Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Coffin and Siris reported three patients with this disorder in 1970. Coffin-Siris syndrome (CSS) and Nicolaides Baraitser syndrome are the most recognizable BAFopathies. The causal genes affecting chromatin remodeling also cause less-specific phenotypes of nonsyndromic intellectual disability.
Growth. Prenatal onset of mild-to-moderate growth deficiency, delayed bone age.
Performance. Moderate-to-severe intellectual disability, severe speech impairment, central hypotonia, seizures, tics, autistic features.
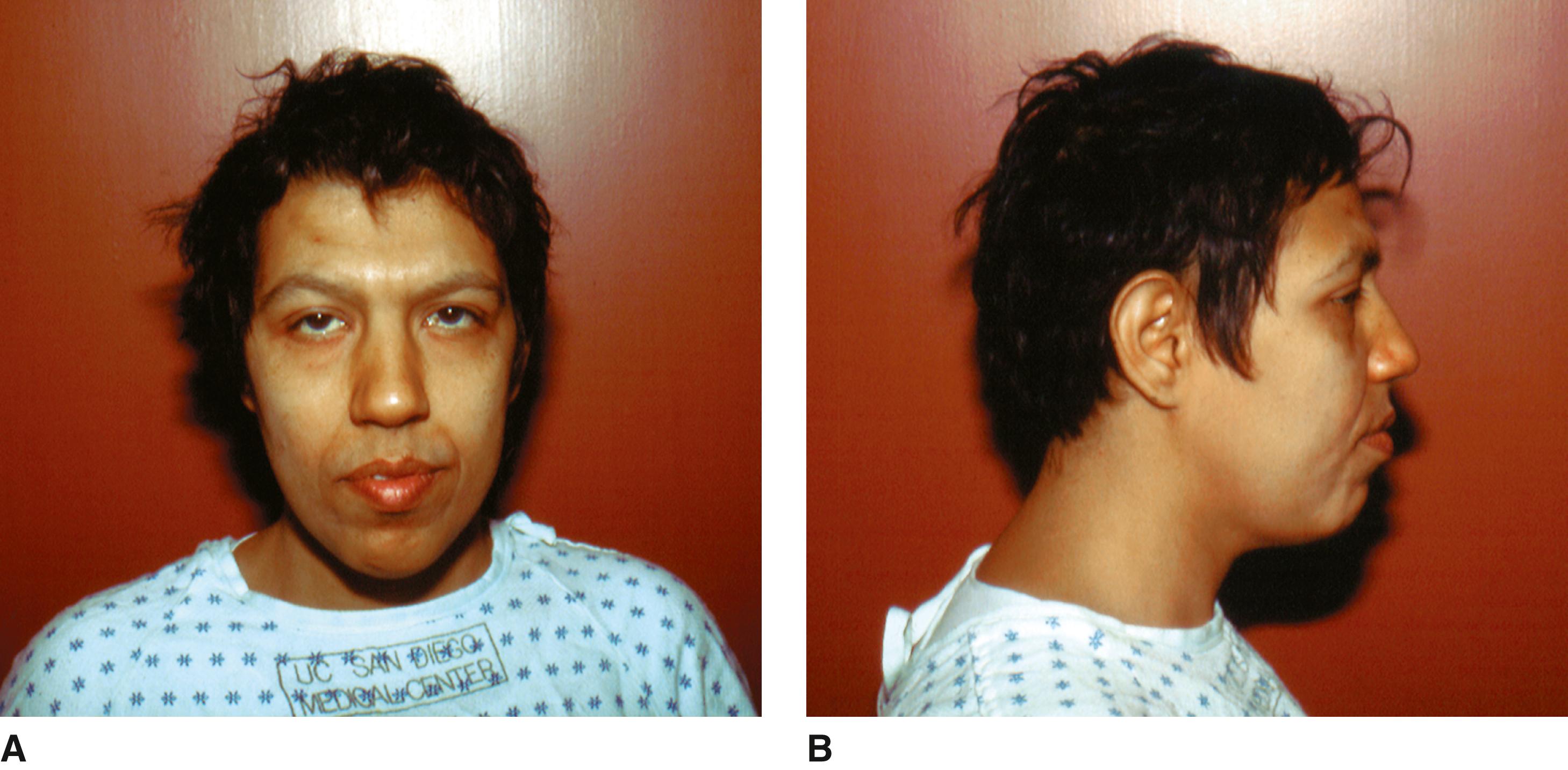
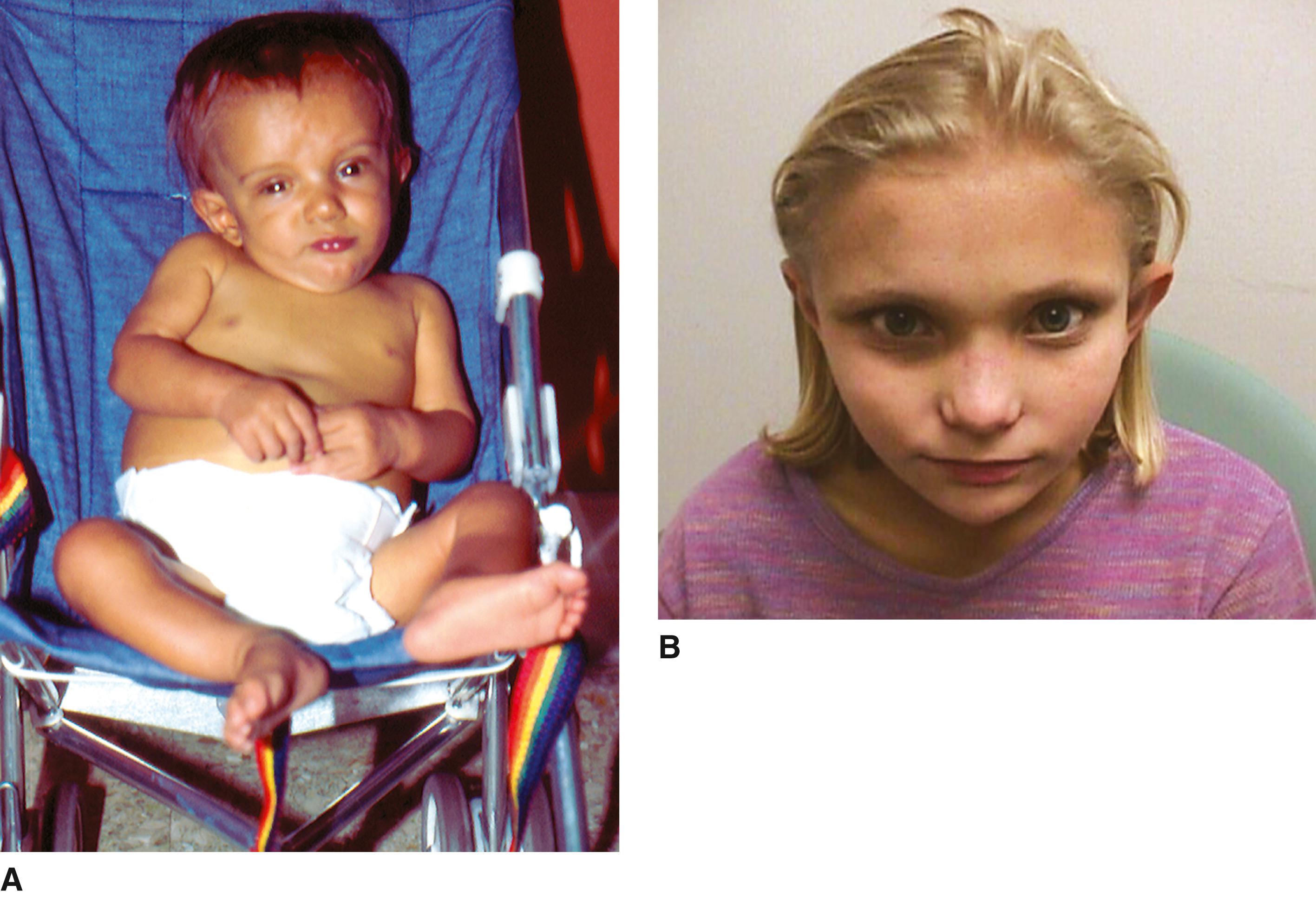
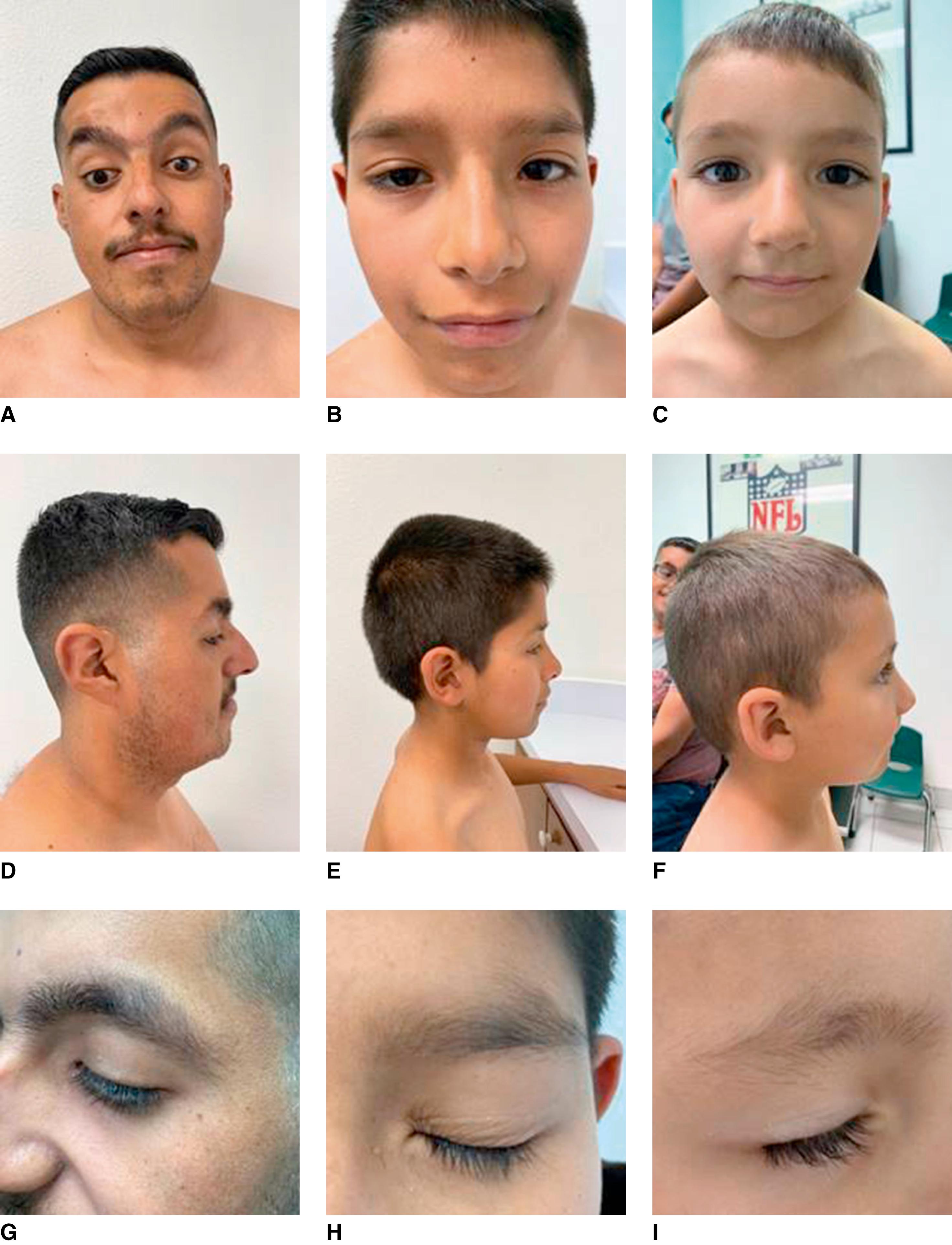
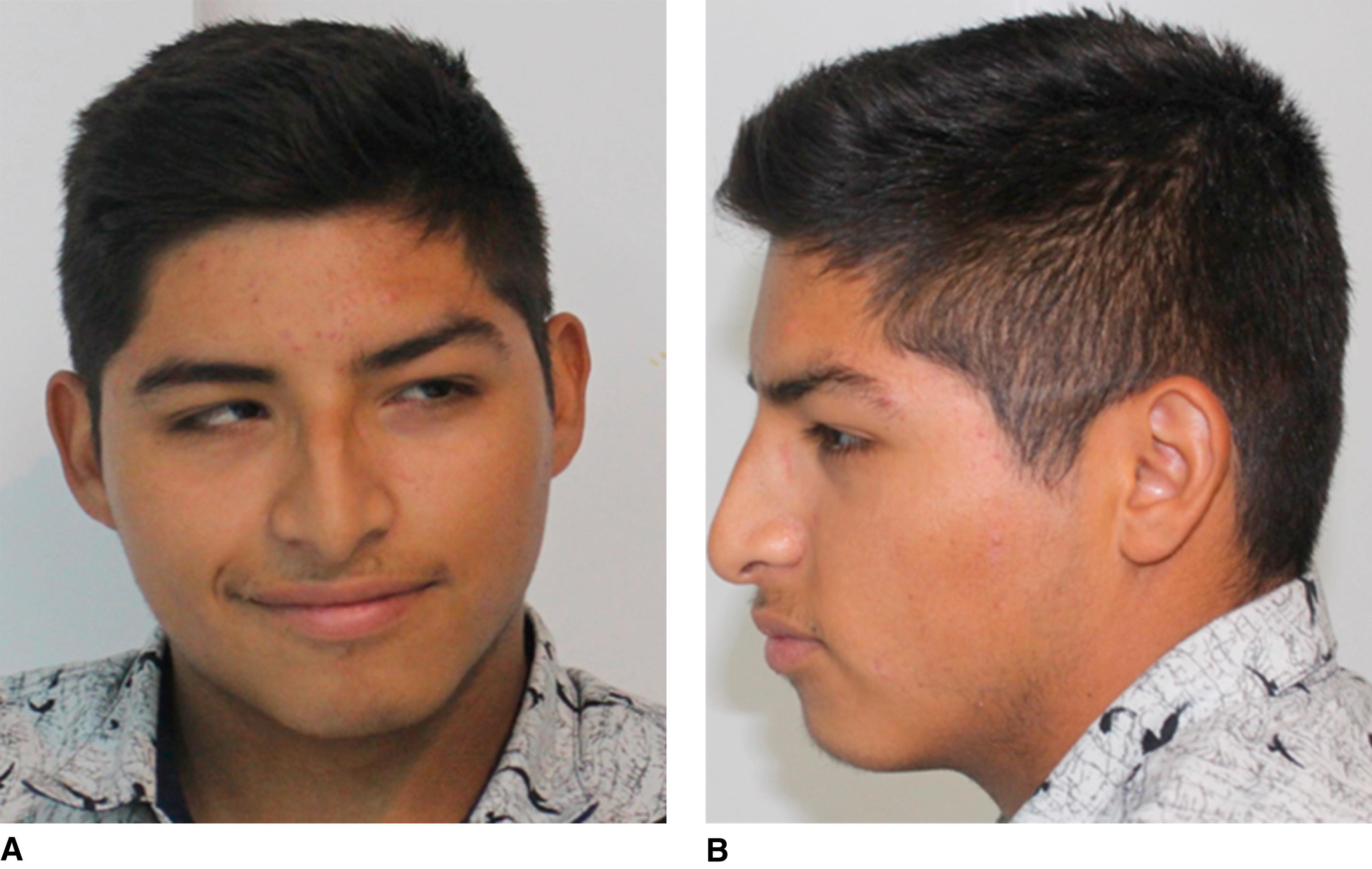
Craniofacial. Mild microcephaly, coarse facies, a wide mouth with full everted lips, flat broad nasal bridge, broad nasal tip, anteverted nares, long philtrum, abnormal ears, bushy eyebrows, long eyelashes, periorbital fullness, ptosis, high palate.
