Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The mapping of the human genome, and more recently the unraveling of human cancer–specific genomes, has led to more detailed understanding of carcinogenesis, cancer growth, progression, and metastasis. With this understanding, new treatment paradigms for cancer have been developed, generating novel agents that have been successfully introduced into the clinic.
Like normal tissues, tumor tissue exploits growth-receptor signal pathways for its maintenance and progression. Disruption of critical pathways can lead to cancer cell death, translating into clinical response, palliation of cancer-related symptoms, and improvement of overall survival for cancer patients. On the other hand, mutations in the growth receptor signal transduction pathway can lead to “addiction” of the tumor to this pathway, resulting in uncontrolled growth. Effective blockade of the mutated protein or its downstream signaling events leads to inhibition of cancer growth and cancer cell death.
The story behind the development of the first targeted therapy, imatinib, illustrates the course of the paradigm shift now gripping the cancer therapeutic world. Since 1960 we have known about the Philadelphia chromosome’s association with chronic myelogenous leukemia (CML). Yet the translocation between chromosome 9 and 22 was not described until 1973, and over the subsequent years the translocation was linked to the Abelson oncogenic virus and its human counterpart. In the late 1990s Nicholas Lydon and Brian Druker developed imatinib, a compound that blocks BCR-Abl. Because BCR-Abl transcript is constitutively expressed in CML, blocking this path led to remarkable responses in patients with the disease. Imatinib received approval by the U.S. Food and Drug Administration (FDA) for the treatment of CML in 2001, and the paradigm shift in cancer therapeutics took hold.
The implications of this paradigm shift have subsequently led to the identification of many growth-receptor signal transcription kinase–mediated pathways that are either upregulated or mutated and thus targetable for drug development. As experience grows with these new targeted agents, we are discovering the importance of crosstalk with other pathways of cancer destruction, including host-mediated factors attributable to the immune system or to stroma. In this chapter we review the areas of targetable therapy related to melanoma.
Melanoma incidence in the U.S. population continues to rise and is associated with a modest increase in mortality rates, primarily in men. Nearly 50% of skin melanomas are diagnosed before the age of 55, thus having a significant impact on a population of individuals in the prime of their working lives. Understanding carcinogenesis, predicting clinical course, and developing new treatments is a high priority as melanoma continues to exasperate biomedical scientists and clinicians, with devastating consequences for patients. When diagnosed in its earliest stages, surgical excision can cure many but not all. Our current knowledge about the risk for primary melanoma to metastasize uses simple tumor characteristics that can be seen by microscopic evaluation and include the depth of invasion from the surface of the skin, whether the tumor is ulcerated, and the number of mitoses in the vertical growth phase. Unfortunately, even shallow primary melanomas with a good prognosis metastasize and cause death, suggesting that the process of invasion into tissue and spread through the blood or lymphatic systems is much more complex.
Melanoma is a tumor that arises from melanocytes, the pigment-producing cells of the body ( Figure 42-1 ). Melanocytes arise from the neural crest and primarily populate the skin and eye, although they can be found in various other organs. The overwhelming majority of melanomas arise from the skin and more rarely the uveal tract of the eye. Cutaneous melanocytes are located at the junction between the epidermis and dermis, at the base of the rete ridges. Melanocytes are dendritic-type cells that communicate and provide pigmentation (melanin) to keratinocytes of the skin. They increase pigmentation production in response to UV exposure. Interestingly, melanin pigmentation migrates to the UV-exposed side of the nucleus, providing shielding to DNA-damaging UV light.
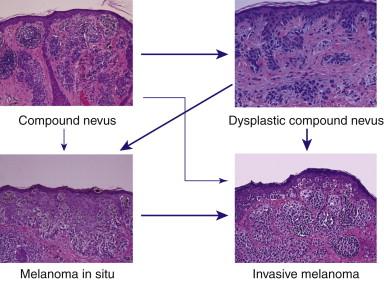
Melanocytes will transform into nevus cells that are able to form theques or nests at the junction of the skin layers (see Figure 42-1 ). These pigmented lesions are called junctional nevi and are flat, homogeneous, brown or tan macules that are well defined. Nevic cells have the ability to invade or migrate into the dermis, forming a macular-papular lesion or compound nevus or a dermal nevus if all the nests are in the dermis. Dermal nevi tend to lose their pigmentation, frequently presenting as a flesh-colored papule. Nevi are acquired lesions and slowly change over time. Newborn infants rarely have nevi, and older individuals, although they have numerous pigmented skin lesions, also have few true nevi. A variation of nevi termed atypical nevi or dysplastic nevi has been recognized and has a different growth pattern, variable amounts of cytological atypia, and a host response identified by lamellar fibroplasia, neovascularization, and lymphocytic infiltration. The number of nevi and atypical nevi are known to be individual risk factors for the development of melanomas. Pathologic series can identify a preexisting nevus in up to 50% of melanomas, suggesting that a precursor lesion exists.
Melanoma typically appears on the sun-exposed areas of the skin, and the amount of sunlight exposure over life is a risk factor. Melanomas arising in sun-damaged skin differ in their molecular pathway expression compared to melanomas from non–sun-damaged skin.
Cutaneous melanomas appear in four major distinct clinical and histologic variants: nodular, superficial spreading, lentigo maligna, and acral lentiginous melanomas. Although molecular pathways may differ between these variants, the risk for metastasis remains linked to the depth of invasion into the skin. Superficial spreading melanoma (SSM) is the most common form of the disease and is typically present for years on the skin. It has the hallmark of the classic ABCDE characteristics popularly known as a symmetry, irregular b orders, variegated c olor, larger d iameter (greater than 6 mm), and e volving over time. SSM has radial growth and nodular or vertical growth. Nodular melanoma has a vertical growth phase without any evidence of horizontal growth. Nodular melanomas usually appear rapidly and invade the dermis quickly. Acral lentiginous melanoma is seen on the palms, soles, and nail beds and is the most frequent melanoma in dark-skinned people. Lentigo maligna melanoma is the invasive form of lentigo maligna (LM), which is a melanoma in situ arising in sun-damaged skin. LMs are typically noted on the skin for many years.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here