Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter is an overview of the examination of higher cortical function as it relates to cortical anatomy and associated functions. Detailed anatomic drawings of the cerebral cortex are provided for one's review while reading this chapter. By the end of the chapter, the reader should gain a basic understanding of cognitive function, anatomical localization, and the neurocognitive examination.
A 78-year-old, right-handed woman presents with a fixed delusional syndrome with increasing paranoia developing over the previous year. There is no past history of psychiatric illness, trauma, surgery, or hospitalizations. There is no history of alcohol or substance abuse. Her behavior becomes increasingly volatile, at times extremely anxious, tearful, or aggressive. She believes there is a female stalker following her everywhere. She would be with her in the bathroom, closet, outside the house, etc. She is always behind her and sometimes would touch the back of her head or her left ear. She would interrupt her in the kitchen, reaching in to grab things without warning. Whenever the patient would look in the mirror, the stalker would hide. The patient is not certain if this intruder is human or not and sometimes thinks the intruder could be her, the patient. She is treated by several psychiatrists, including an inpatient psychiatric hospital stay, with no response to antipsychotic therapy.
On examination she is awake, alert, oriented to person, place, but not to the year or the month. She is attentive to conversation and demonstrates normal comprehension. She speaks fluently, although speech is notable for occasional word finding difficulty. Short-term memory is mildly impaired, recalling only 1 out of 3 words in 5 minutes. The rest of the neurologic examination is notable for visual and tactile extinction to double simultaneous stimulation on the left side. She has finger agnosia on the right. She has partial agnosia of her right hand, sometimes identifying it as someone else and sometimes as her own hand. In fact, she cannot identify her left hand as her own when holding both hands in front of her. The rest of the neurologic examination demonstrates normal cranial nerve, motor, and primary sensory function bilaterally. There are no signs of parkinsonism. Her brain magnetic resonance imaging (MRI) is notable for bi-parietal and mesial temporal atrophy, worse on the right. Blood work is normal. Metabolic brain positron emission tomography (PET) scan shows marked hypometabolism in the right parietal lobe, as well as milder hypometabolism in the left parietal lobe. Comment: This case demonstrates an atypical presentation of dementia affecting posterior cortical function and presenting with pronounced behavior changes and less obvious cognitive decline. However, a detailed cognitive examination was crucial in delineating the basis for her delusion. A combination of sensory extinction on the left and limb misidentification on the right led to her delusional state. She did not recognize her right hand when rubbing her head or touching her ear and misidentified it as someone else's hand. Similarly, she visually extinguished her left hand when both hands were in front of her working in the kitchen. She again misidentified the right hand as someone else's hand. Her language abilities were relatively normal, thus she was able to describe her experience. Hypothetically, her dominant hemisphere was verbalizing severely distorted sensory information coming from the nondominant hemisphere.
Cognition is a complex neurologic function involving multiple neural networks distributed throughout the brain. The neurocognitive examination strives to determine deficits in specific cognitive domains and to localize deficits to corresponding neuroanatomic regions. As in all aspects of neurology, localization of deficits is imperative in making the correct diagnosis.
Behavior often reveals underlying cognitive impairment. The patient's mood, affect, level of cooperation, and distractibility during the interview should be noted. Patients with cognitive deficits commonly develop symptoms of anxiety, depression, even suspiciousness. The emotional consequences of cognitive dysfunction are often mistaken as the primary cause of cognitive symptoms when, in fact, the behavioral changes reflect cognitive impairment. Conversely, there may be limited subjective concern or awareness of underlying cognitive impairment. For example, the early stages of Alzheimer disease may go unnoticed in social situations and patients may not be fully aware of their memory impairment. Without some screening examination of mental status, these cases of early dementia or mild cognitive impairment go undetected until their dementia reaches more severe stages.