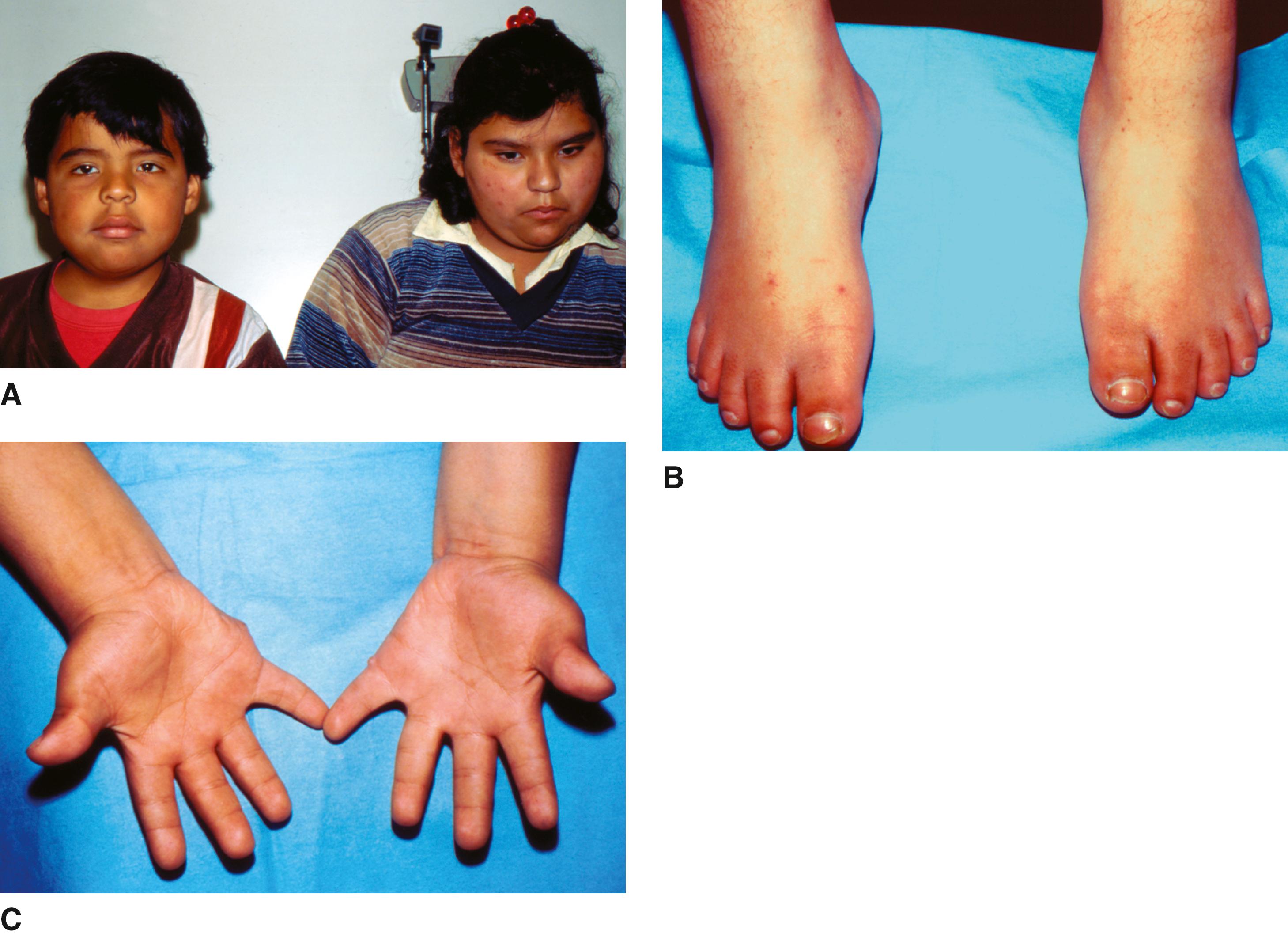
Limbs. Hypoplastic to absent fifth fingers and fifth fingernails and toenails, with lesser hypoplasia in other digits; hypoplasia or absence of terminal phalanges (particularly of the fifth digit); lax joints with radial dislocation at elbow; coxa valga; small patellae.
Hair. Hypertrichosis with a tendency to have sparse scalp hair, low posterior hairline.
Other. Visual problems, including myopia and strabismus; hearing loss; abnormal/delayed dentition; congenital heart defects (patent ductus arteriosus, ventricular septal defect, atrial septal defect, tetralogy of Fallot, patent foramen ovale with aberrant pulmonary vein); renal and genitourinary anomalies (e.g., cryptorchidism, horseshoe kidney, hypospadias); recurrent infections.
Ptosis of eyelids, hypotelorism, absent tear ducts, macroglossia, preauricular skin tag, choanal atresia, cleft palate, hemangioma, cryptorchidism, umbilical or inguinal hernias, short sternum, gastrointestinal anomalies (gastric and duodenal ulcer, neonatal intussusception, intestinal malrotation, gastric outlet obstruction secondary to redundant gastric mucosa), short forearm, vertebral anomalies, kyphosis, scoliosis, joint laxity, diaphragmatic hernia, CNS malformations including Dandy-Walker anomaly of brain, hypoplasia or partial agenesis of corpus callosum, small cerebellum, simplified gyral pattern, and (in one patient) abnormal olivae and arcuate nuclei, and cerebellar heterotopias, hypoglycemia, premature thelarche.
