cause is not known.
Diffuse or regional impairment of tactile sensation or gait ataxia without weakness suggests degeneration of posterior root ganglia cells (sensory neuronopathy). Patients may also have facial numbness and autonomic involvement, manifesting as gastroparesis, orthostatic hypotension, sexual impairment, and Adie pupils. EMG and NCSs differentiate sensory neuronopathies from more common distal sensory axonal polyneuropathies. Sensory neuronopathies may be acquired ( Table 60-2 ) or hereditary.
| Autoimmune |
| Autoimmune chronic active hepatitis |
| Paraneoplastic syndrome |
| Sjögren syndrome |
| Idiopathic |
| Infectious |
| Epstein–Barr virus infection |
| Human immunodeficiency virus infection |
| Rickettsia conorii infection |
| Varicella zoster infection |
| Nutritional |
| Nicotinic acid deficiency |
| Pyridoxine deficiency |
| Vitamin E deficiency |
| Toxic |
| ? Antibiotic-related |
| Cisplatin |
| Pyridoxine |
| Thalidomide |
Paraneoplastic sensory neuronopathy (see Chapter 27 ) is commonly associated with small cell lung cancer but also occurs with breast or ovarian cancer, Hodgkin lymphoma, neuroendocrine tumors, and sarcoma. Symptom onset is generally subacute. Antibodies to the Hu antigen (ANNA-1) are usually present, but their absence does not exclude the possibility of paraneoplastic sensory neuronopathy. Antibodies to the collapsin response-mediator protein 5 (CRMP5) have also been described in some patients with small cell lung cancer. Sensory neuronopathy may occur with other paraneoplastic syndromes. Management is directed to the diagnosis and treatment of the underlying cancer. Treatment of the paraneoplastic condition with intravenous immunoglobulin (IVIg), plasmapheresis, or other immunosuppressive therapies is often disappointing.
Autoimmune or inflammatory conditions associated with sensory neuronopathy (sometimes as the initial manifestation) include Sjögren’s syndrome and autoimmune hepatitis. The posterior root ganglia of patients are infiltrated by T lymphocytes. IVIg and plasmapheresis have benefited some patients.
An acute sensory neuronopathy syndrome characterized by the acute onset of widespread sensory symptoms, areflexia, impaired vibratory sensation, and gait ataxia has developed 4 to 12 days after initial antibiotic treatment for a febrile illness. The underlying pathogenesis in such cases may be infectious, postinfectious, or toxic (related to antibiotic use).
Infectious causes of sensory neuronopathy are shown in Table 60-2 . HIV infection may cause a sensory neuronopathy. T-cell infiltration of dorsal root ganglia has been found in patients with end-stage AIDS. Many of these patients also have pallor of the cervical portion of the gracile tract at autopsy, suggesting that a “dying-back” axonopathy occurs along with sensory neuron loss.
Latent infection of the dorsal root ganglia occurs following primary varicella zoster virus infection. When cell-mediated immunity is compromised, reactivation of viral replication causes the clinical syndrome of herpes zoster. The elderly, transplant recipients, and HIV-positive patients are particularly vulnerable. The prodromal stage of herpes zoster includes fevers, dysesthesias, and malaise. Several days later, a vesicular eruption appears in a dermatomal distribution. Pathologically, there is intense inflammation of the dorsal root ganglia. Once the lesions become encrusted, they are no longer infectious. Approximately 3 percent of patients develop segmental paresis, perhaps from spread of the virus to the anterior horn cells. Most patients recover muscle strength with time. Treatment during the early stages of infection includes acyclovir, valacyclovir, or famcyclovir. Postherpetic neuralgia may occur, particularly in the elderly. Tricyclic drugs or anticonvulsants are effective treatments, as discussed in Chapter 42 . Patients age 50 and older with a history of herpes zoster and immunocompetent patients age 60 or older without a history of herpes zoster should receive the zoster vaccine.
A number of toxins and vitamin deficiencies cause sensory neuronopathy. Because many of these also cause an axonopathy, they are discussed later (pp. 1071–1073).
Hereditary sensory neuronopathy (hereditary sensory and autonomic neuropathy) is both genetically and phenotypically heterogeneous; some forms present with predominantly small-fiber involvement, whereas others have mixed small- and large-fiber involvement. There is variable involvement of the autonomic nervous system. Commercial genetic testing is available for some types.
Trauma and compression, including at childbirth, cause most plexus injuries; other causes include tumor infiltration, postirradiation injury, and infection. An autoimmune monophasic neuritis, often idiopathic but sometimes associated with diabetes mellitus, may involve portions of either the brachial or lumbosacral plexus.
Sports, motorcycle, and industrial accidents cause traction injury to the brachial plexus. If the arm is located at the side of the patient at the time of impact or is distracted away from the torso, the upper roots and plexus are preferentially injured. If the arm is elevated above the head, the lower trunks and roots are most vulnerable. Compression injury of the brachial or lumbosacral plexus may occur during surgery or coma or from mass lesions such as a hematoma or tumor.