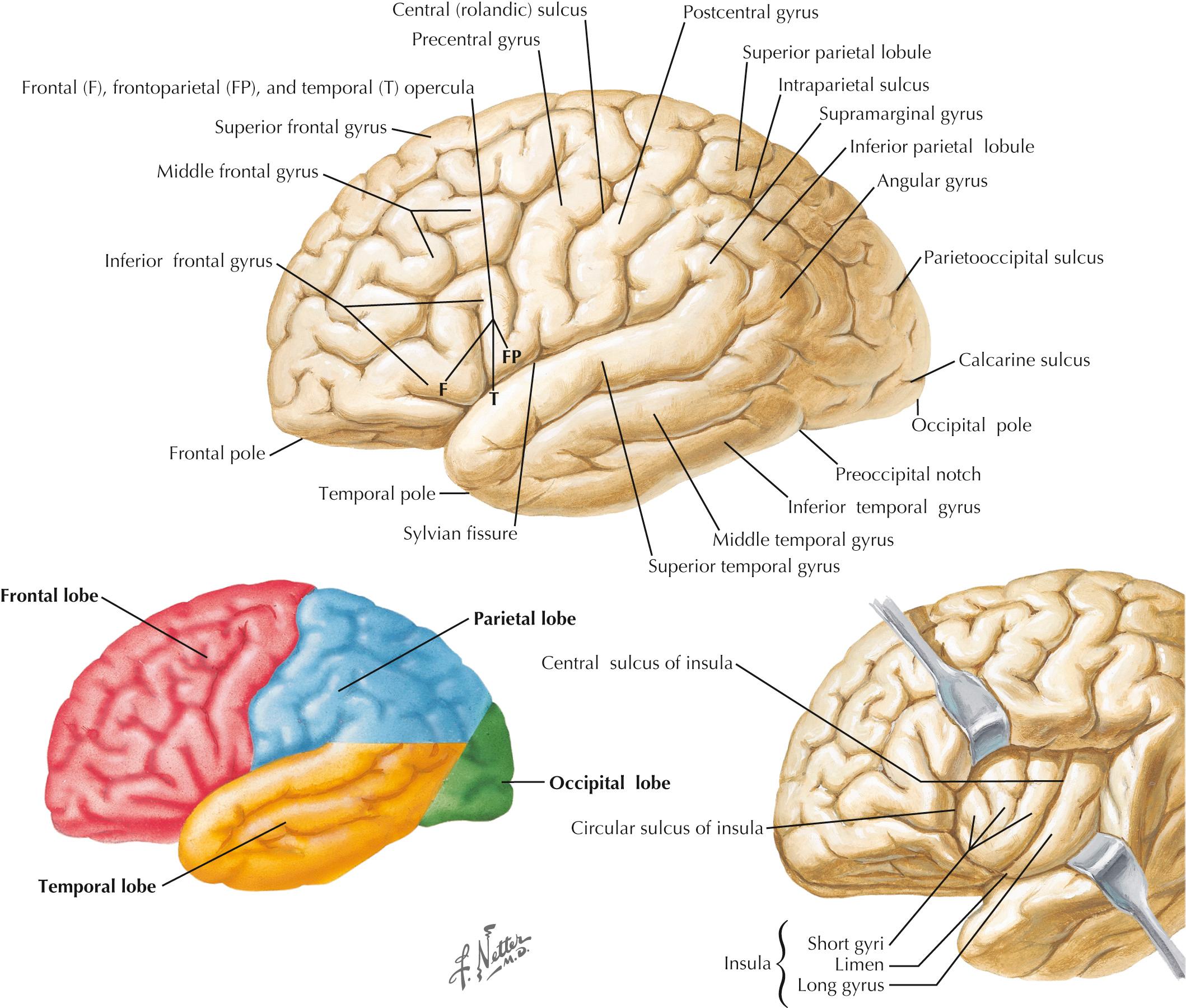
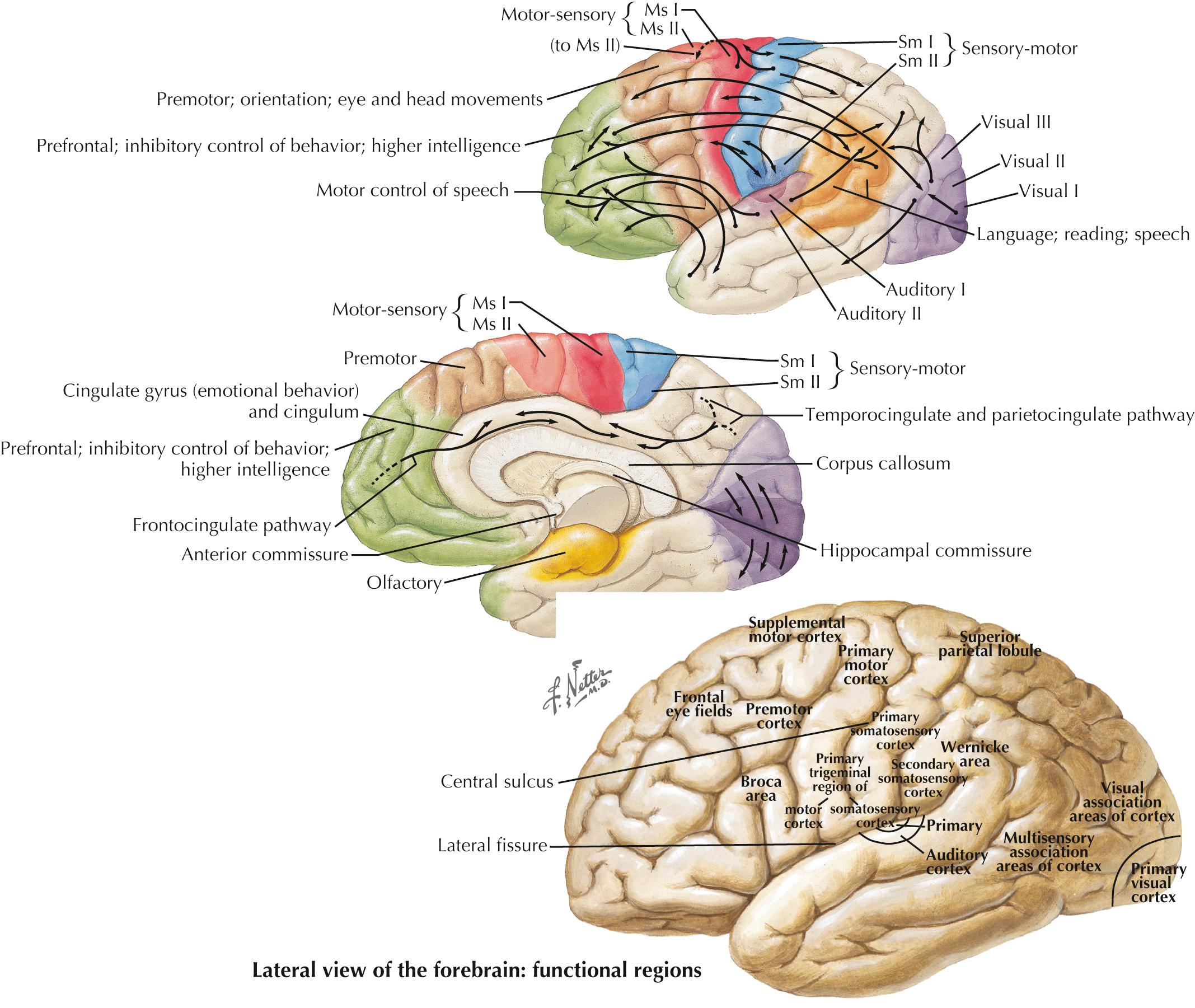
The human cerebral cortex, a network of billions of interconnections, is the most complex part of the nervous system. Anatomically, the cortex is grossly classified into four major functional areas: frontal, temporal, parietal, and occipital lobes ( Fig. 25.1 , Table 25.1 ). These anatomic regions serve different functions, are processed in parallel, and are interconnected in a complex network integrating sensory, motor, memory, and emotional information ( Fig. 25.2 , Table 25.2 ). Although these cortical areas are traditionally discussed as functionally and anatomically isolated, in reality they are components of a larger neural network processing input, output, and feedback from one another. The interconnectedness of cortical regions is critical for “higher cortical” function.