The degree of facial dysmorphism varies, with some patients exhibiting obvious coarseness at birth, and others with only mild facial features. The sparseness of the scalp hair improves with age. Feeding problems leading to failure to thrive and recurrent upper and lower respiratory tract infections are frequent during early life. Both gross motor skills and onset of speech are severely delayed. Autistic features and other behavioral abnormalities are problematic.
Mutations in SMARCB1, SMARCA2, SMARCE1, DPF2, ARID1A , ARID1B, and SOX11 are identified in most but not all individuals with CSS (60% to 90%). New genes causing CSS and CSS-like phenotypes are still being identified.
These genes encode subunits of the BAF chromatin remodeling complex, which acts as an epigenetic modifier by altering chromatin structure. Proper functioning of the BAF complexes plays critical roles in neural development, including the establishment and maintenance of neural fates and functionality.
ARID1B is most common, in 30% to 50 % of diagnosed cases. Individuals with pathogenic ARID1B variants are typically at the milder end of the spectrum of CSS; growth is often normal and the dysmorphic features are more subtle, sometimes with normal fifth fingers and toes.
Deletions and multiple mutations in ARID1B have also been reported in individuals with nonsyndromic intellectual disability, severe speech impairment, autism, and agenesis corpus callosum. All mutations causing CSS identified to date follow an autosomal dominant inheritance pattern.
A few individuals diagnosed with CSS on a clinical basis have been found to have pathogenic variants in SMARCA2 or PHF6 ; on reevaluation the phenotype of these individuals was most consistent with Nicolaides-Baraitser syndrome or Borjeson-Forssman-Lehmann syndrome in its severe female de novo variant, respectively.
Nicolaides-Baraitser syndrome (see Figure 1E ), first described in 1993, includes sparse hair; facial features similar to those seen in CSS short stature; microcephaly; brachydactyly; broadened interphalangeal joint and distal phalanges, owing to decreased subcutaneous fat;, epilepsy; and intellectual disability with marked language impairment, but no nail hypoplasia. Mutations in SMARCA2 have been found in more than 80% of patients with Nicolaides-Baraitser syndrome. This condition has marked phenotypic similarities to the Coffin-Siris syndrome, and common episignatures have been identified for both BAFopathies. Mutations in ARID2 also cause intellectual disability with similarities to CSS.

In 1961, Börjeson and colleagues described an entity of X-linked intellectual disability, epilepsy, hypogonadism, obesity, and dysmorphic facies seen in three related males and three of their less-severely affected female relatives. BFL is a chromatin remodeling disorder with abnormal brain development and severely impaired function.
Growth. Height usually less than 50th percentile, rarely below the 3rd percentile. Moderate obesity, beginning in adolescence, may decrease in later life,
Performance. Moderate-to-severe intellectual disability, with an IQ of 10 to 40, but milder cases have been reported; central hypotonia; markedly abnormal electroencephalograph, with very poor alpha rhythms; seizures may be present.
Craniofacial. Head circumference is usually normal, but macrocephaly or microcephaly can occur. Coarse facies with prominent supraorbital ridges and deep-set eyes, large (7.5 to 9 cm) but normally formed ears.
Eyes. Nystagmus, ptosis, and poor vision, with a variety of retinal or optic nerve abnormalities.
Genitalia. Small penis, with small and soft or undescended testes, and delayed secondary sexual characteristics; hypogonadism appears to be hypogonadotropic.
Skeletal. Thick calvarium, small cervical spinal canal, mild scoliosis, kyphosis, Scheuermann-like vertebral changes, metaphyseal widening of the long bones and hands, hypoplastic distal and middle phalanges, thin cortices.
Other. Central nervous system (CNS) anomalies owing to a primary abnormality of neuronal migration, soft and fleshy hands with tapering fingers, broad feet with short and/or flexed toes, gynecomastia/lipomastia, panhypopituitarism.
These patients are hypotonic from birth, with severe developmental delay. Walking may begin as late as 4 to 6 years and remains awkward. Speech is limited to a few phrases at most. Behavior is usually friendly, but can be challenging and aggressive. The characteristic facial appearance becomes apparent in late childhood, concomitant with the onset of obesity. There is no known unusual susceptibility to health problems, although bronchopneumonia was responsible for the demise of two of the original patients at the ages of 20 and 44 years. Life span is presumed to be normal. A sheltered environment is necessary because of severe limitations of neurodevelopmental performance.
