Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A primary physiological role of platelets is to support hemostasis at sites of vascular injury by forming a plug that arrests blood loss ( Fig. 124.1 ). Normally, disc-shaped platelets circulate in the bloodstream without adhering to the endothelium of the vessel wall. When the endothelium is damaged, platelets adhere to the exposed subendothelial collagen and, at high shear, to collagen-immobilized von Willebrand factor (VWF). Platelet adhesion at the site of vessel wall damage initiates activation events via intracellular signaling pathways that trigger (1) reorganization of the actin cytoskeleton that results in a shape change from discs to irregular spheres with filopodia, and enables platelet spreading to increase surface contact; (2) secretion of dense granule and α-granule contents, including adenosine 5-diphosphate (ADP) from the dense granules; (3) formation and release of second messengers including thromboxane A 2 (TxA 2 ); and (4) exposure of phosphatidylserine (PS) on the platelet surface, thereby creating a procoagulant activated platelet surface for assembly of coagulation factor complexes that accelerate the generation of thrombin (see Chapter 121, Chapter 125 ). Platelet agonists, including ADP, TxA 2 , and thrombin, bind to their specific membrane receptors, initiating signaling pathways that convert integrin αIIbβ3 from a low-affinity resting state to a high-affinity activated state capable of binding its ligands. Divalent fibrinogen and multivalent VWF function as bridges between αIIbβ3 on adjacent activated platelets, resulting in aggregation and plug formation. This series of platelet responses is essential for the hemostatic function of platelets, and when impaired by congenital or acquired defects, bleeding can occur. However, if these same events take place on a ruptured atherosclerotic plaque, they can lead to the formation of a platelet-rich thrombus that can occlude the arterial lumen and lead to ischemia (see Chapter 121 ).
This chapter addresses the molecular basis of platelet activation and primary hemostatic plug formation. Significant progress has been made in defining the molecular mechanisms that govern platelet responses, facilitated by the study of patients with congenital defects of platelet function and/or number, and by the study of genetically modified animals. The field of platelet biology has been expanding to encompass the roles of platelets in non-hemostatic processes; these are reviewed briefly at the end of this chapter (see section on Platelets Beyond Hemostasis), and some are touched upon throughout the chapter. What we have learned about the molecular mechanisms of platelets in the setting of hemostasis and thrombosis is now being applied in new areas to address new questions.
Platelet plug formation is initiated by contact of circulating platelets with proteins in the subendothelial extracellular matrix (ECM). Normal endothelium maintains an effective barrier that prevents circulating platelets from contact with these ECM proteins (see Chapter 122 ). In addition to the physical barrier, endothelial cells actively inhibit platelet activation by the release of nitric oxide, prostacyclin, and enzymes (CD39/CD73) involved in the metabolism of ADP. At sites of vascular injury, where endothelium is lost or damaged and the ECM becomes exposed to flowing blood, platelets come into close contact with ECM adhesive proteins that promote initial attachment and subsequent activation.
The subendothelial matrix can be viewed as a dynamic and mutable interface that provides multiple substrates to support platelet adhesion ( Table 124.1 ). These substrates include collagens, immobilized VWF, fibronectin, laminin, and thrombospondin-1. Plasma proteins such as fibrinogen, vitronectin, and circulating VWF also interact with platelets after binding to matrix components. The roles of collagen and VWF are well defined, while the contributions of other adhesive proteins to the initial attachment of platelets are less well established. Studies of mice deficient in individual matrix proteins have been useful in determining the contribution of these proteins to the integrated function of the ECM in the formation, growth, and stabilization of the platelet plug.
| Adhesive Protein | Receptor(s) |
|---|---|
| Collagen |
|
| von Willebrand factor |
|
| Fibronectin |
|
| Thrombospondin-1 | αvβ3 |
| Vitronectin |
|
| Laminin | α6β1 |
Shear rates in flowing blood, which vary depending on vessel caliber, influence the contribution of specific matrix proteins. At low shear, platelets can be captured directly by collagens, but at higher shear rates (>1000 s −1 ), VWF becomes critical in ensuring efficient platelet attachment via the receptor glycoprotein (GP)Ibα ( Fig. 124.2A ) (see section on Platelet Adhesion Receptors). VWF, secreted from endothelial cells and recruited from plasma, binds to type VI collagen in the vascular matrix via the VWF A1 domain, and to types I and III collagen in both superficial and deeper layers of the matrix via the VWF A3 domain (see Chapter 133 ).