Immune brachial plexopathy (brachial plexus neuritis, neuralgic amyotrophy, Parsonage–Turner syndrome) is an acute monophasic neuropathy that presents with severe shoulder pain accompanied by muscle weakness and atrophy. Both sporadic and hereditary forms exist. Proximal muscle groups are more commonly affected than distal ones; involvement may be either unilateral or bilateral. Sensory loss is mild. Ipsilateral diaphragmatic weakness sometimes occurs from phrenic nerve involvement. Nerve biopsy specimens have revealed perineurial thickening and perivascular inflammatory infiltrates. Corticosteroids or IVIg, or both, have been used in treatment with anecdotally reported success, but controlled studies are needed. Aggressive treatment to control pain is important. The prognosis is excellent, with 60 percent of patients recovering completely within 1 year and 80 percent within a few years.
Nondiabetic lumbosacral radiculoplexus neuropathy refers to a similar disorder that affects the lower extremities. As with immune brachial plexus neuropathy, pain is often the initial symptom. It may occur in the back, buttock, thigh, or leg. Proximal weakness is more common than distal weakness. In time, however, the weakness often becomes more diffuse in the limb, and bilateral involvement is common. Clinically, sensory deficits (despite the pain) tend to be relatively mild. Nerve biopsies have shown evidence of ischemic injury and epineurial perivascular inflammatory collections. Some improvement in strength occurs with time but long-standing motor deficits are common. Case reports suggest a potential benefit of corticosteroids, plasmapheresis, or IVIg therapy, but no positive controlled trials have been published. Diabetic lumbosacral radiculoplexopathy (proximal diabetic neuropathy; diabetic amyotrophy) is discussed in Chapter 19 .
Breast and lung cancers are the two most common secondary neoplasms to infiltrate the brachial plexus. Gastrointestinal and genitourinary cancers, melanomas, and lymphomas may also metastasize to the brachial plexus. Colorectal cancer is the most common neoplasm to infiltrate the lumbosacral plexus, but uterine, prostate, and ovarian cancer may also do so; other neoplasms may spread to the lumbosacral plexus metastatically.
Radiation therapy that includes the plexus in the field (as for breast cancer) may produce delayed weakness, dysesthesias, and numbness in the affected limb ( Chapter 28 ). Irradiation causes marked fibrosis of the nerve fibers, loss of myelin, and destruction of the vascular supply. The period between the radiation treatment and onset of symptoms ranges from a few weeks to more than 30 years. Paresthesias in the median-innervated digits are a common initial symptom. Subsequently, weakness of the intrinsic hand muscles develops. Prominent limb pain and a Horner syndrome suggest tumor involvement rather than radiation-induced injury, whereas the presence of fasciculation potentials and myokymia on needle EMG suggests radiation injury. Distinction of these two disorders is aided by MRI.
Patients with radiation-induced lumbosacral plexopathy have generally been treated for lymphoreticular, testicular, uterine, or ovarian cancer. Patients usually present with slowly progressive distal weakness; numbness or paresthesia is less common. Mild pain occurs in 50 percent of patients. The CSF protein concentration may be elevated. As with radiation-induced brachial plexopathy, the condition may stabilize, but patients are often disabled.
Finally, a lower motor neuron syndrome affecting the legs, with relatively intact sensation, may also occur following irradiation of the distal spinal cord and cauda equina. Patients have generally received more than 40 Gy. Pathologic examination of the cauda equina shows a vasculopathy of the proximal nerve roots. Although the condition eventually stabilizes, patients are usually left with significant disabilities. There is no treatment.
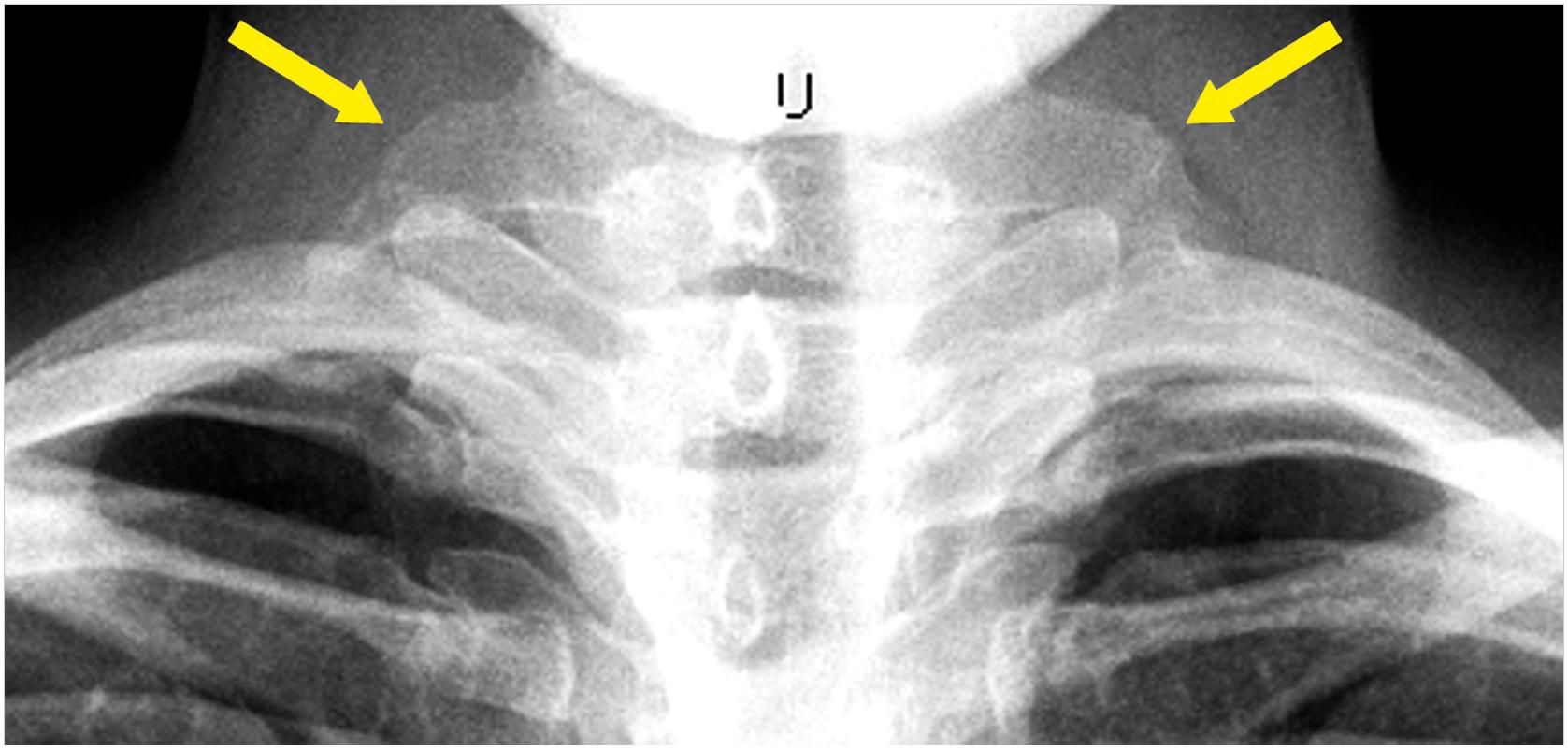
