Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The genomic revolution is inexorably changing our understanding of nearly all medical conditions, and it is changing our clinical practices in the fields of diagnostic pathology and oncology. Indeed, genomic biomarkers have dramatically improved clinical algorithms for diagnosis, prognosis, treatment, and disease monitoring of cancer. It is now well recognized that all clonal neoplasms result from accumulating alterations in the genome that are usually acquired or “somatic” in nature. , Occasionally, there are inherited or “germline” genetic alterations that increase an individual’s chances of acquiring sufficient mutations in order to form a neoplasm. The genomic landscape of the most common cancer types have now been largely described by large sequencing efforts including The Cancer Genome Atlas (TCGA) program and the International Cancer Genome Consortium (ICGC). The development of a genome atlas for all cancer types has been accompanied by the development of targeted therapies.
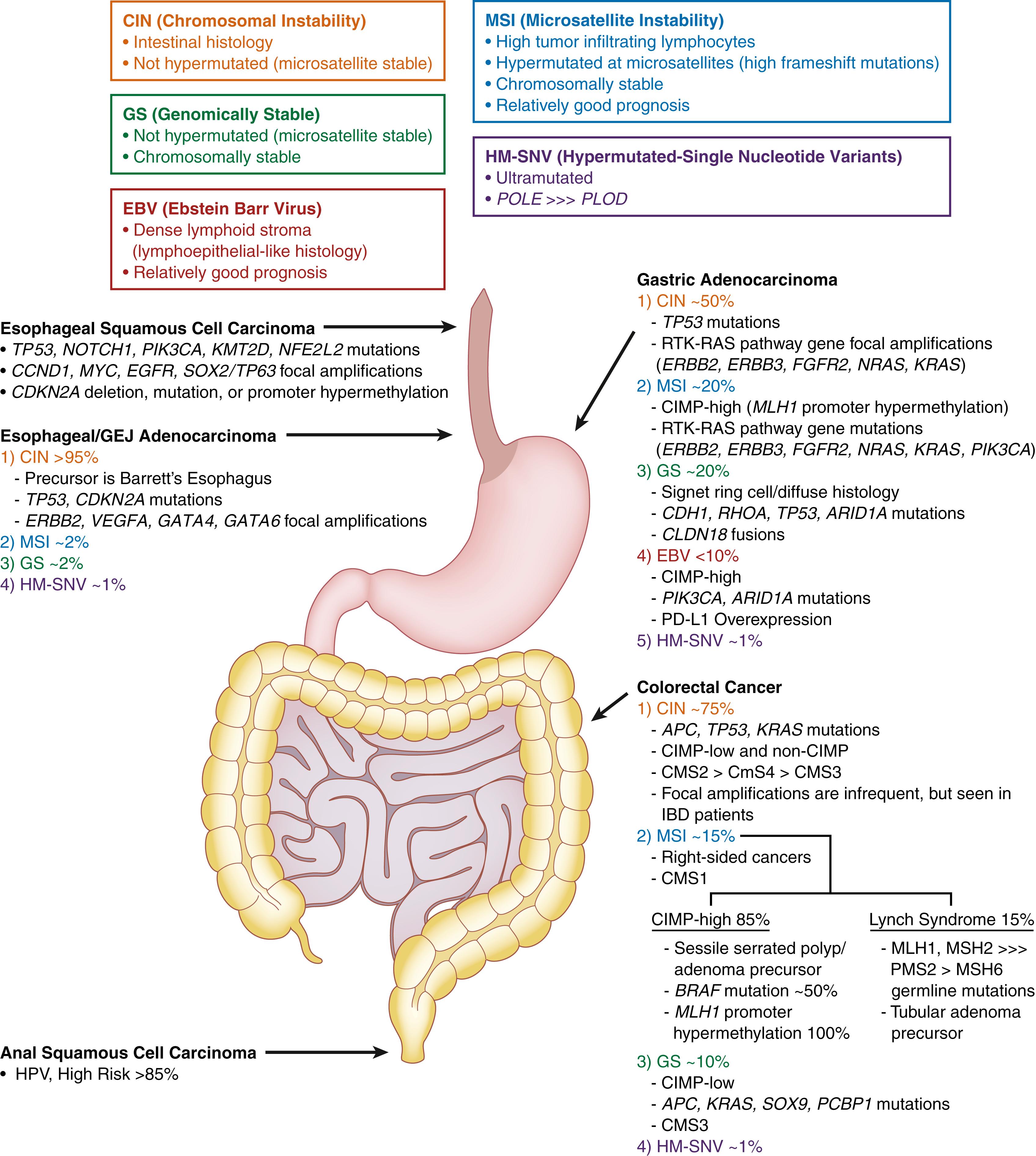
This chapter will highlight the most common molecular alterations of tubal gastrointestinal (GI) tract neoplasms ( Fig. 23.1 ) and will discuss the clinically relevant alterations and methodologies most commonly used for molecular testing in clinical practice ( Table 23.1 ). Although this chapter does not provide a comprehensive reference of all genetic alterations in all tubal gut neoplasms or an exhaustive treatise on the specific intricacies of all molecular diagnostic techniques, it outlines the molecular techniques routinely used in diagnostic laboratories, with a specific focus on the advantages and limitations for each methodology. The goal of this chapter is to help practicing GI pathologists select the best method of testing for each type of cancer specimen that will achieve the best molecularly integrated diagnosis and fulfill the standard of care of molecular testing for optimal clinical management.
