Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Epithelial/neuroectodermal/mesenchymal
Keratoacanthoma
Ceruminal gland neoplasms
Seborrheic keratoses
Squamous papilloma
Melanocytic nevi
Dermal adnexal neoplasms
Pilomatrixoma (calcifying epithelioma of Malherbe)
Neurilemmoma/neurofibroma
Osteoma; chondroma
Hemangioma
Others
Epithelial/neuroectodermal/mesenchymal
Basal cell carcinoma
Squamous cell carcinoma and variants
(Verrucous carcinoma, spindle cell squamous carcinoma, adenoid squamous cell carcinoma, others)
Ceruminal gland adenocarcinomas
Malignant melanoma
Merkel cell carcinoma
Atypical fibroxanthoma
Others
Epithelial
Middle ear adenoma
Middle ear papilloma
Others
Neuroectodermal/mesenchymal
Jugulotympanic paraganglioma
Meningioma
Acoustic neuroma
Others
Epithelial
Middle ear adenocarcinoma
Primary squamous cell carcinoma
Neuroectodermal/mesenchymal
Endolymphatic sac papillary tumor
Rhabdomyosarcoma
Vascular (angiosarcoma; Kaposi sarcoma)
Lymphoproliferative (malignant lymphoma; plasmacytoma)
Secondary tumors
Definition: Solitary squamous epithelial neoplasm believed to arise from hair follicles, frequently occurring on sun-exposed areas of the skin and characterized by rapid development followed by involution and spontaneous regression.
NOTE: Some experts believe that solitary keratoacanthomas represent squamous cell carcinoma with a real but limited ability to metastasize.
No gender predilection; most frequently seen in the sixth to seventh decades of life
Frequently develop on sun-exposed skin:
Majority occur on the face (most commonly on the cheek and nose)
Approximately 10% occur on the external ear (pinna); occasionally may occur on the lips
Usually a solitary lesion but multiple KAs occur
Initially the lesion appears as an erythematous papule or may resemble a wart but over a 1- to 2-month period undergoes rapid enlargement to appear as an exophytic or dome-shaped nodule with a central keratin crater measuring from 1 to 3 cm in diameter.
Typically arise rapidly (6 to 8 weeks) followed by a stationary period lasting up to several months which in turn is followed by involution with spontaneous regression ultimately leading to (crateriform) scar.
Whole growth process may be seen over periods of several months up to a year.
Etiology is unknown but is probably the result of actinic damage.
Multiple and syndromic keratoacanthomas exist and may occur in patients with genetic predisposition.
Less common variants include:
Giant keratoacanthoma:
Grows rapidly and reaches a size of 5 cm or more
May cause destruction of underlying tissues
Spontaneous involution occurs after several months.
Most common sites are the nose and eyelids.
Keratoacanthoma centrifugum marginatum:
May reach 20 cm in diameter
No tendency to spontaneous involution
Peripheral extension with raised, rolled border and central atrophy
Most common sites are dorsa of hands and legs
Subungual keratoacanthoma:
Aggressive behavior that fails to regress spontaneously
Destructive growth in distal portion under a fingernail
Described as part of Muir-Torre syndrome, which is characterized by:
Multiple neoplasms of the skin, including those with sebaceous differentiation and internal (visceral) neoplasms, the most common of which are of colonic origin (adenocarcinoma, adenoma)
In Muir-Torre syndrome, KAs may be one of multiple cutaneous lesions or represent the only type of cutaneous tumor present in this syndrome.
Early lesions appear as an erythematous papule or a wart-like growth.
Mature lesions are elevated and firm with an exophytic or dome-shaped appearance characterized by skin-colored edges and a central cavity or crater filled with keratin debris.
Measures from 1 to 3 cm and occasionally may reach sizes measuring up to 5 cm
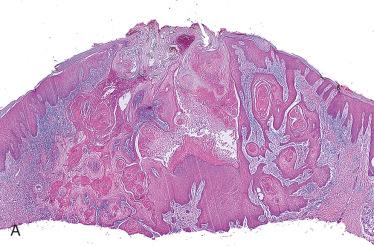
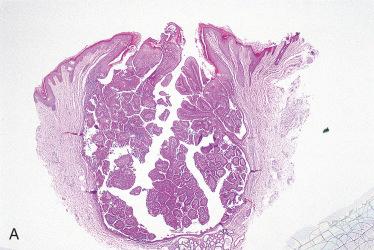
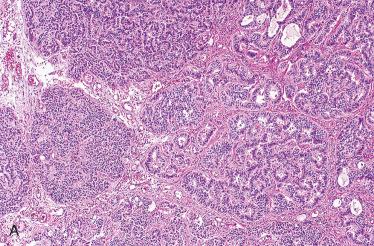
Cup-shaped symmetric lesion with deep bulbous lobules of squamous cells
Early lesion shows hyperkeratosis, parakeratosis, acanthosis with hypergranulosis, and papillomatosis with strands of atypical and dyskeratotic keratinocytes forming a central crater extending into the epidermis.