Neurogenic thoracic outlet syndrome occurs when an anomalous fibrous band between the first thoracic rib and a cervical rib or elongated transverse process on the seventh vertebral body exerts pressure on the first thoracic nerve root or the lower trunk of the brachial plexus. This leads to wasting and atrophy of the hand muscles, particularly of the thenar eminence, and intermittent pain and paresthesias of the inner arm and medial hand, including the fourth and fifth digits. Electrodiagnostic studies confirm the diagnosis. A chest x-ray may show the cervical rib or an elongated transverse process ( Fig. 60-1 ); the fibrous band shows up as a radiolucency. MRI may be helpful in showing and localizing plexus involvement ( Fig. 60-2 ). Treatment is surgical.

The distribution of findings may suggest either a focal, multifocal, or generalized/symmetric pattern of nerve involvement. For the multifocal and generalized neuropathies in particular, identifying the relative involvement of motor and sensory fibers ( Tables 60-3 to 60-5 ) narrows the differential diagnosis. Sensory neuropathies may be further subdivided according to whether predominantly large- or small-diameter fibers are affected ( Tables 60-4 and 60-5 ). Knowing whether the pathogenesis is predominantly axonal or demyelinating ( Tables 60-6 and 60-7 ) also refines the diagnostic search. Generally, patients with axonal neuropathies present with predominantly sensory signs and symptoms, whereas patients with demyelinating neuropathies have more significant weakness. Given the exceptions to this rule, however, NCSs must be performed to distinguish between these two possibilities. Finally, the time course of symptom onset has important implications for pathogenesis ( Table 60-8 ). Discussion here focuses on those peripheral neuropathies associated with systemic diseases.
| Inflammatory and Infectious |
| Chronic inflammatory demyelinating polyradiculoneuropathy |
| Guillain–Barré syndrome |
| Infectious mononucleosis |
| Multifocal motor neuropathy |
| Metabolic |
| Diabetic lumbosacral radiculoplexopathy (diabetic amyotrophy) |
| Porphyria |
| Neoplastic |
| Lymphoma |
| Toxic |
| Dapsone |
| Lead |
| Mercury |
| Nitrofurantoin |
| Organophosphates |
| Connective tissue disorder (especially Sjögren syndrome, systemic lupus erythematosus) |
| Diabetes mellitus |
| Monoclonal gammopathy |
| Nutritional |
| Vitamin B 12 deficiency |
| Vitamin E deficiency |
| Pyridoxine deficiency |
| Paraneoplastic (associated with anti-Hu antibody) |
| Renal failure |
| Toxic |
| Cisplatin |
| Pyridoxine |
| Nitrous oxide |
| Glutethimide |
| Metabolic |
| Amyloidosis |
| Early diabetic polyneuropathy |
| Fabry disease |
| Renal failure |
| Tangier disease |
| Infective |
| Human immunodeficiency virus infection |
| Leprosy |
| Toxic |
| Chloramphenicol |
| Ethanol |
| Metronidazole |
| Other |
| Sensory neuritis of Wartenberg |
| Sensory perineuritis |
| Drugs |
| Amiodarone |
| Chemotherapeutic agents [Adriamycin (doxorubicin), Taxol (paclitaxel), vincristine] |
| Dapsone |
| Disulfiram |
| Hydralazine |
| Isoniazid |
| Metronidazole |
| Nitrofurantoin |
| Phenytoin |
| Tricyclic antidepressants |
| Endocrine |
| Acromegaly |
| Diabetes mellitus |
| Hypothyroidism |
| Infectious |
| Hepatitis B |
| HIV infection |
| Lyme disease |
| Mononucleosis |
| Tick paralysis |
| Metabolic |
| Critical illness |
| Hyperglycemia |
| Hypoglycemia |
| Hypophosphatemia |
| Renal failure |
| Neoplastic and Paraneoplastic |
| Amyloidosis |
| Leukemia |
| Lymphoma |
| Monoclonal gammopathy |
| Small cell lung cancer |
| Nutritional |
| Deficiency of vitamin B 1 , B 6 , B 12 , or E or of copper |
| Vitamin B 6 intoxication |
| Toxins |
| Acrylamide |
| Arsenic |
| Carbon disulfide |
| Ethanol |
| Industrial toxins |
| Lead |
| Mercury |
| Methylbutyl ketone |
| Thallium |
| Triorthocresylphosphate |
| Trauma |
| Cold |
| Mechanical |
| Radiation |
| Acute |
| Acute arsenic poisoning |
| Diphtheria |
| Guillain–Barré syndrome |
| Subacute and Chronic |
| Chronic inflammatory demyelinating polyradiculoneuropathy |
| Monoclonal gammopathy |
| Monoclonal gammopathy of undetermined significance |
| Multiple myeloma |
| Cryoglobulinemia |
| Waldenström macroglobulinemia |
| POEMS syndrome (osteosclerotic myeloma) |
| Lymphoma |
| Lymphoproliferative Disorder |
| After allogenic stem-cell transplant for malignancy |
| Toxins |
| Checkpoint inhibitors |
| n -Hexane |
| Tacrolimus |
| Acute Onset (Hours to Days) |
| Compression |
| Diphtheria |
| Guillain–Barré syndrome |
| HIV infection |
| Ischemia |
| Lyme disease |