This disorder has an X-linked recessive inheritance pattern. Mutations of plant homeodomain (PHD)-like finger gene ( PHF6 ) located at Xq26-27 are responsible. The protein in chromatin remodeling plays a role in the regulation of transcription. PHD zinc fingers interact with chromatin or mediate protein-protein interactions, and recognize specific histone modifications. PHF6 physically associates with the PAF1 transcriptional elongation complex and thereby drives neuronal migration in the cerebral cortex.
Heterozygote females fall into a spectrum of those without any observable features to those with the abnormalities of growth and craniofacial, ocular, and skeletal features characteristic of this syndrome. Performance ranges from mild to moderate intellectual disability (IQ 56 to 70) to above-average intelligence in heterozygous females. The degree of skewing of X-inactivation is not correlated with the severity of the phenotype. Missense mutations allowing for residual protein function cause the classic familial form of X-linked recessive BFLS in males and mildly affected females.
De novo defects in PHF6 in females, presumably lethal in males, result in a recognizable phenotype with ID of variable severity, a characteristic facial gestalt (bitemporal narrowing, prominent supraorbital ridges, synophrys, a short nose), hypoplastic nails, sparse hair, brachydactyly, clinodactyly mainly of the fourth and fifth fingers, dental anomalies, and linear skin hyperpigmentation, with strong overlap with another chromatin disorder, Coffin-Siris syndrome (CSS). These mutations or deletions have a severe effect and appear to lead to complete loss of protein function.
Initially described by Alagille and colleagues in 1969, this disorder was more completely delineated in 1973 by Watson and Miller, who reported five families with 21 affected individuals. Two studies by Emerick and colleagues in 1999 and Subramaniam and colleagues in 2011 have delineated the frequency of findings and natural history of the disorder in large groups of patients.
Growth. Mild growth deficiency in more than 50%.
Performance. Developmental delays (16%); intellectual disability is rare.
Craniofacial. Typical facies (95%) consisting of deep-set eyes; broad forehead; long, straight nose with flattened tip; prominent pointed chin; small, low-set or malformed ears.
Eyes. Posterior embryotoxon (abnormal prominence of the Schwalbe line, the line formed by the junction of the Descemet membrane with the uvea at the anterior chamber angle causing the margin of the cornea to be opaque) in 88%; Axenfeld anomaly (iris strands).
Cardiac. Right-sided defects or pulmonary circulation defects; 67% have peripheral pulmonary artery and/or pulmonary branch stenosis, with or without associated complex cardiovascular abnormalities, particularly tetralogy of Fallot.
Skeletal. Butterfly-like vertebral arch defects (87%); other vertebral defects, including hemivertebrae and spina bifida occulta; rib anomalies.
Hepatic. Paucity of intrahepatic interlobular bile ducts (85%), chronic cholestasis (96%), hypercholesterolemia. Extrahepatic biliary duct involvement (20%), primary hepatocellular cancer.
Renal. Structural abnormalities (39%), including renal dysplasia, small hyperechoic kidney, ureteropelvic obstruction, renal cysts. Functional abnormalities (74%), including renal tubular acidosis, decreased creatinine clearance, increased blood urea nitrogen, histologic abnormalities consisting of mesangiolipidosis.
Vascular. Neurovascular accidents occur in 15%; aneurysms of the basilar, carotid, and middle cerebral arteries; Moyamoya syndrome may be present in a third of patients. Aortic aneurysms, stenosis, and aneurysms of visceral arteries; renovascular anomalies; middle aortic syndrome; hypertension; prenatal ductal stenosis.
Eyes. Retinal degeneration, including chorioretinal involvement and pigmentary clumping; strabismus; ectopic pupils; choroidal folds; anomalous optic disc or vessels; and refractive errors.
Cardiac. Atrial septal defect, ventricular septal defect, patent ductus arteriosus, coarctation of the aorta.
Hands. Short distal phalanges, fifth-finger clinodactyly.
Genitalia. Hypogonadism.
Endocrine. Decreased growth hormone, increased testosterone, hypothyroidism, delayed puberty. Some degree of pancreatic insufficiency (41%).