Mature lesions form a crater filled with hyper- and orthokeratotic material, below which is the epithelial proliferation composed of nests of large keratinocytes with a “glassy”-appearing or eosinophilic cytoplasm and prominent intercellular bridges.
Dyskeratosis and squamous pearl formation are commonly seen.
Transition area between the adjacent squamous epithelium and the hyperplastic epithelium forming the crater is noted by the formation of “shoulders,” a characteristic low-power finding.
A variable chronic inflammatory infiltrate may be seen in the dermis surrounding the lesion composed of mature lymphocytes, histiocytes, eosinophils, and polymorphonuclear leukocytes; neutrophilic intraepithelial “microabscesses” are often seen.
Vascular and perineural invasion may be seen.
With time the lesion involutes and is characterized by regression of the epithelial proliferation, a shallower central crater, granulation tissue proliferation, and fibrosis of the dermis.
Benign keratosis
Seborrheic keratosis, including inverted follicular keratoma
Squamous cell carcinoma:
Differentiation from squamous cell carcinoma is made on the basis of the overall architecture because cytologic atypia is not a reliable criterion for differentiating KA from squamous cell carcinoma.
Differentiation can be extremely difficult especially if less than adequate biopsy material is provided (e.g., from the central aspects of the tumor).
No reliable immunohistochemical staining and/or molecular biologic analyses allowing for differentiating KA from squamous cell carcinoma
Complete surgical excision is the preferred treatment and is curative.
Despite the result of involution and regression, keratoacanthomas should be treated surgically for the following reasons:
Cosmetic considerations
Allow for the best overall architectural evaluation to confirm the diagnosis and help differentiate from a squamous cell carcinoma
Treatment would be the same for a well-differentiated squamous cell carcinoma in this location.
A small percentage of cases may recur.
Keratoacanthomas have been reported to metastasize; however, the metastases have been squamous cell carcinomas, suggesting that the primary tumors may have also been squamous cell carcinomas.
Presence of vascular and/or perineural invasion are not findings indicative of malignancy.
Diagnosis of KA as opposed to squamous cell carcinoma can be made if certain conditions are met, including:
Clear-cut clinical description of the lesion is provided.
Clinical history of rapid evolving lesion with KA as the primary clinical diagnosis
No history of immunosuppression
Adequate biopsy provided allowing for complete visualization of the lesion
Classic histologic findings are identified.
In the absence of these conditions a diagnosis of squamous cell carcinoma is likely.
Definition: Benign tumor of cerumen-secreting modified apocrine glands (ceruminal glands) located in the external auditory canal.
Ceruminal gland tumors arise from the cerumen-secreting modified apocrine glands (ceruminal glands) in the external auditory canal:
Ceruminal glands are located in the dermis of the cartilaginous (inner) portion (outer third) of the external auditory canal.
In general, ceruminal gland neoplasms are uncommon but represent one of the more common tumors of the external auditory canal.
The generic designation of ceruminoma should be avoided; ceruminal gland neoplasms should be specifically diagnosed according to tumor type.
The classification of ceruminal gland neoplasms includes benign and malignant tumors ( Box 24-2 ):
Benign ceruminal gland tumors include:
Ceruminal gland adenoma
Pleomorphic adenoma
Syringocystadenoma papilliferum
Malignant ceruminal gland tumors include:
Ceruminal gland adenocarcinoma
Adenoid cystic carcinoma
Mucoepidermoid carcinoma

Affect men more often than women; over a wide age range but is most frequently seen in the fifth to sixth decades of life
Symptoms include a slow-growing external auditory canal mass or blockage, hearing difficulty, and infrequently, otic discharge.
Skin-covered, circumscribed, polypoid, or rounded mass ranging in size from 1 to 4 cm in diameter
Ulceration is uncommon and may suggest a malignant neoplasm.