| Porphyria |
| Tick paralysis |
| Toxic (e.g., arsenic) |
| West Nile virus infection |
| Subacute Onset (Weeks to Months) |
| Infectious |
| Inflammatory and immune disorders |
| Metabolic |
| Nutritional |
| Paraneoplastic |
| Toxic |
| Chronic (Years) |
| Amyloidosis |
| Chronic inflammatory demyelinating polyradiculoneuropathy |
| Diabetes mellitus |
| Hereditary neuropathy |
| Monoclonal gammopathy |
| Monophasic |
| Guillain–Barré syndrome |
| Herpes zoster |
| Inflammatory ganglionopathy |
| Single toxic exposure |
| Relapsing |
| Hereditary neuropathy with liability to pressure palsy |
| Inflammatory and immune disorders (chronic inflammatory demyelinating polyradiculoneuropathy, monoclonal gammopathy, connective tissue disorders) |
| Porphyria |
| Refsum disease |
| Repeated toxic exposure |
A focal neuropathy may occur wherever ischemia, trauma, compression, injection, infection, or tumor infiltration affects the nerve. Focal ischemic neuropathies are uncommon following brief acute arterial occlusion. An exception to this rule is acute ischemic fibular (peroneal) neuropathy after thrombosis or embolism of the superficial femoral or popliteal arteries. The patient presents with a cool, pulseless distal lower extremity, sudden pain in the calf or foot, and footdrop. The nerve’s susceptibility is related to the common occurrence of a single arterial feeder at the lateral aspect of the knee. Once circulation is restored, recovery may take weeks but is often good. Arterial insufficiency may lead to chronic ischemic neuropathies. Brachial artery to cephalic vein shunts placed for hemodialysis have been associated with median, ulnar, and radial neuropathies. A vascular steal syndrome seems to be a major mechanism of nerve injury, but direct compression of nerves and distal limb edema may also play a role.
Benign tumors of nerves (schwannomas and meningiomas) usually present as sporadic, solitary tumors with or without neurologic signs or symptoms. In a patient with multiple such lesions, however, neurofibromatosis should be suspected. An enlarging lesion or the development or progression of neurologic signs should raise suspicion of malignant transformation.
The common entrapment neuropathies—median neuropathy at the wrist, ulnar neuropathy at the elbow, and fibular (peroneal) neuropathy at the fibular head—share anatomic factors that increase the susceptibility of the nerve to injury; these factors include superficial nerve location, adjacent bony structures, and enclosure by nonelastic connective tissues. External compression of nerves generally causes focal demyelination before significant axonal loss.
Various medical conditions contribute to carpal tunnel syndrome (CTS; median nerve entrapment at the wrist), the most common compressive neuropathy. Diabetes mellitus is a major risk factor. The pathogenesis of CTS in this context may relate to chronic endoneurial hypoxia and changes in the connective tissues of the nerve sheath or transverse carpal ligament. Hypothyroidism and acromegaly are also associated with CTS. In acromegaly, edema of synovial tissues may cause nerve compression. In pregnancy ( Chapter 31 ), edema and weight gain contribute to increased pressure in the carpal tunnel. Rheumatoid arthritis is the most important inflammatory condition associated with CTS. Rheumatoid nodules, wrist deformity, and tenosynovitis are all contributory factors. When CTS accompanies a distal symmetric polyneuropathy in a nondiabetic patient, amyloidosis should be considered. If such patients undergo carpal tunnel surgery, fat and ligament tissue should be sent to pathology for analysis for possible amyloid deposition. Other risk factors for CTS include female sex, ganglion cysts, lipomas, nonspecific tenosynovitis, gout, sarcoidosis, multiple myeloma, aromatase inhibitors, and hereditary neuropathy with liability to pressure palsies. Repetitive hand motions in certain occupations may also be contributory. Conservative management of CTS includes the nocturnal use of wrist splints to prevent wrist flexion or extension (which reduces pressure within the carpal tunnel) or oral or injected corticosteroids. For severe neuropathies or for those in whom conservative measures have failed, surgical release of the carpal tunnel is effective.