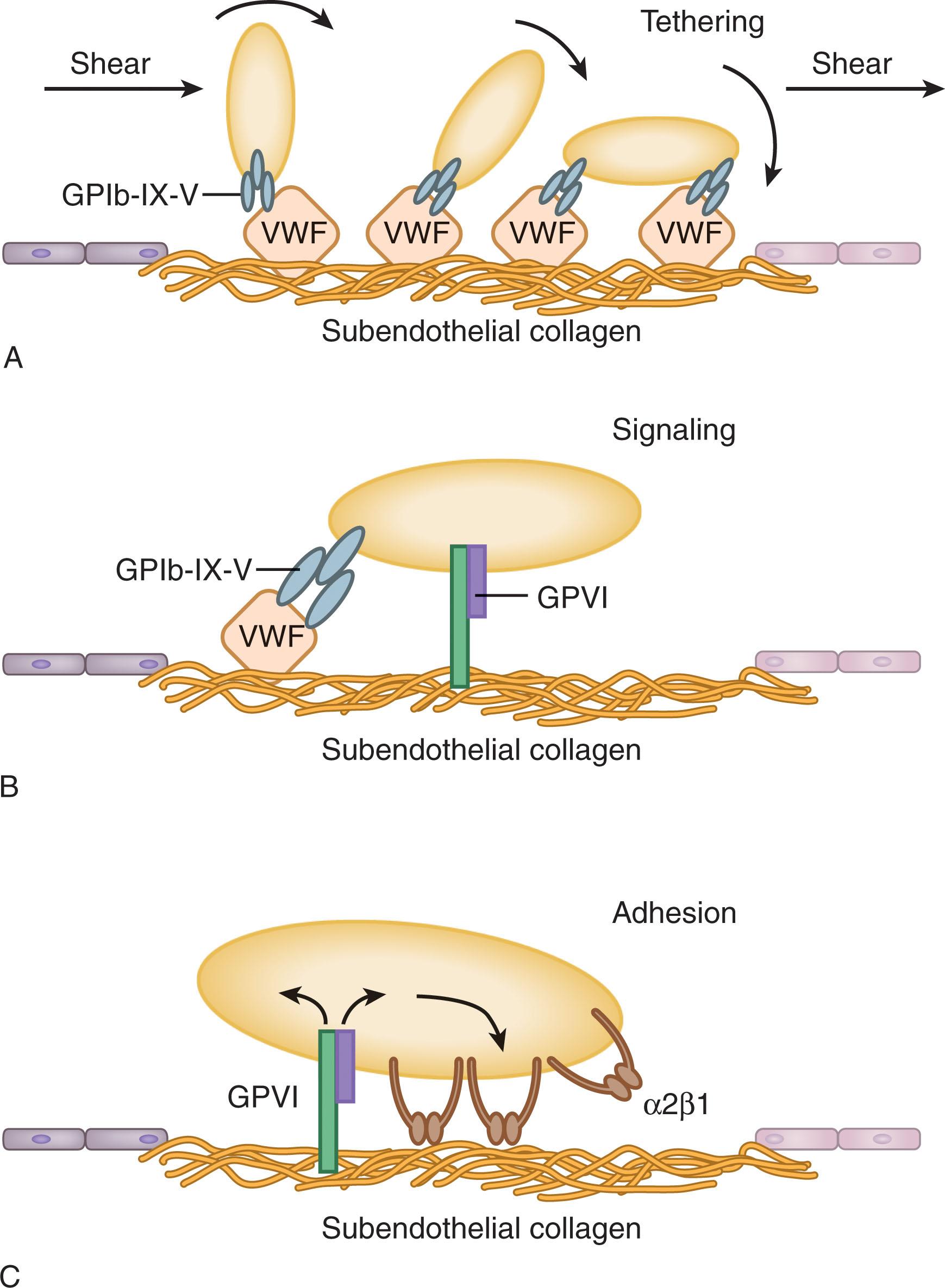
Collagen types I, III, and VI exposed at sites of vascular injury are key substrates for direct platelet adhesion. Collagen is a fibrillar protein made up of tropocollagen monomers packed into units of five to generate microfibrils. Collagens have motifs that are not only recognized by VWF but also by the platelet collagen receptors α2β1 and GPVI (see section on Platelet Adhesion Receptors). At low shear, collagen can function independently of VWF to capture platelets at the matrix surface. However, under high shear, collagen and VWF, with their respective receptors, function in concert.
Platelet adhesion is supported by other substrates in the matrix, and by plasma proteins that interact with the matrix. It is likely that these proteins fine-tune the primary hemostatic response depending on the site or severity of the injury. Plasma proteins including fibronectin, vitronectin, and fibrinogen (and its polymerized product fibrin), matrix protein laminin and platelet α-granule protein thrombospondin-1 support platelet adhesion in experimental systems. It is likely that most of these proteins play an ancillary role in vivo via mechanisms that include enhancing VWF immobilization in the matrix (laminin), protecting large VWF multimers from degradation (thrombospondin-1), or bridging between platelet receptors and matrix collagen (fibronectin).
