Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acute kidney injury (AKI), previously referred to as “acute renal failure”, is defined by an abrupt change in the glomerular filtration rate with rising serum creatinine levels or decrease in urine output. AKI is associated with adverse outcomes.
The newborn kidney undergoes a number of physiologic and functional changes after birth that impact its function and increase the susceptibility to AKI.
The risk of AKI is higher in premature and critically ill infants; those with systemic illness due to birth asphyxia, sepsis, or necrotizing enterocolitis; and infants with congenital heart disease under/after treatment with extracorporeal membrane oxygenation or after cardiac surgery/cardiopulmonary bypass.
AKI has been associated with nephrotoxic medications, including antibiotics such as aminoglycosides and vancomycin, nonsteroidal antiinflammatory drugs, and diuretics.
The KDIGO (Kidney Disease: Improving Global Outcomes) classification is a useful tool for early identification of AKI severity.
Several ongoing research studies seek to measure/monitor kidney function, determine the risk of AKI and the impacts of its early identification, and identify potential treatment options.
During the past decade, there have been extraordinary advances in our understanding of neonatal acute kidney injury (AKI). During this time, it has become clear that AKI occurs commonly in critically ill neonates and is associated with adverse outcomes irrespective of the specific neonatal population studied. AKI is no longer considered a symptom of illness severity but instead an independent risk factor for adverse outcomes, impacting short-term outcomes (length of mechanical ventilation, length of stay, and mortality) as well as long-term kidney health (subsequent chronic kidney disease [CKD] and hypertension).
Neonates with AKI represent some of the most challenging patients encountered in the intensive care unit. A firm understanding of AKI risk factors and pathophysiology is necessary for neonatal providers as well as an appreciation of the unique characteristics of neonatal AKI. This chapter provides a comprehensive overview of neonatal AKI including developmental considerations, definitions, epidemiology and risk factors, evaluation, novel approaches, management, and long-term outcomes.
In order to appreciate the intricacies of neonatal AKI, an understanding of nephrogenesis and the dynamic kidney function changes that occur after birth is critical. A detailed understanding of these processes is outside the scope of this chapter, but this section will serve as a primer to better understand the pathophysiology and potential impact of neonatal AKI on outcomes.
Nephrons are the functional units of the kidney, and their development occurs until 36 weeks’ gestation. At 15 weeks’ gestation there are on average 15,000 nephrons and by 40 weeks of gestation, 745,000 nephrons, with 60% of nephrogenesis occurring in the third trimester.
Animal models and neonatal autopsy studies have shed light on the impact of premature birth on nephron endowment and structure. Altered glomerular structure in 0.2% to 18% of glomeruli in the outer renal cortex has been found in a preterm baboon model. Premature mice models have shown reduced nephron number with subsequent development of reduced glomerular filtration rate (GFR), proteinuria, and hypertension in adulthood. In a postmortem study of human preterm neonatal kidneys, infants who were born preterm and survived for a period of time were noted to have accelerated maturation and abnormal glomerular morphology in comparison with stillbirth controls. Abnormal glomerular morphology may result in later glomerular loss, resulting in hypertension and CKD. This altered glomerular morphology and function in the preterm neonatal kidney is associated with a reduced capacity to respond to insults and an increased susceptibility to injury. As a result, premature birth results in lower nephron endowment, placing the kidney at risk for adverse short- and long-term outcomes.
After birth, the newborn kidney undergoes a number of physiologic and functional changes that impact function and susceptibility to AKI. At birth, the kidneys receive only 2.5% to 4% of total cardiac output compared to 20% to 25% in adults. This increases to 6% at 24 hours of life, 10% at the end of the first week, and 15% to 18% at 6 weeks of age. These changes are driven by increased peripheral vascular resistance and decreased renal vascular resistance. Perfusion in the newborn kidney is dependent on a delicate balance of vasodilatory and vasoconstrictive factors. The greater reliance on factors such as prostaglandins and angiotensin to maintain renal blood flow in the neonatal kidney explains the most potent, adverse impact of medications such as nonsteroidal antiinflammatory drugs and angiotensin converting enzyme inhibitors on kidney function.
Changes in kidney function parallel increases in renal blood flow. GFR is also considerably lower at birth than later in life. In term infants, GFR is 10 to 20 mL/min/1.73 m 2 , increasing to 30 to 40 mL/min/1.73 m 2 by the second week of life and increasing steadily during the ensuing months to reach an adult level by 2 years of age. Preterm neonates have an even lower GFR at birth that increases at a slower rate compared with term infants. Due to tubular immaturity, preterm neonates excrete higher amounts of sodium and have less ability to concentrate urine than do healthy, term infants and adults. This has implications for susceptibility to AKI because increased sodium excretion can be accompanied by significant diuresis, leading to hypovolemia. This risk for AKI is potentially compounded by exposures to nephrotoxic medications in the face of volume depletion.