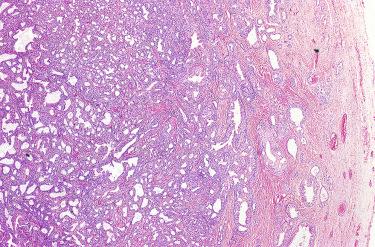
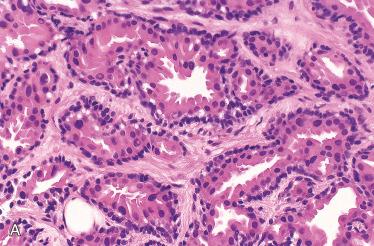
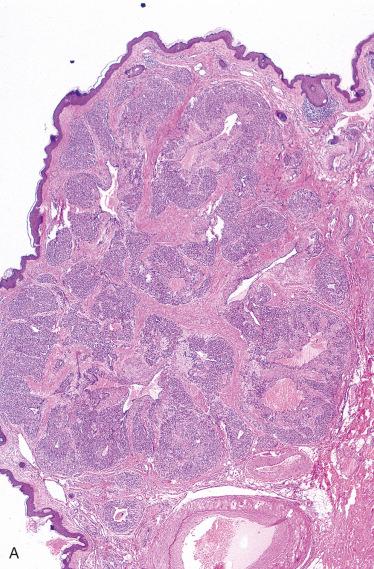
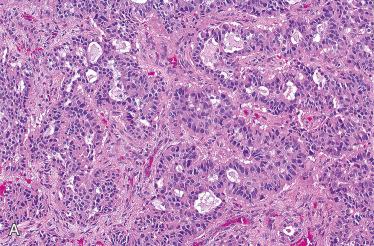
Unencapsulated but well-demarcated glandular proliferation
Glands vary in size and may have various combinations of growth patterns including solid, cystic, and papillary; a back-to-back glandular pattern is commonly seen.
Glands are composed of two cell layers:
Inner or luminal epithelial cell is cuboidal or columnar appearing with an eosinophilic cytoplasm and a decapitation-type secretion (apical “snouts”) characteristic for apocrine-derived cells.
Outer cellular layer is a spindle cell with a hyperchromatic nucleus and represents myoepithelial or basal cells.
Intracytoplasmic golden yellow-brown granular-appearing pigment can be seen in the inner lining (luminal) cells representing cerumen.
Cellular pleomorphism and mitoses can be seen but are not prominent.
Intervening stroma shows a variable admixture of fibromyxomatous tissue.
Histochemistry:
Diastase-resistant, PAS-positive, and/or mucicarmine-positive intracytoplasmic and/or intraluminal material may be seen.
Immunohistochemistry:
Luminal cells:
Strongly and diffusely immunoreactive with CK7; CD117 positive
Myoepithelial or basal cells:
CK5/6, S100 protein, and p63 positive
Ultrastructure:
Epithelial (apocrine cell) and myoepithelial cell differentiation including:
Epithelial cells show features of apocrine cells, including apocrine caps, microvilli, cell junctions, secretory granules, vacuoles, lipid droplets, and siderosomes.
Concentric membranous bodies of the endoplasmic reticulum, phagocytic activity of the tumor cells, intracytoplasmic lumina, ciliated cells, and also spiny collagen in the tumor stroma can be seen.
Pleomorphic adenoma of ceruminal or parotid gland origin
Middle ear adenoma:
May perforate the tympanic membrane and appear to present as an external auditory canal mass, creating potential difficulty in differentiation from a ceruminal gland adenoma
Histologic features of both tumor types should allow for relatively easy differentiation from one another.
Ceruminal gland adenocarcinoma
Complete surgical excision is the preferred treatment and is curative.
Recurrence of the tumor can occur and relates to inadequate surgical excision.
Uncommon tumor
Histology is similar to pleomorphic adenomas of salivary gland origin, including a variable admixture of epithelial and myoepithelial components set in a myxoid to chondromyxoid stroma.
Benign tumor of apocrine gland origin that usually occurs on the scalp and face area
May originate in the external auditory canal from ceruminal glands
Histology is similar to tumors of the more common cutaneous sites and to the salivary gland tumor termed sialadenoma papilliferum (see Section 6).