The individual adhesive proteins serve as ligands for specific receptors on the platelet surface (see Table 124.1 ). Several nomenclature systems have been used to identify the membrane glycoproteins of the platelet, such that the same receptor may have multiple designations. The original and still widely used system designates the membrane glycoproteins according to their electrophoretic mobility upon sodium dodecyl sulfate polyacrylamide gel electrophoresis; protein separation is based on molecular weight, with lower molecular-weight proteins having a greater mobility than those with higher molecular weight. Glycoproteins were designated as GPI, II, III, and so on, with GPI having the highest molecular weight. With greater resolution techniques, additional glycoproteins were identified, hence the subdivision designations, for example, GPIa, GPIb, GPIc; GPIIa, GPIIb. Many of the membrane glycoproteins on the platelet surface exist as noncovalent complexes, for example, GPIa–IIa, GPIb–IX–V, GPIIb–IIIa.
In addition to the GP nomenclature system, the αβ integrin nomenclature system is used. Several of the platelet membrane glycoproteins are members of the integrin family of adhesion receptors (see below), for example, GPIa–IIa is α2β1, GPIIb–IIIa is αIIbβ3. Some glycoproteins also have cluster of differentiation (CD) designations, for example, CD41 for GPIIb and CD61 for GPIIIa. Finally, some receptors have been named based on their function (e.g., the fibrinogen, fibronectin, and vitronectin receptors). Although functional designations can be appropriate from a descriptive standpoint, at least two different membrane glycoproteins on platelets serve as receptors for vitronectin and fibronectin (see Table 124.1 ), and several are receptors for collagen (see below). Beyond creating nomenclature complexity, redundancy of platelet receptors endows the platelet with the capacity to form multiple contacts with a single matrix constituent. Thus, a single ligand may initiate several distinct functional responses by engaging different receptors.
Integrins are members of a superfamily of broadly distributed adhesion receptors that mediate cell-matrix and cell-cell interactions. They are composed of noncovalently associated α and β transmembrane polypeptide subunits with large extracellular domains and short cytoplasmic tails. Of the 18 known α subunits, platelets express five (α2, α5, α6, αIIb, αv), and of the eight known β subunits, platelets express two (β1, β3), with a total of five different platelet integrins. It is estimated that half of the surface area of an activated platelet is occupied by integrin receptors. Many of the glycoprotein receptors on platelets that mediate cell-matrix adhesion are members of the integrin family (see Table 124.1 ). α2β1 is a receptor for subendothelial collagen (see below); α5β1 for fibronectin; α6β1 for laminin; αIIbβ3 for fibrinogen, VWF, and fibronectin; and αvβ3 for vitronectin. Of the integrins expressed on blood cells, αIIbβ3 is the most narrowly distributed and is restricted predominantly to platelets and megakaryocytes. It not only plays a prominent role in platelet aggregation (see section on Molecular Basis of Platelet Aggregation), but in many other platelet responses, including e.g., the association of platelets with tumor cells, an interaction involved in tumor metastasis, and with a variety of microorganisms, interactions involved in infection.
GPIb–IX–V is a notable example of a major cell surface molecule involved in platelet adhesion that is not a member of the integrin family. GPIb is composed of an α (heavy) chain and two β (light) chains; the α and β chains both span the platelet membrane and are linked by disulfide bonds. GPIX and GPV are smaller single-chain transmembrane polypeptides that are noncovalently associated with GPIb, and all three subunits are members of the leucine-rich repeat protein superfamily. GPIb and GPIX are necessary for the expression of the complex on the platelet surface. The GPIbα-GPIbβ–IX–V complex has a stoichiometry of 1:2:1:1 and exists in high copy number on the platelet surface (25,000 to 35,000 molecules per platelet) with the N-terminus of GPIbα being the major ligand-binding subunit of the complex. Platelet activation and aging are associated with the shedding of glycocalicin, a large proteolytic N-terminal fragment of GPIbα that is cleaved by (mostly) ADAM17. The cytoplasmic tail of GPIbα binds to a number of molecules, including 14-3-3ζ and filamin A (that binds to actin filaments in the cytoskeleton) (see section on the Platelet Cytoskeleton) that are important for GPIb-IX-V-mediated signaling.
GPIb–IX–V plays a major role in hemostasis and thrombosis as a receptor for immobilized VWF in the subendothelium. Plasma VWF does not normally interact with platelet GPIb–IX–V, but at the high shear rates that occur in the arterial microcirculation, a conformational change in VWF bound to subendothelial collagen exposes a GPIbα binding site in its A1 domain. Thus, GPIb–IX–V binds to subendothelial VWF; this interaction is reversible with fast on and off rates, which allows for translocation (rolling) of platelets on the surface of the subendothelium (see Fig. 124.2A ). A polymorphism in the GPIbα gene leads to variable numbers of tandem repeats in the macroglycopeptide region (sialomucin “stalk”) of the protein between the ligand-binding region and the transmembrane domain. The length of this region, which is determined by the number of tandem 13-amino acid repeats (one to four), may have a role in regulating platelet adhesion to VWF. With GPIb-IX-V being a major mechanoreceptor on platelets, a pulling force exerted on GPIbα by VWF binding activates a mechanosensory domain close to the transmembrane domain, thereby resulting in intracellular signaling.