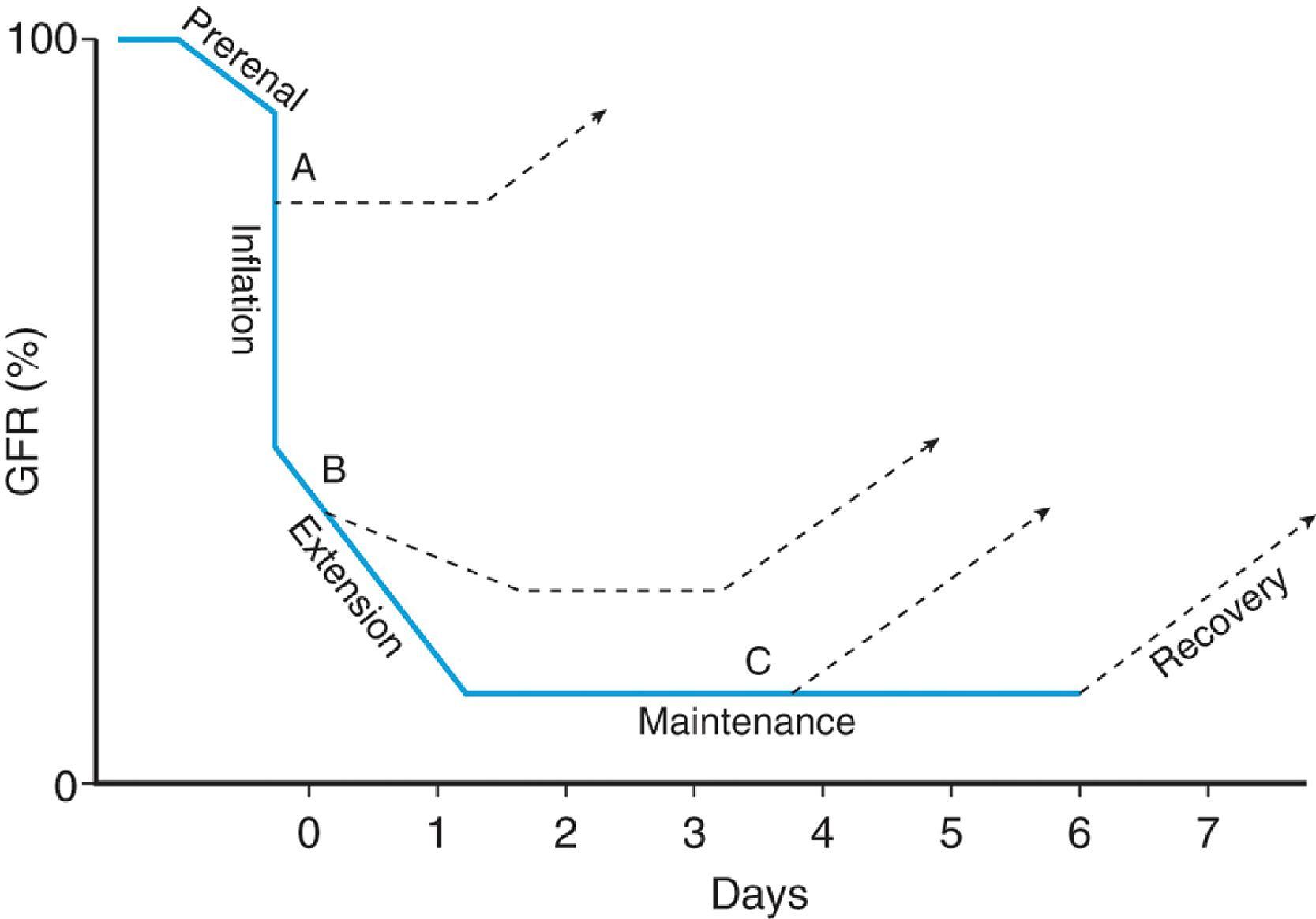
AKI, previously referred to as “acute renal failure,” is defined by an abrupt change in GFR ( Fig. 58.1 ) identified by a rise in serum creatinine (SCr) or decrease in urine output. SCr is known to be an imperfect clinical biomarker for AKI but remains the gold standard for diagnosis at this time. In general, SCr is a delayed marker of AKI (elevated 48–72 hours after insult) and reflects changes in function rather than ongoing tubular damage. Defining AKI in neonates is further complicated by dynamic changes in renal physiology after birth, as noted above, and the presence of maternal SCr. With the increase in GFR that occurs in the first weeks of life, SCr slowly decreases. However, the trajectory of declining SCr is also highly dependent on gestational age (GA) with a slower decline seen in lower GA infants. ,
During the past two decades there has been a transition from threshold-based definitions of AKI to staged definitions that represent the entire spectrum of injury that typifies AKI. These definitions include the Risk, Injury, Failure, Loss, and End stage renal disease (RIFLE), the Acute Kidney Injury Network classification (AKIN), and most recently, the Kidney Disease: Improving Global Outcomes (KDIGO) definition. A multitude of studies have been performed using these staged definitions of AKI in a variety of neonatal populations. This important work led to the development of a consensus neonatal definition of AKI.
