Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Geriatric assessment is a multidimensional, usually interdisciplinary, diagnostic process intended to determine a frail older person's medical, psychosocial, and functional capabilities and problems, with the objective of developing an overall plan for treatment and long-term follow-up. It differs from the standard medical evaluation in its concentration on frail older adults, with their complex problems, emphasis on functional status and quality of life, and frequent use of interdisciplinary teams and quantitative assessment scales.
The process of geriatric assessment can range in intensity from a limited assessment by primary care physicians or community health workers focused on identifying an older person's functional problems and disabilities (screening assessment) to a more thorough evaluation of these problems by a geriatrician or multidisciplinary team (comprehensive geriatric assessment [CGA]), often coupled with initiation of a therapeutic plan. This chapter discusses limited geriatric assessment, such as that which can be performed by a single practitioner in an office setting, and CGA, usually requiring a specialized geriatric setting.
Because the ultimate goal of geriatric assessment is to improve the quality of life for older adults, readers may find Figure 34-1 helpful. As diagrammed, quality of life includes health status and socioeconomic and environmental factors. Health status can be quantified by measures of disease, such as signs, symptoms, and laboratory tests, and by measures of functional status. By functional status, we mean the individual's ability to participate fully in the physical, mental, and social activities of daily life. The ability to function fully in these areas is strongly affected by an individual's physiologic health and can often be used as a measure of the seriousness of a patient's multiple diseases. A CGA should be able to evaluate and plan care for all these areas.
The basic concepts of geriatric assessment have evolved over the past 80 years by combining elements of the traditional medical history and physical examination, social worker assessment, functional evaluation, treatment methods derived from rehabilitation medicine, and psychometric methods derived from the social sciences. By incorporating the perspectives of many disciplines, geriatricians have created a practical means of viewing the whole patient.
The first published reports of geriatric assessment programs came from the British geriatrician Marjory Warren, who initiated the concept of specialized geriatric assessment units during the late 1930s while in charge of a large London infirmary. This infirmary was filled primarily with chronically ill, bedridden, and largely neglected older patients who had not received proper medical diagnosis or rehabilitation and who were thought to be in need of lifelong institutionalization. Good nursing care kept the patients alive, but the lack of diagnostic assessment and rehabilitation kept them disabled. Through evaluation, mobilization, and rehabilitation, Warren was able to get most of the long bedridden patients out of bed and often discharged home. As a result of her experiences, Warren advocated that every older adult patient receive comprehensive assessment and an attempt at rehabilitation before being admitted to a long-term care hospital or nursing home.
Since Warren's work, geriatric assessment has evolved. As geriatric care systems have been developed throughout the world, geriatric assessment programs have been assigned central roles, usually as focal points for entry into the care systems. Geared to differing local needs and populations, geriatric assessment programs vary in intensity, structure, and function. They can be located in different settings, including acute hospital inpatient units and consultation teams, chronic and rehabilitation hospital units, outpatient and office-based programs, and home visit outreach programs. Despite diversity, they share many characteristics. Virtually all programs provide multidimensional assessment using specific measurement instruments to quantify functional, psychological, and social parameters. Most use interdisciplinary teams to pool expertise and enthusiasm in working toward common goals. Additionally, most programs attempt to couple their assessments with an intervention, such as rehabilitation, counseling, or placement.
Today, geriatric assessment continues to evolve in response to increased pressures for cost containment, avoidance of institutional stays, and consumer demands for better care. Geriatric assessment can help achieve improved quality of care and plan cost-effective care. This has generally meant more emphasis on noninstitutional programs and shorter hospital stays. Geriatric assessment teams are well positioned to deliver effective care for older adults with limited resources. Geriatricians have long emphasized the judicious use of technology, systematic preventive medicine activities, and less institutionalization and hospitalization.