In addition to serving as a receptor for VWF in the subendothelium, GPIb–IX–V is also the high-affinity receptor for the soluble agonist thrombin (see section on Soluble Agonist Receptors). Other adhesive ligands for GPIbα include the counter-receptors P-selectin (CD62P), expressed on activated platelets and endothelial cells, and leukocyte integrin Mac-1 (αMβ2), which is involved in the formation of platelet-leukocyte conjugates.
Platelets from patients with Bernard-Soulier syndrome (BSS) lack GPIb–IX–V because of variants in the GP1BA, GP1BB , or GP9 genes that prevent the expression of the complex on the platelet surface. Decreased expression of GPIb–IX–V impairs platelet adhesion to the subendothelium and results in a bleeding diathesis (see section on Molecular Basis of Inherited Platelet Disorders).
Subendothelial collagen has long been recognized as an important initiator of platelet responses, serving as a substrate for platelet adhesion, which ultimately results in platelet aggregation. Three different receptors are involved in platelet responses to collagen: the GPIb–IX–V complex, which binds to collagen via VWF (see above), and GPVI and α2β1 (GPIa–IIa), which directly bind to collagen.
GPVI, with 3000 to 4000 copies per platelet, is a transmembrane protein member of the immunoglobulin superfamily, with two extracellular immunoglobulin domains. Its cytoplasmic domain contains a proline-rich sequence that binds to tyrosine kinases involved in platelet signaling (see section on Activation Pathways). GPVI is noncovalently associated with the Fc receptor γ chain (FcRγ) dimer, which is required for GPVI surface expression and for GPVI signaling via immunoreceptor tyrosine-based activation motifs (ITAMs) in the FcRγ cytoplasmic tails. There is in vitro and in vivo evidence of shedding of GPVI from the surface of activated platelets by the action of ADAM10 and ADAM17. Fibrin has recently been described as an additional ligand for GPVI, adding to the scope of the role of this receptor in platelet adhesion. Deficiencies of GPVI can be associated with a mild bleeding diathesis (see section on Genetic Basis of Inherited Platelet Function Disorders).
α2β1, with approximately 4000 copies per platelet, is the major collagen-binding integrin on the platelet surface. It undergoes a conformational change from a low- to a high-affinity state to allow it to bind to collagen. Silent polymorphisms in the α2 gene control its expression level, with higher plasma membrane levels associated with enhanced adhesion to collagen in vitro and an increased risk of cardiovascular disease.
The adhesion of platelets to collagen is a complex, multistep process. An initial interaction of GPIb–IX–V with VWF in the subendothelium (see above) facilitates a direct, low-affinity interaction of GPVI with collagen (see Fig. 124.2B ). Binding of GPVI to collagen is a potent stimulus to intracellular signaling pathways (see section on Activation Pathways). As a result of this signaling cascade, α2β 1 is activated to bind collagen with high affinity (see Fig. 124.2C ), thereby forming a stable interaction. Alternatively, or in addition, low levels of constitutively activated α2β1 can initiate direct binding of platelets to collagen, thereby assisting GPVI to bind and to initiate activation signaling. At high shear, GPVI plays the major role in mediating stable adhesion, while at lower shear, α2β1 has a more significant role.
CLEC-2 (C-type lectin-like receptor 2) is a transmembrane glycoprotein that was originally described as the receptor responsible for platelet activation by the snake venom rhodocytin, inducing signaling events similar to those initiated by GPVI (see section on Activation Pathways). The major endogenous ligand for CLEC-2 is the transmembrane mucin-like glycoprotein podoplanin, which is expressed on cells outside the vasculature ; the CLEC-2-podoplanin interaction does not appear to contribute to hemostasis and arterial thrombosis, although it is involved in inflammation-driven venous thrombosis. Critically, platelet CLEC-2 interaction with podoplanin on lymphatic endothelial cells regulates blood and lymphatic vascular separation during fetal development (see Chapter 122 ). The CLEC-2-podoplanin interaction on neuro-epithelium is important in blood vessel development in the embryonic brain.