| Detection Method | Types of Alterations That Can Be Detected | Examples | Tissue Requirement | Tumor Fraction Requirement | Advantages | Disadvantages | ||
|---|---|---|---|---|---|---|---|---|
| Single-gene methods | Performed in situ on a tissue section | Immunohistochemistry | Point mutations | BRAF p.V600E, IDH1 p. R132H, TP53 dominant-negative hotspots | Single unstained section per antibody | Tumor fraction can be low because analysis occurs in situ | Widely available, rapid turnaround time, inexpensive, limited tissue and tumor content requirement | A negative result does not exclude mutations in the gene as only one amino acid change is detected. For example, IDH1 p. R132C would not be detected |
| Gene amplification or gene expression caused by fusion event | ERBB2 (HER2), NTRK, STAT6 | Staining result could be equivocal. Example: 2+ Her2 staining | ||||||
| Loss-of-function mutation (frameshift, nonsense, splicing) or deletion of tumor suppressor | MLH1, MSH2, MSH6, PMS2, SDHB, TP53 | Loss of staining can be difficult to interpret | ||||||
| Promoter hypermethylation causing loss of tumor suppressor expression | MLH1, SDHB | Antibodies are not widely available for most molecular alterations | ||||||
| FISH or CISH | Amplification of a gene | ERBB2 (HER2) | Single unstained section per probe set | Tumor fraction can be low because analysis occurs in situ | Widely available, rapid turnaround time, relatively inexpensive, limited tissue and tumor content requirement | Can only assay a single gene per test | ||
| Deletion of a gene | CDKN2A, PTEN | |||||||
| Gene rearrangements/fusions | EWSR1, PRKACA rearrangement | Break-apart probes can capture any rearrangement involving EWSR1, but cannot tell you the fusion partner | ||||||
| Detection of oncogenic viruses | EBV, HPV | |||||||
| Requires purification of nucleic acids | PCR | Hotspot mutations, microsatellite instability, promoter hypermethylation (needs bisulfite treatment) | BRAF V600E, microsatellite instability, MLH1 promoter hypermethylation | 5-10 unstained slides for extraction of tumor DNA | ≥40% tumor fraction required for MSI, MLH1 promoter methylation ∗ | Fast and inexpensive | MSI does not inform as to which of the four mismatch repair proteins is mutated or hypermethylated | |
| Reverse transcriptase PCR | Gene fusions | EWSR1-FLI1 fusion, DNAJB1-PRKACA fusion | 5-10 unstained slides for extraction of tumor RNA and generation of cDNA | Can be low because sensitivity is high | Easy to generate primers for any gene fusion of interest, can determine the fusion partner | RNA in FFPE samples can be degraded; may require multiple primer pairs to detect fusion transcripts with different breakpoints | ||
| Sanger sequencing | Point mutations, small insertions or deletions | KRAS mutations in codons G12, G13, G61, G146 | 5-10 unstained slides for extraction of tumor DNA | ≥40% tumor fraction required ∗ | Easy to generate primers for any gene exon of interest | Have to amplify and sequence every exon of interest; labor intensive and expensive. (e.g., activating KIT mutations occur in exons 9, 11, 13, 14, 17, and 18; inactivating mutations in tumor suppressor genes like TP53 can occur in any of numerous exons) | ||
| Genomic methods | Array CGH | Focal gene amplifications | ERBB2 (HER2), EGFR, MYC, CCND1, KRAS, BRAF | 10 unstained slides for extraction of tumor DNA | ≥30% tumor fraction required ∗ | High-resolution copy number data | No data for mutations or rearrangements | |
| Focal gene deletions | APC, PTEN, RB1, TP53, CDKN2A | |||||||
| Large-scale chromosomal gains and losses | Monosomy, trisomy | |||||||
| Next-generation sequencing | Point mutations, small insertions or deletions | KRAS, NRAS, BRAF, PIK3CA, KIT, PDGFRA, CTNNB1 | 5-10 unstained slides for extraction of tumor DNA or tumor RNA | Sensitivity for mutation detection is high, but sensitivity for copy number changes and fusion detection usually requires ≥30% tumor fraction ∗ | Can detect all types of alterations in many genes in a single assay | Requires resources for bioinformatic data processing and storage, 1- to 2-week turnaround time | ||
| Large insertions/deletions | CTNNB1 exon 3 deletion | |||||||
| Gene rearrangements/fusions | EWSR1 rearrangement | |||||||
| Microsatellite instability | Microsatellite instability | |||||||