The evaluation and management of the other common entrapment neuropathies are discussed in standard neurologic texts.
Most multifocal neuropathies are immune mediated or infectious ( Table 60-9 ). The immune-mediated forms may be idiopathic, triggered by an infection or toxin/medication, or associated with diabetes mellitus. The most severe presentation is the acute and catastrophic appearance of multiple mononeuropathies (mononeuritis multiplex) caused by systemic vasculitis.
| Infection |
| Diffuse infiltrative lymphocytosis syndrome |
| Herpes zoster |
| Human immunodeficiency virus infection |
| Leprosy |
| Lyme disease |
| Syphilis |
| Tuberculosis |
| Ischemia |
| Vasculitic neuropathy |
| Systemic necrotizing vasculitis |
| Vasculitis associated with connective tissue diseases (rheumatoid arthritis, Sjögren syndrome, systemic lupus erythematosus) |
| Vasculitis associated with infections (hepatitis B and C, HIV) |
| Medication-induced vasculitis |
| Nonsystemic vasculitic neuropathy |
| Diabetes mellitus (diabetic lumbosacral radiculoplexus neuropathy, diabetic mononeuropathies) |
| Idiopathic Immune-Mediated Neuropathy |
| Idiopathic brachial plexopathy |
| Graft-versus-host disease |
| Multifocal acquired demyelinating sensory and motor neuropathy (Lewis–Sumner syndrome) |
| Multifocal motor neuropathy |
| Sarcoidosis |
| Sensory neuritis of Wartenberg |
| Sensory perineuritis |
| Multiple Compressions and Entrapments |
| Amyloidosis |
| Neurolymphomatosis |
| Rheumatologic conditions |
| Trauma |
| Tumors |
| Genetic Conditions |
| Hereditary neuropathy with liability to pressure palsy |
| Porphyria |
Vasculitic neuropathy is an ischemic neuropathy caused by obliteration of the nerve’s nutrient blood vessels by inflammatory infiltrates. It usually presents as a subacutely evolving, asymmetric, painful sensory or sensorimotor neuropathy. Often, the deficits are in the distribution of multiple individual nerves (mononeuropathy multiplex). Nerves in the lower extremities are often affected first, but any nerve may be involved. Over time in untreated patients, as additional nerves become injured, motor and sensory deficits may become confluent, thereby mimicking a polyneuropathy. Sometimes, as in the case of cryoglobulinemic vasculitic neuropathy, the initial presentation of a vasculitic neuropathy is symmetric.
Neuropathy may occur with primary vasculitis, in which the underlying cause is not known, or secondary vasculitis, in which the causative factor is identified. The primary systemic vasculitides are classified according to size of the damaged blood vessels, organs involved, and the suspected immunopathologic mechanisms at play. Polyarteritis nodosa, microscopic polyangiitis, granulomatosis with polyangiitis (Wegener granulomatosis), and eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome) are the primary systemic vasculitides most commonly associated with vasculitic neuropathies. The most common vasculitic neuropathy is an idiopathic form similar to polyarteritis nodosa and microscopic polyangiitis but without overt systemic involvement, called nonsystemic vasculitic neuropathy. Because these patients do not have a defined connective tissue or other systemic disease, the diagnosis is established by nerve biopsy. Most of these patients have an elevated erythrocyte sedimentation rate, and a minority are anemic with peripheral leukocytosis and thrombocytosis. Secondary vasculitis may be associated with connective tissue diseases, infections, neoplasms, medications, or toxins.
Given the broad differential diagnosis of vasculitic neuropathy, the laboratory evaluation is extensive and often includes a complete blood count and erythrocyte sedimentation rate; examination for antinuclear antibodies, rheumatoid factor, antineutrophil cytoplasmic antibodies, complement levels, and hepatitis B and C serologies; urinalysis with microscopic analysis; and renal and hepatic function tests. The work-up may also include an HIV antibody test, chest x-ray, and Lyme antibody studies. An electrodiagnostic study is essential to document the multifocal nature of the axon loss. A nerve biopsy is often necessary for diagnosis. For the systemic vasculitides, the diagnostic yield is increased if biopsy is performed on both the nerve and muscle.
The systemic vasculitides are often fatal if untreated, so aggressive immunosuppression with combined corticosteroids and cyclophosphamide is usually indicated. When vasculitis is caused by drugs, removal of the offending agent often leads to benefit. For vasculitis associated with chronic viral infections, treatment often includes antiviral therapy or removal of viral antigens by plasmapheresis.
Approximately one-third of cases of polyarteritis nodosa are associated with hepatitis B infection. More than 80 percent of patients with hepatitis B–associated polyarteritis nodosa have a neuropathy. Although the clinical features may be indistinguishable from classic polyarteritis nodosa, the disease manifestations of hepatitis B–associated vasculitis may be more severe. Immune complex deposition is thought to be the main immunopathologic mechanism.
Treatment of hepatitis B–related vasculitic neuropathy is specialized. Although immunosuppressive therapies lead to increased viral replication, two retrospective studies suggest that a short course of corticosteroids is beneficial. Following steroid therapy, either tenofovir or entecavir may be used. Plasma exchanges are usually given concurrently over a 10-week period to clear the immune complexes. Relapses are uncommon.