Most agonist receptors on platelets are members of the superfamily of trimeric G protein-coupled receptors (GPCRs) that contain seven transmembrane spanning α-helices, four extracellular loops and domains, and four intracellular loops and domains. Upon binding of their ligands, intracellular signaling is initiated via G proteins (GTP-binding proteins) associated with the GPCRs at the inner plasma membrane, leading to diverse downstream responses (see section on Activation Pathways). The platelet GPCRs include receptors for thrombin, ADP, the arachidonic acid metabolite TxA 2 , and epinephrine ( Table 124.2 ). Deficiencies or dysfunction of these GPCRs can result in bleeding diatheses ranging from mild to severe (see section on Molecular Basis of Inherited Platelet Disorders).
| (A) | ||
|---|---|---|
| Agonist | GPCR | G Protein |
| Thrombin | PAR1 | G q , G i (?), G 12/13 |
| PAR4 | G q , G 12/13 | |
| ADP | P2Y1 | G q |
| P2Y12 | G i | |
| TxA 2 | TP | G q , G 12/13 |
| PGI 2 | IP | G s |
| (B) | ||
|---|---|---|
| G Protein Subunit(s) | Effector | Function |
| Gα q | PLC-β | ↑IP 3 /DAG |
| Gβγ i | PLC-β | ↑IP 3 /DAG |
| PI3K-γ | ↑3-PPIs | |
| Gα 12/13 | p115-RhoGEF | RhoA activation |
| Gα s | Adenylate cyclase | ↑cAMP |
| Gα i | Adenylate cyclase | ↓cAMP |
Thrombin receptors on platelets belong to the protease-activated receptor (PAR) family, GPCRs with a unique activation mechanism that involves cleavage of the N-terminal extracellular domain, thereby creating a new N-terminus that acts as a tethered ligand for the receptor. PAR1 and PAR4 are present on human platelets (PAR3 and PAR4 on mouse platelets); PAR1 is the high-affinity thrombin receptor (approximately 2500 copies per platelet), responding to thrombin at nanomolar concentrations, and PAR4 is a lower affinity receptor. After thrombin cleavage of the N-terminus of PAR1, the tethered ligand (peptide sequence: Ser-Phe-Leu-Leu-Arg-Asn; SFLLRN) undergoes a conformational change and forms an intramolecular complex with a region also on the N-terminal extracellular domain of the receptor, referred to as ligand binding site-1. This triggers the G protein cycle of PAR1’s associated G proteins. PAR4 is nonhomologous with PAR1 in both the peptide sequence of the tethered ligand (Gly-Tyr-Pro-Gly-Lys-Phe; GYPGKF) and its binding characteristics. Although PAR4 requires a higher concentration of thrombin for cleavage, once cleaved, it produces a more sustained signal than PAR1. GPIb–IX–V also possesses a high-affinity binding site for thrombin on GPIbα that facilitates PAR1 cleavage by thrombin.
Platelet PAR1 can be cleaved and activated by proteases other than thrombin, including several members of the membrane metalloproteinase family. These enzymes cleave PAR1 at sites different from the thrombin cleavage site, generating distinct tethered ligands, and distinct patterns of downstream G protein activation.
ADP is an important primary platelet agonist and amplifies other primary responses following its secretion from platelet dense granules. Platelets have two ADP receptors: P2Y1 and P2Y12, which are GPCRs that are coupled to distinct G proteins. ADP binding to P2Y1 (approximately 150 copies per platelet), which is coupled to the α subunits of G q and G 12/13 , mediates a transient rise in intracellular calcium, and induces platelet shape change and rapidly reversible aggregation. ADP binding to P2Y12 (approximately 500 copies per platelet), which is coupled to the α subunit of G i , results in inhibition of adenylyl cyclase, decreased levels of cyclic AMP (cAMP) and enhancement of the aggregation and secretion responses produced by other agonists. The ADP-P2Y12 receptor axis is key to positive feedback signaling that recruits circulating platelets to the primary platelet plug. Full aggregation responses to ADP in vitro require concurrent activation of both receptor pathways.
Adenosine 5’-triphosphate (ATP) is an antagonist of P2Y1 and P2Y12, but an activator of P2X1, a ligand-gated ion channel, that causes rapid influx of Ca 2+ from the external milieu and amplifies responses to other agonists. The effects of ADP and ATP are modulated in vivo by CD39, a nucleoside triphosphate diphosphohydrolase (NTPDase-1) expressed by endothelial and vascular smooth muscle cells that hydrolyzes both ATP and ADP, thereby maintaining homeostasis and preventing inappropriate platelet activation.
In humans, the TxA 2 thromboxane/prostanoid (TP) receptor exists in two isoforms, the result of alternative splicing (TPα and TPβ). TPα is the dominant form expressed on platelets, with approximately 1000 copies per platelet.
Epinephrine is a relatively weak agonist but plays a role in potentiating platelet activation by other agonists, manifested through its ability to inhibit cAMP formation. In humans, the epinephrine receptor is the α 2A -adrenergic receptor (approximately 300 copies per platelet).