| Structure | Anatomic Significance |
|---|---|
| Lateral (Sylvian) fissure | Separates temporal lobe from frontal and parietal lobes |
| Central (Rolandic) sulcus | Separates frontal lobe from parietal lobe |
| Lobe | Notable Gyri | Notable Sulci | Notable Functions |
|---|---|---|---|
| Frontal | Superior frontal gyrus Middle frontal gyrus Inferior frontal gyrus Precentral gyrus |
Superior frontal sulcus Inferior frontal sulcus Precentral sulcus |
Motor control, expressive speech, personality, drive |
| Parietal | Postcentral gyrus Superior parietal lobule Inferior parietal lobule Supramarginal gyrus Angular gyrus |
Postcentral sulcus Intraparietal sulcus |
Sensory input and integration, receptive speech |
| Temporal | Superior temporal gyrus Middle temporal gyrus Inferior temporal gyrus |
Superior temporal sulcus Inferior temporal sulcus |
Auditory input and memory integration |
| Occipital | Transverse occipital sulcus Lunate sulcus |
Visual input and processing |
Assessment of cognitive function requires direct testing of various cognitive domains in a structured, hierarchical fashion. The major cognitive domains included in a routine mental status examination include level of consciousness, orientation, attention, language, memory, visuospatial processing, and executive function. These are operationally defined as follows.
Level of consciousness underlies all aspects of mental status and must be considered immediately. A stuporous patient may be difficult to examine fully due to waxing and waning level of consciousness; obviously it is not possible to make a full cognitive assessment in a comatose patient. Generally, patients may be described as awake and alert, drowsy or lethargic, stuporous (needs stimulation to stay awake and responsive), obtunded (needs stimulation to awaken but not responsive), or comatose (not awake, not responsive).
Attention is a complex brain function allowing the individual to focus and register specific information from external and internal environments. Impaired attention may affect the patient's performance in other cognitive tasks, such as reading, writing, or memorizing lists. Digit span testing is a good means to test attention. The examiner may ask the patient to repeat a list of five digits following the same sequence. Next, a list of three digits is provided and the patient is instructed to repeat the sequence in reverse order. This test elicits the patient's ability to give immediate focus and avoid distraction. Fewer than five digits forward or three digits backward would indicate attention problems.
Orientation allows an individual to identify when, where, and who they are at any given moment. This requires intact attention, memory, language, and recognition involving widespread cortical regions as well as high-order cognitive processing. Testing this simple modality provides an efficient means to survey general cognitive function. Disorientation to time and/or place may occur in either widespread or focal cortical dysfunction. Of note, not knowing the current year suggests greater severity of disorientation than not knowing today's date. Similarly, not knowing the town or state at present is more concerning than not knowing the floor of the building. Several orientation questions are necessary to identify mild disorientation. Disorientation for person may be seen in severe stages of dementia, although by this point cognitive function may be severely impaired in general and testing specific domains becomes very difficult.
Language function includes the patient's ability to monitor and to comprehend language-related sounds and visual symbols and to generate meaningful verbal or written responses. Most interaction with patients is language-based, and therefore it is crucial to ascertain whether language function is impaired early in the course of the examination. For example, a patient with an expressive aphasia may not be able to express three words during memory testing, express the date, or name of a place. Such a deficit would not necessarily indicate impaired short-term memory or inattention, but rather, a primary impairment of language. Impairment of language typically follows left hemispheric damage, although right hemispheric lesions may also impair language function, as discussed later in this chapter.