A minority of patients with hepatitis C virus (HCV) infection develop a peripheral neuropathy, sometimes associated with cryoglobulinemia. As cryoglobulinemia can cause a vasculitic neuropathy with more severe neurologic deficits, the following discussion focuses on it.
HCV is the most common cause of essential mixed cryoglobulinemia, which occurs in about one-third of patients with HCV; a cryoglobulinemic neuropathy only occurs in 2 to 3 percent of patients. Other manifestations of cryoglobulinemia include edema, palpable purpura, and membranoproliferative glomerulonephritis. The cryoglobulinemia results from an oligoclonal expansion of B-lymphocytes. Most cryoglobulinemic neuropathies are distal, axonal, and symmetric with predominantly sensory deficits. Mononeuropathies, either single or multiple, may also occur. Rarely, patients with cryoglobulinemia may develop demyelinating polyneuropathies associated with IgM binding to myelin.
Patients with HCV-associated cryoglobulinemic neuropathy should be treated with direct-acting antiviral therapy. For refractory cases, immunosuppression with monoclonal anti-CD20 antibodies (rituximab) with or without corticosteroids may be necessary.
Any organism can produce a vasculitis if it elicits either circulating or in situ immune complexes. CMV and herpes zoster are the only two infections known to infect endothelial cells of peripheral nerve blood vessels.
HIV infection ( Chapter 43 ) may rarely cause a systemic vasculitis. It usually occurs in the early symptomatic stage of the disease. Multiple patterns of nerve involvement have been described, including mononeuropathy, mononeuritis multiplex, cranial neuropathies, distal symmetric polyneuropathy, and asymmetric polyneuropathy. The possibility of CMV vasculitis must be excluded in this patient population. In CMV-negative cases, nerve biopsy samples show a necrotizing vasculitis that may involve the endoneurial vessels in addition to the epineurial vessels. Other causes of multifocal neuropathies in HIV patients include neurolymphomatosis and diffuse infiltrative lymphocytosis syndrome.
Immune-mediated multifocal neuropathies exist in which the target of the immunologic attack is the myelin or axon rather than the blood vessels. These entities include multifocal motor neuropathy, Lewis–Sumner syndrome (or multifocal acquired demyelinating sensory and motor neuropathy), sensory perineuritis, and migratory sensory neuropathy of Wartenberg. In some cases, there is overlap between these neuropathies and GBS and chronic inflammatory demyelinating polyneuropathy (CIDP). Because GBS and CIDP are usually associated with generalized weakness, however, they are discussed separately in a later section.
Multifocal motor neuropathy is important to recognize because it can superficially mimic motor neuron disease, and attention here is focused on this disorder. Patients typically present with painless wasting, weakness, and sometimes fasciculations of the distal upper-extremity muscle groups, although any muscle group may be affected, even the tongue. Careful examination reveals that weakness occurs in a peripheral nerve rather than segmental pattern. Upper motor neuron signs are not present. Patients may complain of mild sensory symptoms such as numbness or paresthesia, but the sensory examination is typically normal. Reflexes tend to be depressed only in regions of weakness. NCSs usually reveal conduction block in motor nerves along with normal sensory nerve conduction responses. Half of patients have elevated titers to GM1 ganglioside.
IVIg is the most effective therapy for multifocal motor neuropathy, with approximately 80 percent of patients responding to it. Its efficacy has been confirmed by multiple randomized, placebo-controlled trials. Other agents that may improve or stabilize the disease include subcutaneous immunoglobulin, cyclophosphamide, azathioprine, rituximab, and interferon-beta. Mycophenolate mofetil did not have an IVIg-sparing effect in a randomized, controlled trial. Although a few patients have been reported to respond to prednisone, it is usually ineffective or may cause an exacerbation of weakness. Plasmapheresis is usually not effective.
Neurosarcoidosis is discussed in Chapter 49 , to which the reader is referred.
Lyme disease and leprosy are important causes of multifocal neuropathy and are discussed separately in Chapter 39, Chapter 41 .
The medical disorders discussed in this section cause generalized and symmetric neuropathies. In axonal neuropathies, the sensory and motor deficits are usually length dependent such that the deficits are most severe in the feet. With long-term disease, a classic stocking-glove neuropathy occurs, with or without autonomic involvement. In demyelinating polyneuropathies, however, the weakness may involve proximal and distal muscle groups more equally.
As discussed in Chapter 19 , diabetes mellitus may be associated with both generalized and focal neuropathies. The focal neuropathies include lumbosacral radiculoplexus neuropathy (diabetic amyotrophy; proximal diabetic neuropathy), thoracolumbar neuropathy, entrapment neuropathies, and cranial neuropathies. The generalized neuropathies include distal symmetric sensory or sensorimotor polyneuropathy, acute painful neuropathy, autonomic neuropathy, and acute motor neuropathy.
Approximately 50 percent of diabetics develop a distal symmetric sensorimotor polyneuropathy. Risk factors for polyneuropathy include degree of hyperglycemia, duration of diabetes, age, hypertension, hypertriglyceridemia, and smoking. The association between prediabetes and polyneuropathy is a subject of active debate. A number of investigators have found an increased prevalence of impaired glucose tolerance in patients with idiopathic neuropathy. However, a careful case-control study of patients with idiopathic neuropathy did not show a significant association between prediabetes and neuropathy.