| Tumor mutation burden (TMB) | Hypermutation | |||||||
| Focal gene amplifications | ERBB2 (HER2) | |||||||
| Focal gene deletions | APC, PTEN, RB1, CDKN2A | |||||||
| Large-scale chromosomal gains and losses | Monosomy, trisomy | |||||||
| DNA methylation profiling (by array or NGS of bisulfite-converted DNA) | Epigenetic subgroups | CIMP-high, CIMP-low, non-CIMP subtypes | 5-10 unstained slides for extraction of tumor DNA | >40% tumor fraction required ∗ | Outperforms conventional histologic-based methods for tumor classification and prognostic stratification | Not yet clinically validated or reimbursable for tubal gut neoplasms |
∗ Methods performed on nucleic acids usually require at least 30% to 40% tumor content, and microdissection of unstained FFPE slides is often required to enrich for tumor content before DNA extraction.
Cancer arises from accumulations of genetic alterations in the genome. , Genetic alterations are defined as changes in the DNA sequence and/or DNA content resulting from single nucleotide point mutations; small or large insertions or deletions (indels); copy number changes including large-scale chromosomal gains and losses as well as focal amplifications or deep deletions; and structural rearrangements/translocations. In addition to changes in the DNA sequence/content, epigenetic changes can also occur that modify gene expression or function. One of the most common forms of epigenetic alterations is methylation of CpG islands in the genome, which are enriched in promoter regions and generally lead to decreased gene expression. CpG island methylation cannot be detected with standard DNA sequencing without bisulfite treatment of the DNA. It is thus important to understand what types of genetic alterations can be detected by each molecular method.
Detection of single nucleotide changes along with small insertions and deletions in an unknown nucleic acid sample is the most common assay performed in molecular diagnostics. These assays are performed to identify hereditary germline disease–associated mutations and somatic or acquired mutations in tumor cells. Although sequencing is the “gold standard” method, it was not always the most practical approach before next-generation sequencing (NGS) because of the size of the target gene that must be analyzed, the limited DNA sample that may be available, or the rarity of the variant sequence in the nucleic acid population to be analyzed. Many different approaches to screening for mutations have evolved in the past 20 years in response to improved technologies. The most common methods used today include Sanger sequencing, polymerase chain reaction (PCR), and NGS, each of which is discussed briefly in the following sections with an emphasis on the advantages and limitations of each method.
Chromosomal copy number changes and structural variations are a hallmark of cancer and include abnormal chromosomal number (i.e., trisomies, monosomies, aneuploidy), translocations, focal amplifications, and subchromosomal deletions. Although deletions and abnormalities in chromosome number are among the most common changes, particularly in solid tumors, translocations and focal amplifications have garnered the most interest because of their association with oncogenic activations that may be susceptible to targeted inhibition. The most common methods used in the characterization of chromosomal copy number changes and structural variations include fluorescence in situ hybridization (FISH), comparative genomic hybridization (CGH) array methods, reverse transcriptase PCR (RT-PCR), and NGS.
Clinical tumor samples are most frequently formalin-fixed paraffin-embedded (FFPE) samples, so most molecular methodologies used for tumor samples are optimized for FFPE tissues. Most germline genetic testing, on the other hand, is performed on high-molecular-weight genomic DNA or RNA extracted from white blood cells in whole-blood samples. Improved methods use more limited samples, such as blood spots and buccal smears. A thorough discussion of all methods is beyond the scope of this chapter, so we will focus on testing of surgical pathology samples and other samples that may harbor neoplastic cells, including cytopathology samples and cell-free DNA that may be used for molecular screening and diagnosis.