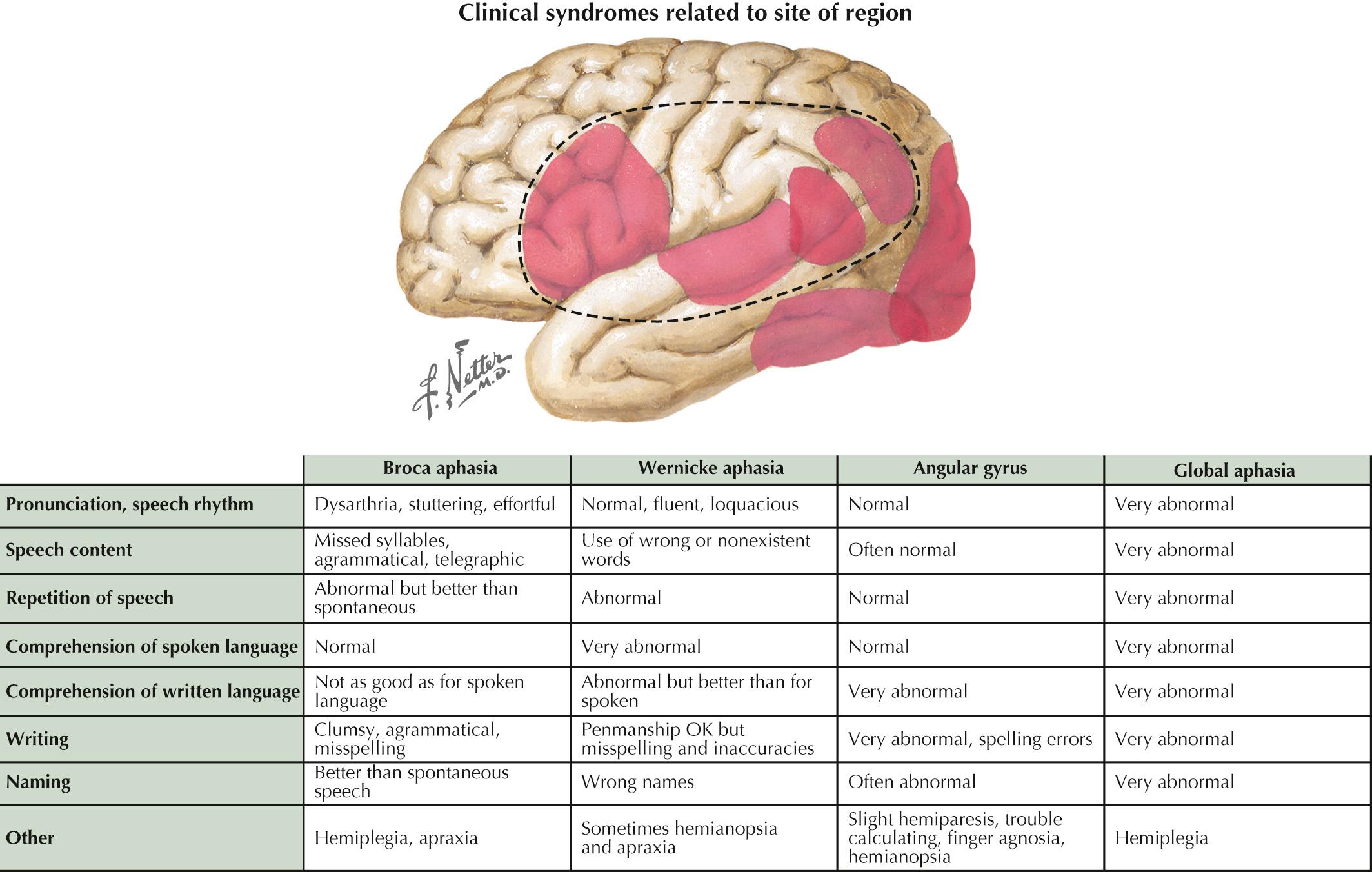
Language encompasses multiple cortical regions and is not classifiable within strict cortical anatomic borders. Impairment of language function is a common neurologic symptom presenting acutely, as in stroke, or more insidiously, as in neurodegenerative disease. The classic nomenclature of the aphasia syndromes ( Fig. 25.3 ) is largely based upon lesion analysis in cases of stroke or tumor. These syndromes postulate distinct, interconnected cortical regions responsible for the various phases of language processing from comprehension to expression. Broca syndrome is characterized by stuttering, agrammatical, effortful, and telegraphic language. This was thought to be an expressive language disorder typical of anterior frontal lesions (so-called motor aphasia). Wernicke aphasia, characterized by impairment of comprehension, is characterized by fluent expression of wrong or nonexistent words and syllables (neologisms and semantic paraphasic errors) that is sometimes referred to as a “word salad.” Receptive language disorders were thought to be related to lesions of the more posterior temporal parietal cortex. Other aphasia syndromes, such as conduction aphasia, anomic aphasia, and the transcortical aphasias, emerged to describe syndromes that did not fit neatly into the broader forms of Broca and Wernicke aphasias. These syndromes were traditionally associated with various left middle cerebral artery (MCA) territory strokes or left hemispheric tumors and were thought to arise from disconnection between distinct cortical regions. However, exceptions to the traditional classification of aphasia occur commonly. For example, it is not unusual for a posterior MCA division stroke with no injury to the inferior frontal cortex to produce a nonfluent aphasia. Moreover, the progressive aphasia syndromes often produce characteristic language disorders that do not fit any of the traditional aphasia paradigms. Indeed, even in the acute stroke setting, the classification of aphasia as expressive or receptive, motor or sensory, or nonfluent or fluent is too simplistic and often inaccurate. Very few patients present with pure aphasia syndromes.