Epithelioid hemangioma (EH), also known as angiolymphoid hyperplasia with eosinophilia (ALHE), has been a controversial lesion with regard to its classification (reactive proliferation or neoplastic process) and its relationship to Kimura disease:
A reactive cause especially secondary to trauma has been proposed but a neoplastic origin is favored.
Considered to represent the benign end of the spectrum of vascular tumors characterized by epithelioid endothelial cells, many of which are rich in lymphocytes and eosinophils
Malignant end of the spectrum includes epithelioid hemangioendothelioma and epithelioid angiosarcoma.
Shares features with Kimura disease, but the clinical and histologic differences allow these entities to be separated and considered as distinct clinicopathologic entities ( Table 24-1 )
| EH | Kimura Disease | |
|---|---|---|
| Gender | M = F or F > M | M > F |
| Peak incidence | 3rd to 5th decades | 2nd to 3rd decades |
| Head and neck site | Periauricular, forehead | Postauricular, scalp |
| Lymphadenopathy | Absent to rare | Common |
| Peripheral eosinophilia | <25% | >50% |
| Location | More superficial situated in subcutaneous, dermis | More deeply situated extending to the subcutaneous fat, fascia, and skeletal muscle |
| Histology | Nodular vascular proliferation lined by plump-appearing (epithelioid) endothelial cells with pleomorphic changes and hyperchromatic nuclei, and accompanied by a prominent inflammatory cell infiltrate with variable admixture of lymphocytes, histiocytes, plasma cells, and eosinophils | Vascular component is sparse with minimal epithelioid endothelial changes; lymphoid proliferation predominates, but prominent eosinophilic cell infiltrate, including eosinophilic microabscesses can be seen; associated fibrosis is present |

No gender predilection; most frequently occurs in the third through fifth decades of life
Subcutaneous proliferation with a predilection for the external ear (auricle and external canal), as well as other head and neck sites, including the scalp and forehead ( Fig. 24-8 )
Symptoms include pruritus and bleeding following scratching; regional lymphadenopathy and peripheral eosinophilia are uncommon but may be present.
History of trauma elicited in a number of cases, as well as the microscopic impression of vascular damage, and the demonstration of immunoglobulin deposits in the vessels have led several observers to favor a reactive or reparative etiology.
Hormonal influences may play a role in some cases, as suggested by the association with pregnancy in some patients and by the age and gender distribution of the disease.
Human herpesvirus 8 (HHV-8) has not been identified in association with EH.
Characterized by single or multiple, pink to red-brown indurated cutaneous papules or subcutaneous nodules
Measure from a few millimeters to 1 cm in diameter
Clusters of papules may coalesce to form large plaque-like lesions.
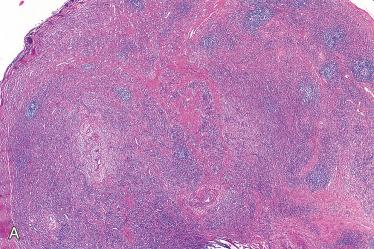
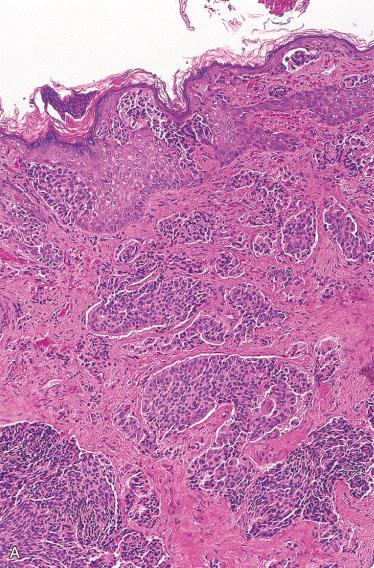
Characterized by a nodular vascular proliferation accompanied by a variably dense lymphoid infiltrate rich in eosinophils
Process is circumscribed but not encapsulated and may involve the subcutis or dermis, or both.
Vascular component:
Varies in size from capillary to medium-sized arteries and veins
Vascular spaces are lined by plump-appearing (epithelioid) endothelial cells with pleomorphism, hyperchromatic nuclei, copious eosinophilic cytoplasm, and inconspicuous nucleoli.
Frequently, the endothelial cells protrude into the vessel lumen in a “hobnail” fashion, creating a cobblestone-like appearance.