Immunohistochemical staining on FFPE sections is a routine method in all surgical pathology practices, and there are an increasing number of antibodies that can help detect genetic alterations. For example, there are numerous antibodies against tumor suppressor proteins that are commonly lost in cancer as a result of deletion, truncating mutations, or promoter methylation. Also available are antibodies against proteins that are overexpressed in tumor samples as a result of amplification or translocation; antibodies against oncoproteins that aberrantly localize to the nucleus based on genetic alterations; antibodies against proteins that serve as surrogate markers of defining genetic alterations in tumors; and most recently, mutant-specific antibodies that recognize hotspot mutations in oncoproteins. Examples relevant to GI neoplasms are provided in Table 23.1 . Advantages of immunohistochemistry include rapid turnaround time, minimal tissue requirement (single 5-micron section per stain), and in situ visualization of the results, which allows for accurate interpretation in samples with low tumor content. The major limitation is that only a small fraction of clinically relevant mutations currently have a mutant-specific antibody available, and it is unlikely that there will ever be antibodies available for all clinically relevant molecular alterations.
FISH and chromogenic in situ hybridization (CISH) are widely used methods that can be applied to detection of DNA and RNA variants. Metaphase FISH is a cytogenetic technique that requires culture of live cells, and this allows detection of much smaller abnormalities than are detected by conventional karyotyping. Interphase FISH does not require culture of live cells, and it is therefore a practical method that is commonly used to study routinely fixed tumors.
For interphase FISH analyses, DNA probes in the 60- to 200-kb range are covalently attached to a fluorescent molecule, hybridized to a complementary target sequence in cellular DNA, and visualized under a fluorescent microscope as a point of fluorescent light in the nucleus of the cell. Probes are designed with specificity to any region of interest within the genome and are widely available for centromeric regions (i.e., CEN probes) and telomeres. Multiple probes may be hybridized simultaneously and analyzed separately by using different colors of fluorescent dyes.
Known, recurrent oncogenic translocations are commonly detected by FISH by using dual-fusion probes or break-apart probes. Dual-fusion probes contain two probes, each labeled with a different fluorescent dye and designed to bind regions spanning the breakpoint of each translocation partner. In the absence of a translocation, two distinct nuclear signals are observed for each colored probe. In the presence of a translocation, there is a single distinct signal for each color from the nontranslocated chromosomes, and the other two signals then combine, or fuse, together both colors for the translocation. Dual-color, break-apart probes are particularly useful in detecting translocations in which one gene can recombine with multiple partners, like EWSR1 . This approach consists of two probes that bind to the intact gene flanking the breakpoint. In the setting of a translocation, the two probes break apart from each other and yield two distinct signals rather than a single hybrid signal.
Copy number aberrations are also well suited for detection by FISH. Centromeric probes give an accurate count of chromosome number and are useful in the detection of aneuploidy. When centromeric probes are used in combination with probes that target specific genes or hotspot chromosomal regions, they also allow a readout of regions of genomic deletion or amplification. Diploid tumor cells have two distinct centromeric probe signals and only one chromosomal arm signal in the setting of a deletion, but more than two in the case of amplification. Multiple cells are typically scored, and a signal ratio is calculated and compared with validated positive and negative control ratios.
Tumor samples are a complex mixture of neoplastic cells, stromal cells, inflammatory cells, and background (normal) tissues. Some carcinomas, like those of the pancreas and biliary tree, are characterized by scattered, small neoplastic glands embedded within abundant desmoplastic stroma. Other cancers may be infiltrated by a dense lymphocytic response. As a result, unenriched tumor samples may vary in neoplastic cellularity from a high of approximately 80% to a low of only 5% to 10% tumor cell fraction. The success of many molecular diagnostic assays depends on a neoplastic cellularity or tumor cell fraction of at least 40%, and microdissection is usually required to enrich the sample for neoplastic cells. Manual microdissection often involves scraping specified regions of unstained FFPE sections under direct guidance of an adjacent and aligned hematoxylin and eosin (H&E)-stained section. These approaches can produce marked improvements in neoplastic cellularity.