Early symptoms include distal numbness, burning dysesthesias, and allodynia in the feet or toes. Although discomfort is present throughout the day, it often worsens at night or with rest. Cramps are common in the calves and foot muscles. Treatment consists of tight glycemic control, which helps to prevent and slow the progression of the polyneuropathy. Large-scale controlled trials of aldose reductase inhibitors and nerve growth factor in the treatment of diabetic neuropathy have yielded disappointing results. Controlled trials of intravenous and oral preparations of the antioxidant α-lipoic acid have demonstrated its benefit on neuropathy signs and pain.
Hypothyroidism is a common cause of median neuropathy at the wrist (CTS). Myxedematous tissue beneath the flexor retinaculum is thought to cause median nerve compression. Hypothyroidism may also cause a polyneuropathy that presents with distal dysesthesias and stocking-and-glove sensory loss. Reflexes may be diminished with a delayed relaxation phase. Electrodiagnostic and pathologic studies have shown mixed axonal and demyelinating features. Considerable improvement may occur in both CTS and hypothyroid polyneuropathy following replacement therapy.
Acromegaly may cause entrapment neuropathies due to connective tissue hyperplasia and bony overgrowth. A sensorimotor polyneuropathy may also occur associated with hypertrophic, sometimes palpable, nerves.
As discussed in Chapter 43 , HIV infection is associated with both acute and chronic, multifocal or generalized polyneuropathies. These include mononeuritis multiplex from vasculitic neuropathy, GBS, CIDP, and distal sensory polyneuropathy. Of all these neuropathies, distal sensory polyneuropathy is by far the most common, occurring in at least 50 percent of patients with advanced HIV infection. In the era before combination antiretroviral therapy, reduced CD4 + lymphocyte cell counts and increased HIV viral loads increased the risk and severity of HIV polyneuropathy. Dideoxynucleoside antiretrovirals also increase the risk of neuropathy, possibly because of toxicity to mitochondria. A polyneuropathy (usually symmetric) may occur as part of the diffuse infiltrative lymphomatosis syndrome.
Patients typically present with burning dysesthesia in feet and ankles, often with prominent allodynia. On examination, small-fiber sensory modalities are affected predominantly. Weakness related to the neuropathy is uncommon, even in advanced cases. There is no specific treatment, although a number of symptomatic treatments for neuropathic pain, including gabapentin, amitriptyline, tramadol, and lamotrigine, are effective.
HCV infection and leprosy may cause generalized and symmetric peripheral nerve involvement, as is discussed earlier in this chapter and elsewhere in this volume.
Once used interchangeably with the label acute inflammatory demyelinating polyneuropathy , GBS now encompasses any acute, idiopathic inflammatory polyneuropathy producing progressive muscle weakness and areflexia, regardless of whether the underlying neuropathy is demyelinating or axonal. In many cases, a respiratory or gastrointestinal illness precedes the onset of neurologic symptoms by 1 to 3 weeks. Often paresthesias in the distal limbs herald the onset of the neuropathy. Pain similar to sciatica, myalgia, or a cramp may also occur. Rapidly progressive, symmetric weakness soon follows. Typically the weakness starts in the legs, but it may begin in the arms or face. Symptoms may progress acutely over just a few days or subacutely over as long as 4 weeks. The degree of weakness at the nadir of the progressive phase is highly variable, from mild weakness to quadriplegia with respiratory failure. Maximum deficits occur within 1 month, followed by a plateau lasting for days to weeks and rarely months. Gradual improvement occurs after the plateau phase. Prognosis is good, with a 5 percent mortality rate. Permanent disabilities remain in 5 to 10 percent of patients, mild deficits in 65 to 75 percent, and no deficit in 15 percent. The annual incidence is 1 to 2 cases per 100,000 population.
The initial assessment of GBS patients should include measurements of respiratory capacity and inspiratory force. Patients with a vital capacity of less than 20 mL/kg or a maximum inspiratory pressure less than 30 cmH 2 O are likely to require mechanical ventilation. These measurements are much more sensitive than arterial blood gas analysis for predicting incipient neuromuscular respiratory failure. Admission to the intensive care unit (ICU) is warranted for any patient with rapidly progressive disease, significant bulbar or facial weakness, or autonomic dysfunction. Motor findings typically outweigh sensory deficits. One-third of patients may develop facial diplegia. Stretch reflexes are hypoactive or absent.
Blood tests and a lumbar puncture should be undertaken to evaluate for other causes of acute polyneuropathy or polyradiculopathy. In 50 percent of patients, an initial CSF sample will reveal an elevated protein concentration; with subsequent analysis, 90 percent of samples show increased protein, with values ranging from 55 to 250 mg/dL. The CSF is usually acellular with normal pressure. If more than 10 white cells/mm 3 are present, alternative diagnoses should be considered. NCSs commonly show evidence of a polyneuropathy, usually demyelinating, but are sometimes normal when the patient first presents.
In Western societies, GBS is usually a demyelinating polyradiculoneuropathy (acute inflammatory demyelinating polyradiculoneuropathy; AIDP). A number of infections may trigger GBS, including CMV, Epstein–Barr virus, herpesvirus, Campylobacter jejuni , Mycoplasma pneumoniae , and HIV infection. Rabies and swine flu vaccinations, recent surgery, and pregnancy have also been implicated as triggers for GBS. Both humoral immune responses and T-cell activation are thought to play roles in the pathogenesis. Pathologically, there is the early appearance of lymphocytes surrounding nerve vessels. This is followed by demyelination. Secondary “bystander” axonal degeneration may also occur.