As mentioned earlier, patients commonly present complaining of gradual onset of word-finding difficulty; this is a general symptom that is not always the result of a primary language disorder. Rather, it may be a manifestation of either inattention or a memory impairment. Therefore the assessment of language must distinguish primary language disorders from other cognitive deficits or secondary language impairment. The patient presenting with progressive primary language disturbance often does not fit neatly into the traditional neuroanatomic aphasia classifications.
Newer descriptions of language impairment elucidated through study of patients with primary progressive aphasia have emerged. There are three main types of primary progressive aphasia, namely, primary nonfluent expressive aphasia, logopenic aphasia, and semantic aphasia. Primary nonfluent expressive aphasia is characterized by progressive impairment in verbal output, the mechanics of speech, or structure of words and sentences. The patient knows what to say but not how to say it. Logopenic aphasia is a progressive loss of verbal content. Vocabulary is reduced and speech becomes emptier. As with primary nonfluent expressive aphasia, the patient knows the meaning to convey but has no words to convey the message. Semantic aphasia may be described as a loss of meaning. The patient's words do not correspond to the meaning of the message. Moreover, the patient does not comprehend the words or the messages of others, or their own message.
Language may be defined as the attempt to convey a message in verbal, spoken, or written form. This appears to occur in four interconnected stages, including speech initiation, speech content, speech structure, and motor programming of speech. These stages correlate with specific anatomical regions ( Fig. 25.4 ).