Once a subendothelial or soluble agonist binds to its receptor on the platelet surface, intracellular signaling pathways (detailed in Fig. 124.3 ) are set in motion. These signaling pathways result in reorganization of the cytoskeleton and platelet shape change, storage granule exocytosis, TxA 2 synthesis, PS surface exposure, and αIIbβ3 activation.
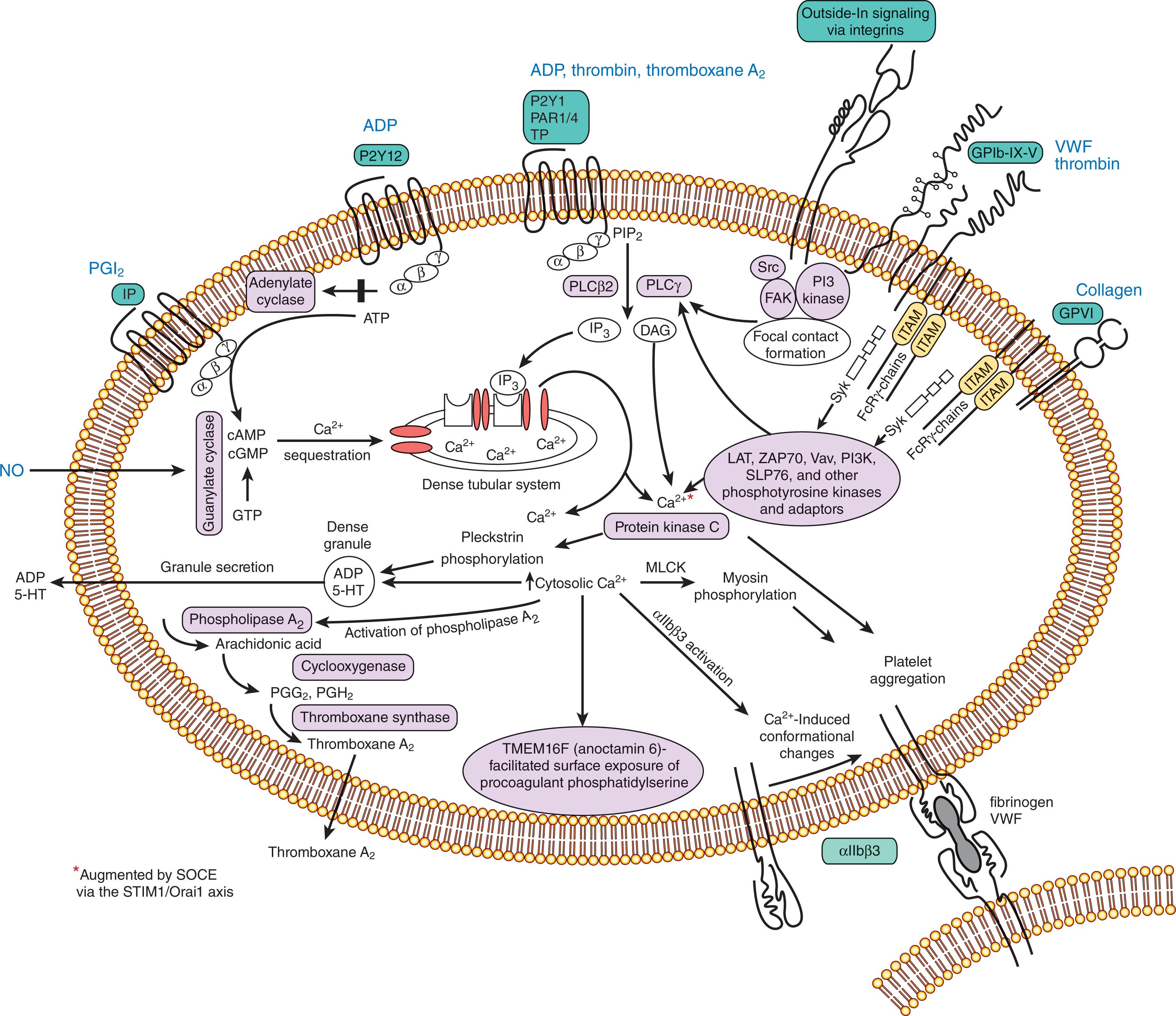
The signaling pathways, initiated by collagen binding to the ITAM-linked receptor GPVI, and by thrombin, ADP, TxA 2 , and epinephrine binding to their specific GPCRs, comprise a “molecular toolkit” of signaling molecules—effectors, second messengers, and signal integrators—which will be considered briefly. Much has been learned about the signaling pathways from genetically modified mice. The reader is referred to comprehensive reviews of platelet signaling for more detail.