In northern China, the most common GBS subtype is an acute motor axonal neuropathy (AMAN) associated with C. jejuni infection. These patients often have antibodies to gangliosides, including GM1, GD1a, and GD1b. The strains of C. jejuni associated with AMAN have GM1-like epitopes in their lipopolysaccharide membranes that contain a Gal(b1–3)GalNac moiety. Terminal motor axon branches and the internode axonolemma also contain a high concentration of this moiety. Because of molecular mimicry between these bacterial and axon antigens, those portions of the motor axons appear to be the initial targets in the autoimmune attack.
Both AIDP and the less frequent AMAN subtype have been associated with recent Zika virus infection. The viral syndrome precedes the onset of GBS symptoms by a median of 6 days. Treatment is the same as for other presentations of GBS.
There are several other variants of GBS. The most common, the Miller Fisher syndrome, accounts for about 5 percent of all cases of GBS. Patients develop the triad of ophthalmoplegia, ataxia, and areflexia, with varying degrees of limb weakness. Almost all cases of Miller Fisher syndrome are associated with IgG antibodies to GQ1b. Other variants include pharyngeal-cervical-brachial weakness; paraparesis; bilateral facial paresis with distal paresthesias; pure ataxia; acute pandysautonomia; and acute motor–sensory axonal neuropathy. The AMAN variant is usually associated with IgG anti-GM1 antibodies. All variants have in common absent or diminished stretch reflexes, elevated CSF protein concentrations, and electrodiagnostic abnormalities.
For severe cases, treatment includes support in the ICU and immune-modulatory therapy. Plasmapheresis or IVIg is effective in improving short- and long-term neurologic function. The costs of plasmapheresis and IVIg are similar, and the relapse rate for IVIg is no different from that for plasmapheresis. Compared with plasmapheresis, IVIg is associated with fewer complications (e.g., hemodynamic fluctuations), is easier to administer, and is usually available in community hospitals where plasmapheresis may not be accessible. A combination of plasmapheresis followed immediately by IVIg does not lead to significantly better outcomes.
Corticosteroids are not beneficial.
CIDP is a chronic neuropathy characterized by symmetric weakness, sensory loss, and depressed stretch reflexes. Weakness usually affects both proximal and distal muscle groups. The cranial nerves are rarely involved, but cranial neuropathies may be a presenting feature. A small percentage of patients have papilledema. The weakness must progresses beyond 2 months in order to meet an arbitrary criterion for the diagnosis of CIDP. The clinical course may be relapsing, progressive, or stepwise. There are a number of clinical variants of CIDP manifesting with either pure motor or sensory involvement or with evidence of only distal demyelination. CIDP may occur with certain medical disorders, including monoclonal gammopathies, inflammatory bowel disease, thyroid disease, HIV infection, diabetes mellitus, Charcot–Marie–Tooth neuropathies, and CNS demyelination. Approximately 10 percent of CIDP patients have antibodies directed against proteins expressed at the nodes of Ranvier. Patients with these antibodies do not have segmental demyelination of the nerve fibers. Instead disruption of the nodal architecture blocks conduction of signals along the affected nerve fibers.
The electrodiagnostic and pathologic features are similar to those of GBS. Lumbar puncture typically reveals an acellular CSF with an elevated protein level, but other laboratory tests are unremarkable. NCSs confirm slowed nerve conduction velocities or the presence of conduction block caused by demyelination. Nerve biopsy is occasionally performed, and the findings include endoneurial perivascular inflammation with demyelination, remyelination (onion bulb formations), and secondary axonal degeneration.
Randomized, controlled trials have demonstrated the benefit of corticosteroids, plasmapheresis, subcutaneous Ig, and IVIg. A crossover study demonstrated that plasmapheresis and IVIg are about equally effective. Azathioprine, cyclosporine, mycophenolate, and cyclophosphamide are sometimes reported to be beneficial but have not been tested in controlled clinical trials. Overall, most patients respond to treatment, but relapses are common. Most patients ultimately achieve a remission. Aggressive and early treatment is warranted because unchecked disease may eventually lead to axon loss and muscle atrophy for which there is no specific treatment.
A monoclonal gammopathy of undetermined significance (MGUS) may present as a symmetric sensorimotor polyneuropathy with variable proportions of axonal or myelin injury. The prevalence of MGUS is 1 to 3 percent in people older than 50 years. Only a minority of those with MGUS ever develop a clinically significant neuropathy, the precise number varying in different series and depending on which heavy chain is involved. Compared with neuropathy patients having IgA and IgG MGUS, patients with IgM MGUS have more sensory ataxia and more evidence of demyelination on electrodiagnostic studies. Specific antibodies can sometimes be found to myelin-specific proteins. The CSF is acellular but the protein concentration is often elevated.
Generally, neuropathies associated with MGUS respond less well to immunosuppressive or immunomodulatory therapy than idiopathic CIDP. IgG and IgA MGUS neuropathies respond better than IgM MGUS neuropathies to plasmapheresis. Improvement has also been documented with rituximab, fludarabine, and alkylating agents. Some patients have responded to IFN-α and IVIg. Long-term studies to determine the relationship between specific immunologic markers and disease recurrence will help to develop targeted therapies.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here