Increased mitotic activity and moderate to marked nuclear pleomorphism not identified
Lobular arrangement of the proliferating vessels may be evident; however, the distribution of vessels is more haphazard in some lesions:
Vessels vary from irregular, poorly canalized thin-walled spaces to rounded well-formed vessels with thickened walls.
In some cases there is evidence of disruption or damage to some of the involved vessels.
Origin from a small artery or vein is common but may depend on adequate sampling.
Common for the entire lesion to be intravascular (intravascular EH):
Differ from “conventional” EH by virtue of predominant spindle cell (pericytic) component
Predominantly occurs in young to middle-aged adults
Solitary nodule most often in head and neck or upper limb
Inflammatory component surrounds the vascular proliferation and is characterized by an admixture of lymphocytes, histiocytes, and eosinophils; on occasion, eosinophils may be few in number or absent.
Immunohistochemistry:
Endothelial cells are:
CD31, ERG, and to a lesser extent CD34 positive
Glucose transporter protein 1 (GLUT1) negative
Rarely cytokeratin positive
Lobular capillary hemangioma:
Prominence of epithelioid endothelial features and associated lymphoplasmacytic and eosinophilic infiltrate contrast with findings in hemangiomas.
Infantile hemangioma:
GLUT1 positive
Angiosarcoma:
Shows a diffusely infiltrative lesion composed of anastomosing vascular channels lined by pleomorphic cells with increased mitotic activity
Presence of the characteristic inflammatory infiltrate in EH typically not found in angiosarcoma
Local surgical excision or desiccation are the preferred treatments and are curative:
Rarely, lesions may regress.
Recurrence reported in up to one-third of cases
Metastasis virtually never occurs.
Superficial radiotherapy results in at least partial response in the majority of patients.
Intralesional or systemic steroids, cryotherapy, and intralesional vincristine, bleomycin, and fluorouracil not proven to be curative
Not considered synonymous with EH
Occurs in subcutis of the head and neck; other less common sites of involvement include groin, extremities, and chest wall
In contrast to EH:
Occurs primarily in Asians and tends to affect males
Often associated with regional lymphadenopathy and peripheral eosinophilia
Increased serum immunoglobulin E (IgE), proteinuria, and nephrotic syndrome may occur as part of the disease.
Tend to be larger lesions that are predominantly subcutaneous nodules with a tendency to occur in locations other than in the head and neck
Etiology is unknown:
Presence of peripheral eosinophilic and elevated serum IgE suggests immunologic reaction to an unknown stimulus.
Shares histologic features with EH but differences are seen, including:
Lymphoid proliferation, including germinal centers, predominates; the vascular component is sparse and exhibits minimal epithelioid endothelial changes.
Lesion is usually located much deeper than EH, often extending to the fascia and to skeletal muscle, and the subcutaneous fat is usually fibrotic.
Eosinophils are always numerous in Kimura disease but may be sparse or even absent in EH.
Eosinophilic epithelioid granulomatous reaction and/or eosinophilic microabscess formation may be identified.
Lobular capillary hemangioma
Angiosarcoma
Local surgical excision or desiccation are the preferred treatments and are curative.
Recurrence occasionally occurs.
Malignant transformation or association with malignancy not reported
Mesenchymal tumors of the external auditory canal are rare and include osteoma, chondroma, leiomyoma, schwannoma, and myxomas.
In contrast to exostosis, osteomas are true neoplasms of bone capable of unlimited growth.
Occurs in the external auditory canal presenting as an asymptomatic solitary mass
Histologically is composed of mature bone with associated intraosseous fibrovascular tissue
Surgery is curative.
Described in Carney complex as an autosomal-dominant syndrome complex that includes:
Cardiac myxomas:
May be associated with peripheral tumor emboli
Approximately one-quarter of all patients with cardiac myxomas die of its complications.
Cutaneous myxomas:
Tend to appear in early adulthood
Predilection for eyelids
Range from small sessile papules to large pedunculated, finger-like lesions
In most cases are multiple
Found in dermis or subcutis
Usually circumscribed
Significant percentage of patients may have myxoma of external ear:
85% of patients with myxoma of external ear have Carney complex
Spotty pigmentation:
Lentigines on face and vermilion border of lips
Blue nevi including epithelioid blue nevi
Endocrine disease/tumors:
Primary pigmented nodular adrenocortical disease causing Cushing syndrome
Pituitary adenoma causing acromegaly
Sexual precocity associated with testicular lesions (e.g., Sertoli cell tumor)
Thyroid diseases (hyperplasia)
Increase risk of pancreatic ductal and acinar cell neoplasms
Psammomatous melanotic schwannoma
Occasionally associated with breast lesions including multifocal myxoid fibroadenomas and myomatosis
Most patients with Carney complex harbor mutation of PRKAR1A gene located at 17q22-24 encoding regulatory R1 alpha subunit of protein kinase A.