The GPCRs for soluble platelet agonists are constitutively associated at the inner plasma membrane with specific heterotrimeric G proteins (consisting of α, β, and γ subunits) of the families G q , G 12/13 , and G i (see Table 124.2A ). The receptor for the potent platelet inhibitory molecule, prostaglandin I 2 (PGI 2 ; prostacyclin) is also a GPCR and is coupled to G s .
In the basal, resting state, guanosine 5’-diphosphate (GDP) is bound to the α subunit of the G protein. Upon ligand binding, a GPCR acts as a guanine nucleotide exchange factor (GEF), promoting exchange of GDP for guanosine 5’-triphosphate (GTP) on different classes of the α subunit. Sites on the α and βγ subunits are thereby exposed, allowing for activation of effector molecules including the β isoform of phospholipase C (PLCβ), the γ isoform of phosphatidylinositol 3-kinase (PI3K), and the small GTPase (see below) Rho-specific GEF, p115-RhoGEF (see Table 124.2B ). Adenylate cyclase is activated via G s and inhibited by G i . Intrinsic GTPase activity of the α subunit, enhanced by GTPase-activating proteins (GAPs), specifically regulator of G-protein signaling (RGS) proteins, hydrolyzes the α subunit-bound GTP to GDP, thus restoring the G protein to its inactive resting conformation.
GPVI is the most potent signaling collagen receptor. As an ITAM-linked receptor, clustering of GPVI upon binding to collagen results in phosphorylation of the constitutively associated FcRγ dimer by tyrosine kinases of the Src family (Fyn and Lyn) that are associated with the cytoplasmic domain of GPVI. Phosphorylation of tandem ITAM motifs enables binding of Syk via Src homology 2 (SH2) domains. Activation of the tyrosine kinase Syk leads to the phosphorylation of the adaptor protein LAT, which serves as the platform for the assembly of a signalosome—a complex of multiple signaling enzymes and adaptor molecules (e.g., SLP-76, Gads, Grb2) within membrane lipid rafts. The signalosome serves as a membrane scaffold for phosphorylation/activation of effectors including phospholipase Cγ (PLCγ) and the β isoform of PI3K.
The platelet receptor platelet-endothelial cell adhesion molecule (PECAM-)1 negatively regulates GPVI signaling via immunoreceptor tyrosine-based inhibitory motif (ITIM) sequences in its cytoplasmic tail by recruiting the tyrosine phosphatase SHP-2 and reducing LAT signalosome assembly.
The signaling pathway initiated by binding of GPIb–IX–V to VWF is similar to that of GPVI in that both involve activation of PLCγ via FcRγ, Fyn and Lyn, and Syk. Binding of platelets to podoplanin via CLEC-2 also induces signaling events like those initiated through GPVI. However, rather than (tandem) ITAM phosphorylation, it involves phosphorylation of smaller hemITAMs in the cytoplasmic tails of dimerized receptors.
Activation of PLC, either the β-isoform (by thrombin, ADP, or TxA 2 via G q ) or the γ-isoform (by collagen, protein tyrosine kinases, and scaffold molecules) results in the hydrolysis of the inner plasma membrane leaflet phospholipid phosphatidylinositol-4,5-bisphosphate (PI-4,5P 2 ). The two second messengers that are the formed, soluble inositol-1,4,5-trisphosphate (IP 3 ) and membrane-associated diacylglycerol (DAG), lead, respectively, to increased cytosolic Ca 2+ concentrations and to activation of a variety of proteins, most notably protein kinase C (PKC), a serine/threonine kinase.
Activation of PI3K isoforms, either γ (via G i ) or β (via the collagen signaling pathway), results in phosphorylation of PI-4,5P 2 to yield PI-3,4,5P 3 . Inner membrane leaflet PIP 3 functions in signaling by interacting with proteins that contain binding motifs termed pleckstrin homology (PH) domains; an example of a major PIP 3 effector is Akt, that is activated to function as a serine/threonine kinase.
PKC is a central protein kinase in the PLC signaling pathway that phosphorylates the serine and threonine residues of many platelet proteins, including pleckstrin. Upon activation by DAG and Ca 2+ , the conventional isoforms, PKCα and PKCβ, play important roles in platelet secretion and platelet spreading on fibrinogen, respectively. The serine/threonine kinase Akt (PKB) regulates platelet secretion and αIIbβ3 activation.
PKA and PKG are described in the section below on Cyclic Nucleotides.
The mitogen-activated PKs (MAPKs) ERK, JNK, and p38 are serine/threonine kinases that are activated following platelet stimulation with physiological agonists and are involved in platelet activation processes.