In 2013, an expert working group consisting of neonatologists and nephrologists at a National Institutes of Health–sponsored neonatal AKI workshop agreed that the neonatal modified KDIGO definition should be used as a consensus definition for neonatal AKI ( Table 58.1 ). The modifications of the neonatal KDIGO definition include a reference SCr value, defined as the lowest previous SCr value and an absolute SCr cutoff of ≥2.5 mg/dL (221 μmol/L) to define severe AKI (stage 3). Using this definition, single-center studies and the multicenter AWAKEN (Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates) study have clearly shown AKI occurs commonly in the neonatal intensive care unit (NICU) and is associated with adverse outcomes.
| Stage | SCr Criteria | Urine Output Criteria a |
|---|---|---|
| 0 | No change in SCr or rise < 0.3 mg/dL | >0.5 mL/kg/hour |
| 1 | SCr rise ≥ 0.3 mg/dL within 48 hours or SCr rise ≥ 1.5−1.9 × reference SCr b within 7 days |
<0.5 mL/kg/hour for 6–12 hours |
| 2 | SCr rise ≥ 2–2.9 × reference SCr b | <0.5 mL/kg/hour for >12 hours |
| 3 | SCr rise ≥ 3 × reference SCr b or SCr ≥ 2.5 mg/dL or Receipt of dialysis |
<0.3 mL/kg/hour for >24 hours or anuria for >12 hours |
a Urine output for the AWAKEN study was collected over a 24-hour period and differed slightly from these criteria.
b Reference SCr, defined as the lowest previous SCr value. KDIGO, Kidney Disease: Improving Global Outcomes; SCr, serum creatinine.
In discussions about AKI definitions, it is critical to consider urine output. Although urine output criteria have been included in every AKI staging iteration, they have rarely been systematically studied. This largely stems from the challenges of quantifying urine output and retrieving this data from medical records. As a result, the contribution of urine output to AKI has largely been ignored in the AKI literature until recently. Recent multicenter work in critically ill children and neonates has clearly shown that AKI as defined by urine output identifies distinct episodes of AKI associated with adverse outcomes that would have been missed by SCr-based criteria alone. , Although there remain important questions about the optimal threshold and duration of oliguria, it is clear that urine output is a critical component to the definition of neonatal AKI.
It is important to appreciate that the authors of the consensus statement acknowledge the fact that the neonatal modified KDIGO definition represents a starting point for an iterative process in defining neonatal AKI. In an effort to begin to interrogate the current definition of neonatal AKI, a secondary analysis of the AWAKEN study data was undertaken to evaluate optimal definitions based on GA. The study identified a number of opportunities for optimization of the neonatal AKI definition, including unique SCr rise cutoffs for different GAs. The optimal absolute SCr rise thresholds to predict mortality were ≥0.3 mg/dL (≥26.5 μmol/L) for <29 weeks’ GA and ≥0.1 mg/dL (≥8.85 μmol/L) for ≥29 weeks GA. Further prospective studies are needed to determine the optimal SCr-based neonatal AKI definition for both clinicians and researchers. Until further work is done and subsequent consensus modifications of the neonatal AKI definition are published, it is recommended that clinicians and researchers use the neonatal modified KIDGO criteria to define neonatal AKI.
Despite the many recent advances in our understanding of neonatal AKI, there are no evidence-based treatments for AKI. As a result, it is critical to understand which neonatal populations are at highest risk to develop AKI. Single-center work has clearly shown that there are identifiable patient factors and disease characteristics that predispose neonates to AKI. The AWAKEN study has provided a large, multicenter, retrospective review of risk factors for AKI in both the early (first 7 days) and later neonatal period. ,
Several specific populations of neonates are known to be at high risk for AKI, including premature neonates (particularly very low birth weight [VLBW, i.e., birth weight <1,500 g] and extremely low birth weight [ELBW, i.e., birth weight <1,000 g] infants) and infants with specific diseases processes including sepsis, necrotizing enterocolitis (NEC), and hypoxic-ischemic encephalopathy (HIE), as well as those infants who reuire extracorporeal membrane oxygenation, and those with congenital heart disease requiring cardiac surgery. Preterm infants, especially VLBW and ELBW infants, are known to be at particularly high risk for AKI given the dynamic changes in renal blood flow and physiology after birth compounded by lower nephron endowment as described above. These vulnerable patients are also known to have prolonged hospitalizations with potential for multiple episodes of AKI and are particularly sensitive to other perinatal factors and nephrotoxins. Table 58.2 includes epidemiologic study findings for premature, VLBW, and ELBW infants, specifically. The epidemiology, as well as the pathophysiology believed to be underlying the increased risk for AKI in each of these conditions, is shown in Table 58.3 .