Geriatric assessment begins with the identification of deteriorations in health status or the presence of risk factors for deterioration. These deteriorations include worsening of disease and worsening of functional status. If disease alone has worsened, without affecting function, the patient should be able to be cared for in the usual primary care settings. In addition, when functional status problems are mild and are not rapidly progressive, it is appropriate for a primary care practitioner to proceed with the assessment. However, because families and patients identify functional status problems early, and because internists and family practitioners often are unfamiliar with the concept of “treating” functional status impairment as a problem in its own right, patients often self-refer to geriatric care settings for these functional status problems, when such settings are available. Patients who have new severe or progressive deficits should ideally receive comprehensive multidisciplinary geriatric assessment. Figure 34-2 outlines an approach for evaluating older outpatients with health status deterioration and deciding who should be referred to multidimensional geriatric assessment settings.
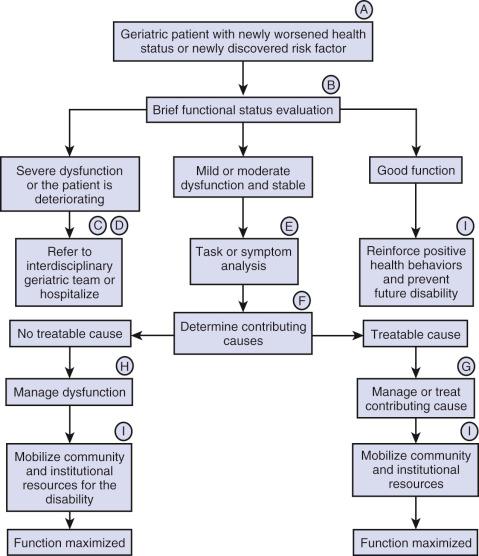
Using this approach, an older patient with a deteriorating health status of any type, whether it is a markedly elevated blood glucose level, vertebral collapse, or new inability to perform errands, should be evaluated briefly to determine the full extent of functional disabilities. Many experts believe that frail older adults, defined generally as people older than 75 years or older than 65 years with chronic disease, should also be screened for functional disability or risk factors at regular intervals, such as once a year, even when no known acute health insults have occurred. When a new disability or high-risk state is detected through screening, such patients may also be appropriate for a full geriatric assessment.
A typical geriatric assessment begins with a functional status review of systems that inventories the major domains of functioning. The major elements of this review of systems are captured in two commonly used functional status measures—basic activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Several reliable and valid versions of these measures have been developed, perhaps the most widely used being those by Katz and colleagues, Lawton and Brody, and Wade and Colin. These scales are used by clinicians to detect whether the patient has problems performing activities that people must be able to accomplish to survive without help in the community. Basic ADLs include self-care activities, such as eating, dressing, bathing, transferring, and toileting. Patients unable to perform these activities will generally require 12- to 24-hour support by caregivers. IADLs include heavier housework, going on errands, managing finances, and making phone calls, activities that are required if the individual is to remain independent in a house or apartment.
To interpret the results of impairments in ADLs and IADLs, physicians will usually need additional information about the patient's environment and social situation. For example, the amount and type of caregiver support available, strength of the patient's social network, and level of social activities in which the patient participates will all influence the clinical approach taken in managing deficits detected. This information could be obtained by an experienced nurse or social worker. A screen for mobility and fall risk is also extremely helpful in quantifying function and disability, and several observational scales are available. An assessment of nutritional status and risk for undernutrition is also important in understanding the extent of impairment and for planning care. Likewise, a screening assessment of vision and hearing will often detect crucial deficits that need to be treated or compensated for.
Two other key pieces of information must always be gathered in the face of functional disability in an older adult. These are a screen for mental status (cognitive) impairment and a screen for depression. Of the many validated screening tests for cognitive function, the Folstein Mini-Mental State Examination and the Kokmen Short Test of Mental Function are among the best because they efficiently test the major aspects of cognitive functioning and have been available for many years. Of the various screening tests for geriatric depression, the Yesavage Geriatric Depression Scale and PHQ-9 (depression screen of the Patient Health Questionnaire) are in wide use, and even shorter screening versions are available without significant loss of accuracy.