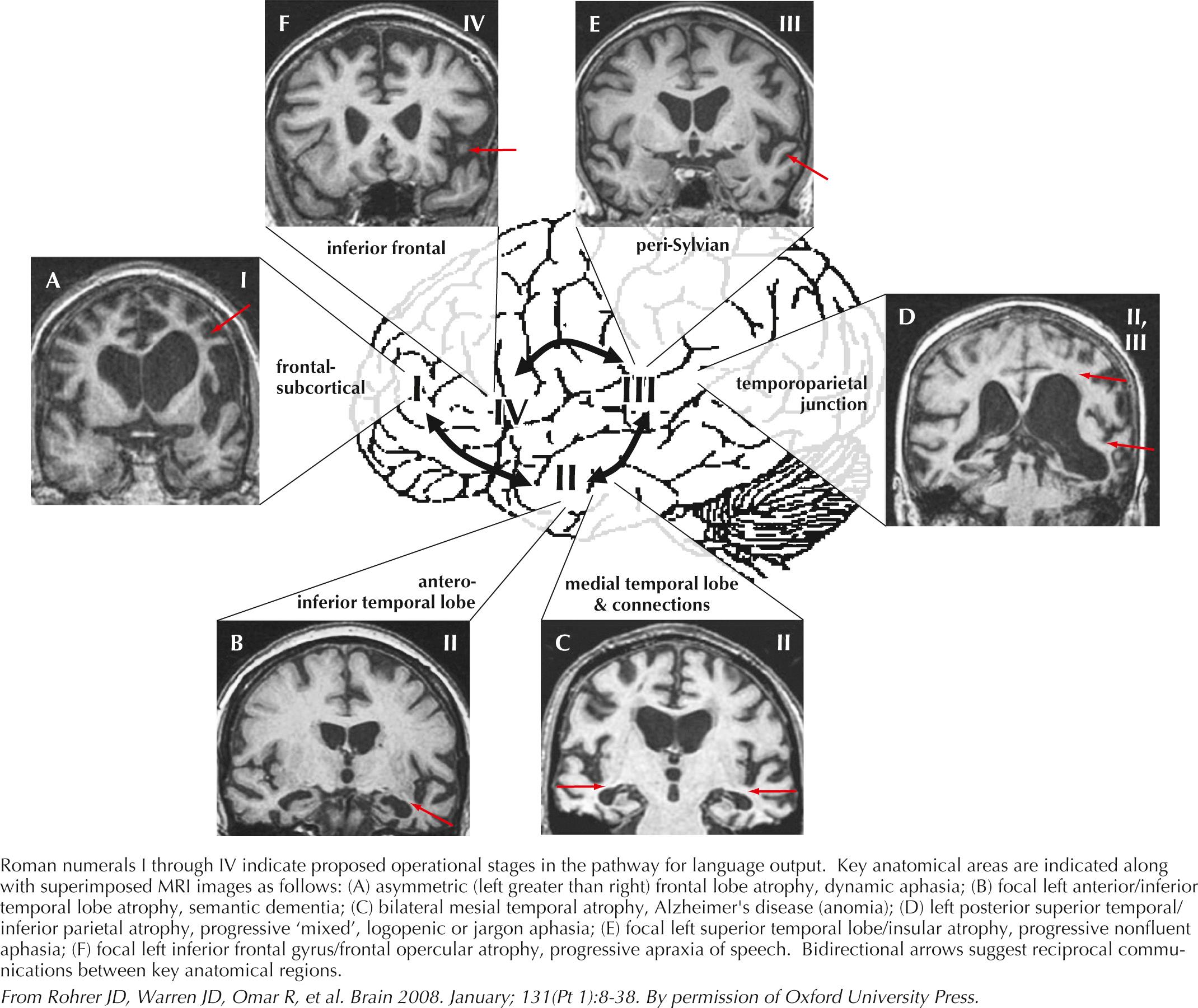
Initiation of speech involves the ability to generate and plan a spoken message. Patients with speech initiation problems are quiet, as though they have nothing to say, so-called dynamic aphasia. Responses are terse and elaboration is absent. Patients speak only in response to conversation, not to initiate conversation. Although the amount of speech is reduced, the content and structure of spoken language are normal. This is often seen in patients with anterior frontal and subcortical abnormalities. These individuals often appear inert and slow to respond in general, sometimes referred to as appearing as a “bump on a log.”
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here