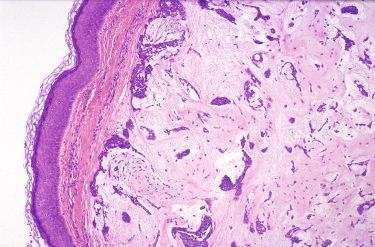
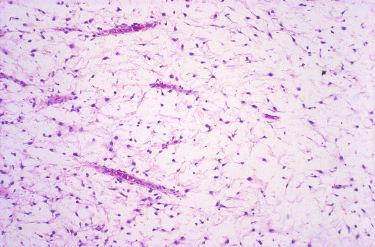
Histology characterized by the presence of sparse cytologically bland spindle- and stellate-shaped cells in abundant myxoid stroma and prominent capillary vasculature:
Lesion consists chiefly of mucoid material in which are suspended a loose framework of reticulin fibers.
Cellular component consists of a population of spindled to stellate cells with tiny pyknotic nuclei and delicate cytoplasmic process.
Cellular pleomorphism is not seen.
Periphery of the tumor is surrounded by a pseudocapsule of condensed reticulin fibers and compressed host tissue, particularly skeletal muscle.
Often associated with basaloid proliferation of overlying epithelium:
May result in misdiagnosis of basal cell carcinoma or trichofolliculoma
Myxoid matrix in myxoma stains with alcian blue and is hyaluronidase sensitive
Mucicarmine and colloidal iron stain the myxoid material.
Immunohistochemistry of cellular component includes:
CD34 and vimentin positive
Cells may stain for actins and/or desmin, suggesting myofibroblastic differentiation.
Typically negative for S100 protein, MUC4, cytokeratins
Myxoid neoplasms:
Myxoid change occurs in a variety of benign neoplasms, including neurofibroma, neurilemmoma, and lipoma, may mimic myxoma, especially in limited biopsy material.
Of greater concern is that the histologic pattern in myxomas may mimic myxoid soft tissue malignancies, which are much more common in this location, particularly embryonal rhabdomyosarcoma, and less commonly undifferentiated pleomorphic sarcoma, low-grade fibromyxoid sarcoma, myxoid liposarcoma, and myxoid chondrosarcoma.
In contrast to myxoma, sarcomas display:
Much greater cellularity
A richer vascular pattern often with delicate plexiform capillary vascular network
Differing cytologic features including cellular pleomorphism with increased mitotic figures; multinucleated giant cells in undifferentiated pleomorphic sarcoma; cytoplasmic MUC4 in low-grade fibromyxoid sarcoma; lipoblasts in liposarcoma; rhabdomyoblasts in rhabdomyosarcoma; and atypical chondroblasts in chondrosarcoma are distinctive features for these sarcoma types.
Surgery is the preferred treatment.
Although soft tissue myxomas lack a discrete capsule, they rarely recur after excision.
Definition: Benign glandular neoplasm arising from the middle ear mucosa.
Generally considered an uncommon neoplasm
No gender predilection; occurs over a wide age range but is most common in the third to fifth decades of life
Any portion of the middle ear may be affected, including the eustachian tube, mastoid air spaces, ossicles, and chorda tympani nerve.
Most common symptom is that of unilateral conductive hearing loss:
Fullness, tinnitus, and dizziness may also occur.
Pain, otic discharge, and facial nerve paralysis rarely occur and may be indicative of a malignant process.
Otoscopic examination in the majority of cases will identify an intact tympanic membrane with tumor confined to the middle ear space with possible extension to the mastoid; occasionally, the adenoma will perforate through the tympanic membrane with extension into and presentation as an external auditory canal mass.
No known etiologic factors related to the development of MEA:
Not associated with a prior history of chronic otitis media
Concurrent cholesteatomas may be seen but there is no known association between these two lesions.
Radiologic imaging:
In its more typical radiologic presentation, appears as a relatively avascular soft tissue density without evidence of destructive, invasive, or erosive properties.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here