The major measurable dimensions of geriatric assessment, together with examples of commonly used health status screening scales, are listed in Table 34-1 . The instruments listed are short, have been carefully tested for reliability and validity, and can be easily administered by virtually any staffperson involved with the assessment process. Both observational instruments (e.g., physical examination) and self-report (completed by patient or proxy) are available. Their components of them, such as watching a patient walk, turn around, and sit down, are routine parts of the geriatric physical examination. Many other types of assessment measures exist and can be useful in certain situations. For example, there are several disease-specific measures for stages and levels of dysfunction for patients with specific diseases such as arthritis, dementia, and parkinsonism. There are also several brief global assessment instruments that attempt to quantify all dimensions of the assessment in a single form. These latter instruments can be useful in community surveys and some research settings but are not detailed enough to be useful in most clinical settings. More comprehensive lists of available instruments can be found by consulting published reviews of health status assessment.
| Dimension | Basic Context | Examples |
|---|---|---|
| Basic ADLs | Strengths and limitations in self-care, basic mobility, and incontinence | Katz (ADLs) ; Lawton Personal Self-Maintenance Scale ; Barthel index |
| IADLs | Strengths and limitations in shopping, cooking, household activities, and finances | Lawton (IADLs) ; Older Americans Resources and Services, IADL section |
| Social activities and supports | Strengths and limitations in social network and community activities | Lubben Social Network Scale ; Older Americans Resources and Services, social resources section |
| Mental health, affective | The degree to which the person feels anxious, depressed, or generally happy | Yesavage Geriatric Depression Scale ; PHQ-9 |
| Mental health, cognitive | The degree to which the person is alert, oriented, and able to concentrate and perform complex mental tasks | Folstein Mini-Mental State ; Kokmen Short Test of Mental Function |
| Mobility, gait, and balance | Quantitative scale of gait, balance, and risk of falls | Tinetti Performance-Oriented Mobility Assessment ; Get Up and Go Test |
| Nutritional adequacy | Current nutritional status and risk of malnutrition | Nutrition Screening Initiative Checklist ; Mini-Nutritional Assessment |
A number of factors must be taken into account in deciding where an assessment should take place, outlined in Table 34-2 . Mental and physical impairment make it difficult for patients to comply with recommendations and navigate multiple appointments in multiple locations. Functionally impaired older adults must depend on families and friends, who risk losing their jobs because of chronic and relentless demands on time and energy in their roles as caregivers, and who may be older adults themselves. Each separate medical appointment or intervention has a high time cost to these caregivers. Patient fatigue during periods of increased illness may require the availability of a bed during the assessment process. Finally, enough physician time and expertise must be available to complete the assessment within the constraints of the setting.
| Parameter | Office Setting | Outpatient or Home Care Team | Inpatient Unit or Team |
|---|---|---|---|
| Level of disability | Low | Intermediate | High |
| Cognitive dysfunction | Mild | Mild to severe | Moderate to severe |
| Family support | Good | Good to fair | Good to poor |
| Acuity of illness | Mild | Mild to moderate | Moderate to severe |
| Complexity | Low | Intermediate | High |
| Transportation access | Good | Good | Good to poor |
Most geriatric assessments do not require the full range of technology nor the intense monitoring found in the acute-care inpatient setting. However, hospitalization becomes unavoidable if no outpatient setting provides sufficient resources to accomplish the assessment fast enough. A specialized geriatric setting outside an acute hospital ward, such as a day hospital or subacute inpatient geriatric evaluation unit, will provide the easy availability of an interdisciplinary team with the time and expertise to provide needed services efficiently, an adequate level of monitoring, and beds for patients unable to sit or stand for prolonged periods. Inpatient and day hospital assessment programs have the advantages of intensity, rapidity, and ability to care for particularly frail or acutely ill patients. Outpatient and in-home programs are generally cheaper and avoid the necessity of an inpatient stay.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here