| Classification | Study | Incidence of AKI | Findings |
|---|---|---|---|
| Premature infants | Ladeiras 2018 (n = 106) |
22.6% |
|
| Shalaby 2018 (n = 214) |
56% |
|
|
| Elmas 2018 (n = 105) |
20% |
|
|
| Stojanovic 2017 (n = 195) |
44% |
|
|
| Nagaraj 2016 (n = 450) |
12% | ||
| Weintraub 2016 (n = 357) |
30.3% |
|
|
| Stoops 2016 (n = 125) |
30.5% |
|
|
| Stojanovic 2014 (n = 150) |
26% |
|
|
| VLBW and ELBW infants | Askenazi 2015 (n = 122) |
30% |
|
| Chowdhary 2018 (n = 483) |
60% |
|
|
| Srinivasan 2018 (n = 457) |
19.5% |
|
|
| Daga 2017 (n = 115) |
22.6% |
|
|
| Lee 2017 (n = 276) |
56% |
|
|
| Carmody 2014 (n = 455) |
39.8% |
|
|
| Rhone 2014 (n = 107) |
26.2% |
|
|
| Koralkar 2011 (n = 229) |
18% |
|
a Functional kidney failure was defined as all cases without oliguria but with persistently deranged kidney function (i.e., a minimum of two abnormal values taken 24 hours apart) and cases of oliguria that responded to a challenge test, with kidney sonography not revealing any abnormality and with no persistent biochemical derangement.
b Intrinsic kidney failure was defined as cases with oliguria responding to a challenge test but having either persistent biochemical derangement of kidney function or kidney sonography demonstrating altered echo texture.
| High AKI Risk Conditions | Pathophysiology | Epidemiology | |
|---|---|---|---|
| Study | Findings | ||
| Sepsis | Kidney hypoperfusion, ischemia, direct injury of kidney tubule cells, inflammation, and apoptosis all play a significant role Effects on the microcirculation are associated with organ dysfunction , AKI can occur despite maintenance of systemic BP and RBF in septic episodes , |
Vachvanichsanong 2012 (n = 139) |
|
| Mathur 2006 (n = 200) |
|
||
| NEC | May be associated with bacteremia, systemic inflammation; animal models show widespread kidney inflammation, disruption of tight junction proteins, and AKI | Bakhoum 2019 (n = 77) |
|
| Criss 2018 (n = 181) |
|
||
| HIE |
|
Chock 2018 (n = 38) |
|
| Medani 2014, Karlo 2014, Matyanga 2013 |
|
||
| Alaro 2014 (n = 60) |
|
||
| Sarkar 2014 (n = 88) |
|
||
| Selewski 2013 (n = 96) |
|
||
| ECMO |
|
Mallory 2019 (n = 424) |
|
| Fleming 2016 (n = 832) |
|
||
| Zwiers 2013 (n = 242) |
|
||
| Askenazi 2011 (n = 7941) |
|
||
| Congenital heart disease and cardiac surgery |
|
SooHoo 2018 (n = 95) |
|
| Mah 2018 (n = 117) |
|
||
| Kumar 2016 (n = 102) |
|
||
| Piggott 2015 (n = 95) |
|
||
| Alabbas 2013 (n = 122) |
|
||
| Morgan 2013 (n = 264) |
|
||
| Blinder 2012 (n = 430) |
|
||
Single-center NICU studies using modern, staged definitions of neonatal AKI, similar to the modified neonatal KDIGO classification, have clearly shown that AKI occurs commonly and is associated with adverse outcomes. The AWAKEN study, the only large multicenter NICU study to date including more than 2000 infants, revealed a similar AKI incidence to prior single-center studies at 29.9% using SCr and urine output KDIGO criteria. AKI incidence varied by GA groups (22–29 weeks’: 49.7%; 29–36 weeks’: 18.3%; and >36 weeks’: 36.7%). When classified according to highest AKI stage, 46.4%, 23.6%, and 29.9% of patients with AKI were classified as stages 1, 2, and 3, respectively. After adjusting for several potential confounders, infants with AKI had 4.6 times higher odds of mortality (95% CI, 6.1–11.5 times) and stayed in hospital 8.8 days longer (95% CI, 6.1–11.5 days). Data from this landmark study confirm the strong association of the neonatal KDIGO definition with poor outcomes observed in single-center studies.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here