Laser microdissection methods may be used to dramatically enrich neoplastic populations, although the yield of tissue is significantly reduced by these labor-intensive methods. Assay requirements must be tailored to the tissue parameters to determine which enrichment methods are needed. In liquid-phase enrichment, cells are digested to release them in a suspension and then purified by bead-tagged antibodies that target cell surface antigens. These approaches are common in research applications, but are used much less frequently in clinical practice.
In addition to tissue samples obtained from sections cut from paraffin blocks, cytopathology samples may also be used in molecular diagnostic assays. The number of cells and quantity of DNA available for testing from cytology preparations have recently been shown to be consistently adequate for a variety of methodologies, including NGS. The use of cytological specimens in molecular assays must be closely supervised by a pathologist who can ensure that an adequate specimen is collected during the biopsy procedure, and because the process may consume the permanent diagnostic record.
Small amounts of detectable cell-free DNA circulate in the plasma and serum of healthy individuals, and in those with a variety of disease states. In patients with cancer, this includes DNA and RNA from tumor cells. Detection of a variety of tumor mutations, microsatellite alterations, methylation abnormalities, and chromosomal alterations has laid the foundation for development of assays for use in cancer screening, diagnosis, and therapeutic monitoring. In a similar manner, DNA from other biofluids (e.g., effusions, fecal samples, biliary aspirations, luminal washings) may be used in molecular diagnostic assays. These technologies are an extremely active area of research and hold promise for the development of a variety of novel assays. One significant obstacle with cell-free DNA is the low fraction of tumor-derived DNA, which means alterations will all have low mutant allele frequencies, and both the sensitivity and specificity of variant detection is markedly decreased. Thus cell-free DNA is a commonly used method of monitoring disease burden, rather than making an initial diagnosis.
Historically, extraction of high-quality DNA and RNA has required fresh or frozen tissue samples. If processed very quickly after surgical removal, these samples provide excellent nucleic acids for subsequent investigations. However, degradation of nucleic acids may occur. Degradation depends on several factors: tissue necrosis, duration of acute surgical ischemia, the time from resection to tissue harvesting, DNase and RNase activity during extraction, and improper storage. Attempts to use formalin-fixed, paraffin-embedded tissue samples create unique challenges and are usually less successful because of DNA fragmentation, DNA cross-linking, and contaminants. However, these samples are much more widely available, and improvements in nucleic acid recovery and subsequent testing have greatly increased the utility of these samples.
Traditional extraction of good-quality high-molecular-weight DNA requires a three-step extraction procedure. First, cell and tissue lysis use detergents, proteinase K, and RNase. Second, proteins are removed, avoiding RNA and chemical contamination. Third, DNA is purified. Conventional manual extraction techniques use phenol-chloroform purification and precipitation by using ethanol or isopropanol. Newer, kit-based approaches use a variety of bead-based elution technologies to purify DNA. Some methods yield DNA of lesser purity and lower molecular weight, although this result is acceptable for many applications. The methods used must appropriately balance ease of use, expense, quality, and downstream assay requirements.
RNA is extracted by two predominant methods: phenol-based extraction (e.g., TRIzol reagent) and silica matrix or glass fiber filter-based binding. TRIzol methods retain small RNAs, including microRNA (miRNA) and small interfering RNA (siRNA). TRIzol reagent also includes guanidine isothiocyanate to maintain the integrity of RNA while disrupting cells and dissolving cell components.
After extraction, nucleic acids must be accurately quantified to assess the success of the extraction and to determine the correct quantity of template for subsequent applications. Quantification is typically performed by using either ultraviolet spectrophotometry or fluorometric quantification with a known control or standard.
Sanger sequencing is currently known as first-generation sequencing. Sanger sequencing was described by Frederick Sanger in the 1970s and is based on electrophoretic separation of randomly terminated linear sequence extensions. Modern day automated Sanger sequencing uses fluorescent chemistry (different fluorescent dyes label the four dideoxynucleotide chain terminators: ddATP, ddCTP, ddGTP, ddTTP) and capillary electrophoresis. It has served as the primary machine for single-gene diagnostics in molecular diagnostics laboratories and as the workhorse for the first generation of the human genome sequencing project that was completed in 2003. Sanger sequencing is accurate, has well-defined chemistry, and is best suited for reading 300-base pair (bp) to 1-kilobase (kb) DNA fragments in a single reaction.
Sanger sequencing has technical limitations, particularly throughput (i.e., number of bases per second that can be read). Electrophoretic separation is the predominant rate-limiting step that severely limits the speed and cost of assays. For example, it has been estimated that one automated sequencer would require several decades and tens of millions of dollars to sequence a single genome today. Another limitation is sensitivity. The lower limit of detection is 20% mutant allele frequency, which means a sample would need to contain at least 40% tumor content to reliably detect a heterozygous mutation.