An increase in the intracellular Ca 2+ concentration ([Ca 2+ ] i ) is a key event that triggers platelet activation and aggregation; Ca 2+ -dependent responses include shape change, secretion, procoagulant surface exposure, TxA 2 formation, and αIIbβ3 activation. The basal [Ca 2+ ] i is maintained at approximately 0.05 μM and can increase to greater than 1 μM with strong stimulation. The initial increase results from IP 3 -mediated release of Ca 2+ from the dense tubular system (DTS) via IP 3 -receptors. Upon depletion of this Ca 2+ pool, store-operated Ca 2+ entry (SOCE) occurs from the platelet exterior. Stromal interaction molecule 1 (STIM1), a protein in the DTS membrane, undergoes a conformational change when DTS Ca 2+ is depleted, allowing it to bind and activate Orai1 (calcium release-activated calcium channel protein 1), the major SOCE Ca 2+ -selective release-activated Ca 2+ (CRAC) channel in the platelet plasma membrane.
An increase in [Ca 2+ ] i is one of the main triggers for activation of cytosolic phospholipase A 2 (cPLA2), resulting in the formation of the proaggregatory prostanoid TxA 2 . cPLA2 hydrolyzes the polyunsaturated fatty acid arachidonic acid from the C2 position of inner plasma membrane leaflet phospholipids, and arachidonic acid is converted to the cyclic endoperoxide intermediates prostaglandin (PG)G 2 and PGH 2 by cyclooxygenase (COX)-1. Thromboxane synthase in the platelet cytosol metabolizes PGH 2 to TxA 2 , which diffuses out of the platelet and is available to activate additional platelets via the TP receptor.
In contrast to the heterotrimeric G proteins associated with GPCRs, platelets also contain small (i.e., low molecular weight) GTPases (belonging to a superfamily of monomeric G proteins) that are critical signaling integrators. Like heterotrimeric G proteins, they are activated by GEFs and inactivated by GAPs. Roles of specific small GTPases of the Rho family, involved in cytoskeletal dynamics, the Ras family, involved in cell adhesion, and the Rab family, involved in membrane trafficking, are described below in the sections Cytoskeletal Reorganization, Molecular Mechanisms of Aggregation and Secretion of Granules, respectively.
PGI 2 and nitric oxide (NO), synthesized by the endothelium, aid in maintaining platelets in a resting state. PGI 2 -mediated activation of adenylate cyclase via G s increases the intracellular level of cAMP. Nitric oxide (NO) diffuses into the cytoplasm and activates soluble guanylate cyclase, generating cGMP. These cyclic nucleotides activate PKA and PKG, respectively. Both serine/threonine kinases phosphorylate multiple substrates including filamin and the small GTPase Rap1. Elevated levels of cAMP and cGMP result in sequestration of intracellular Ca 2+ in the DTS, and inhibition of cytoskeletal rearrangement, granule secretion, and aggregation.
In contrast, lowered levels of cAMP occur due to inhibition of adenylate cyclase via G i ; this is important in facilitating activation of platelets.
Platelet plug formation requires platelets to undergo a rapid change from their resting discoid shape to active forms that spread over the damaged subendothelium and recruit additional platelets by providing an expanded surface area for platelet–platelet or platelet–leukocyte interactions. The discoid shape of the circulating platelet is maintained by an internal cytoskeleton composed of polymers of actin and tubulin and their associated proteins (see also Chapter 123 ). Shape change requires the remodeling of the resting cytoskeleton and the assembly of new cytoskeletal fibers to transform the platelet into its activated configuration.
The resting platelet cytoskeleton maintains cell shape and integrity as the platelet encounters the high shear forces of blood flow in small vessels. The spectrin-based membrane skeleton (similar but not identical to that of erythrocytes) forms a contiguous network with actin filaments to support platelet ultrastructure. Actin is the single most abundant platelet protein (2 million copies per platelet), forming 2000 to 5000 linear actin polymer filaments that are cross-linked to form a rigid cytoplasmic network. Cross-linking proteins include filamin A and B, and α-actinin. The interaction between filamin A/B and the cytoplasmic tail of the VWF receptor GPIbα provides structural stability and the major link between the plasma membrane and the actin cytoskeleton. Loss of this linkage in platelets deficient in either GPIbα (BSS) or filamin A results in loss of restraint of the spectrin lattice, swelling of the membrane skeleton, and large fragile platelets that are subject to rapid clearance from the circulation.
Platelets contain a long microtubule wound 8 to 12 times into a coil that sits just beneath the plasma membrane, maintaining the discoid shape of the resting platelet. Microtubules are rigid polymers made up of αβ-tubulin heterodimeric subunits. β1-tubulin deficient mice have platelets that are spherical and fail to develop a discoid shape due to aberrant microtubule assembly. A heterozygous human variant in β1-tubulin, which may be present in as many as 10% of the general population, results in decreased levels of β1-tubulin and a subset of spherocytic platelets.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here