PCR is a fast and inexpensive technique used to amplify, or copy, small segments of DNA of interest. The amplified PCR products can then be used in numerous molecular and genetic analyses, including modern day Sanger sequencing, DNA fingerprinting or specimen identity analysis, microsatellite instability (MSI) analysis, and melting curve analysis.
For simplicity, sequence variant detection methods may be divided into PCR-based technologies and sequencing technologies. Methodological approaches may be tailored to the range of expected results. For instance, the approaches used to detect a common known sequence variant at a set codon (e.g., BRAF V600E mutation in thyroid cancer) are very different from mutation screens applied to an entire exon, multiple exons, entire genes, or a panel of genes. PCR-based approaches use a variety of different techniques. Common approaches include PCR primers that are designed to amplify specific recurrent mutations and real-time PCR melting curve analysis. However, as sequencing technologies have improved and reactions have become simpler and cheaper to perform and analyze, sequencing approaches have become the first choice for sequence variant detection. PCR is still commonly used for detection of MSI and MLH1 promoter hypermethylation, although MSI is becoming more routinely performed as part of NGS panels.
Methylation-specific PCR starts with bisulfite treatment of the DNA. Methylated DNA is characterized by the conversion of cytosine to 5-methylcytosine, which results in suppression of gene transcription when it occurs in the regulatory promoter region. During bisulfite treatment, unmethylated cytosine residues are deaminated, which converts them to uracil, whereas 5-methyl cytosines are unchanged. Possible methylation of key DNA sequences may then be evaluated by methylation-specific PCR, which uses sets of primers that are complementary to T residues for unmethylated cytosines or C residues for methylated cytosines.
Known, recurrent translocations are readily detectable by RT-PCR or PCR performed on cDNA that is reverse transcribed from purified RNA. Different methods use the same general principles; several primer pairs and sets of primer pairs are designed to detect all possible known breakpoints for a given translocation. Each primer pair consists of a forward primer that flanks the fusion junction on one side and a reverse primer that flanks the fusion junction on the other side. Multiple primers are needed because of the limitation in the size of PCR products and the large genomic variability in known breakpoints for some translocations. This RT-PCR reaction can be performed either quantitatively to measure amplicon production in real time or can be followed by gel electrophoresis of the reaction product to determine whether an amplicon was produced, which indicates that the specific fusion transcript being assayed is present. The RT-PCR product can also be sequenced by Sanger sequencing to confirm and visualize the fusion transcript.
Array-based hybridization is a technology that uses a large number of targets that are densely arrayed on a small, readable substrate, allowing multiple, simultaneous hybridizations. Array targets are immobilized on glass slides or other materials and may consist of DNA, cDNA, PCR products, oligonucleotides, RNA, or proteins. Array-based hybridizations were originally developed on nitrocellulose and nylon membranes and were moved to treated glass slides in 1987. The development of technology to deposit small spots of target on glass substrates led to a rapid increase in the miniaturization of spots and the array density of spots. High-density oligonucleotide arrays with oligonucleotides covering the entire human genome have been developed and are commercially available for research or clinical use including from Affymetrix (CytoScan HD Array and OncoScan FFPE Assay), Illumina (HumanCytoSNP BeadChip and Infinium CytoSNP-850K BeadChip), Agilent (SurePrint G3 Human CGH Array), and others.
CGH arrays are designed to test DNA. Specific genomic DNA sequences are spotted onto an array corresponding to loci known to be amplified or deleted in human tumors or possibly encompassing a much more comprehensive representation of the human genome. Genomic DNA from the test sample is purified, fragmented, fluorescently labeled, and hybridized, typically in a competitive two-color hybridization with a known normal or control sample. To facilitate application to limited tissue samples, several methods have been developed to globally amplify test DNA before CGH analysis. Competitive hybridization allows a readout of the relative genomic copy number across all assayed genomic loci.
Expression arrays are designed to determine the relative expression level of a vast number of genes in a single sample. Typical experiments use labeled mRNA in a competitive, two-color fluorescent hybridization with a known control sample. These tests simultaneously measure the transcript level of thousands of genes compared with a control or normal specimen. This transcriptional profiling (i.e., transcriptome analysis) is commonly applied to human neoplasms in the research setting.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here