Other. Cleft palate, shortened ulna, spina bifida occulta, lack of normal increase in interpedicular distance from L1–L5, abnormalities of inner ear structures, clubfeet, craniosynostosis, increased risk of pathologic early fractures (particularly of lower limbs), thyroid cancer, high-pitched voice, hypodontia, palatal and gingival xanthomas, radioulnar synostosis.
Most patients present with neonatal jaundice. Cholestasis, which develops within the first 3 months in 44% and between 4 months and 3 years in the remainder, is manifested by pruritus, acholic stools, xanthomata, or hepatomegaly. Intrahepatic bile duct paucity is often progressive, but may not be evident in newborns. Bile duct diversion, such as Kasai surgeries, can improve cholestasis and prevent progression to cirrhosis and liver failure. Transplantation is required in 15%. Long-term prognosis depends on severity and duration of early cholestasis, severity of cardiovascular defects, liver status as it relates to liver failure or portal hypertension, and occurrence of vascular accidents. Mortality is approximately 10%, with vascular, cardiac, and hepatic causes accounting for most deaths.
This disorder has an autosomal dominant inheritance pattern with highly variable expressivity. Mutations in JAG1 located within chromosome band 20p12 are responsible in 89% of cases. Less than 7% have a deletion of the entire JAG1 gene. More than half are de novo mutations. Less than 1% have mutations in a second gene, NOTCH2 ; no clear phenotypic differences are known to be clearly related to the gene involved. Classic diagnostic criteria combine the presence of bile duct paucity with at least three of five systems affected: liver, heart, skeleton, eye, and dysmorphic facies. However, mutations in JAG1 are found in one-third of patients with very incomplete Alagille syndrome presenting with only one or two clinical features, especially if the heart (2% tetralogy of Fallot, 4% peripheral pulmonic stenosis) or liver is affected. JAG1 encodes for a cell surface protein that is a ligand for the Notch transmembrane receptor. JAG1 and Notch are parts of the Notch signaling pathway, which is critical for the regulation of cell fate decisions.
The variable manifestations of this syndrome were initially described by Bardet and Biedl in the 1920s. This disorder clearly differs from the condition described in 1865 by Laurence and Moon, although it was referred to as the Laurence-Moon-Biedl syndrome in the third edition of this book.
Growth. Early obesity (83%) with the majority below the 50th percentile for height.
Performance. Slow development of expressive speech, poor articulation, delay of motor milestones, mild intellectual disability correlated with visual disability. Ataxia, poor coordination. Psychiatric manifestations, including anxiety, depression, bipolar disorder, obsessive compulsive disorder.
Craniofacial. Macrocephaly, bitemporal narrowing, large ears, short and narrow palpebral fissures, long philtrum, low nasal bridge, short nose, midfacial hypoplasia, and mild retrognathia.
Ocular. Retinal rod-cone dystrophy (100%), myopia (75%), astigmatism (63%), nystagmus (52%), glaucoma (22%), posterior capsular cataracts (44%), mature cataracts or aphakia (30%), typical retinitis pigmentosa (8%).
Limbs. Postaxial polydactyly (58%) of hands, feet, or both, unilateral or bilateral; syndactyly; brachydactyly of hands (50%); broad, short feet.
Kidney. Nephronophthisis, including abnormal calyces (95%), communicating cysts or diverticula (62%), fetal lobulations (95%), diffuse cortical loss (29%), focal scarring (24%).
Genitalia. In males, small penis and testes (88%), hypospadias, chordee, cryptorchidism. In females, partial and complete vaginal atresia; septate vagina; duplex uterus; hydrometrocolpos; vesicovaginal fistula; hypoplastic fallopian tubes, uterus, and ovaries.
Cardiac defects, particularly valvular stenoses and atrial/ventricular septal defects, laterality defects, dental anomalies, unilateral renal agenesis and urologic anomalies, imperforate anus, polycystic ovaries, laryngeal web, esophageal atresia with tracheoesophageal fistula, diabetes mellitus, diabetes insipidus, clinodactyly of the fifth finger, cystic dilatation of the intrahepatic and common bile ducts, hepatic fibrosis, hirsutism, hearing loss, Hirschsprung disease..
The average age at diagnosis is 9 years. Obesity often begins to develop in the first year. The intellectual disability is usually mild to moderate. However, significant behavioral problems occur in 33%, including immaturity, frustration, disinhibition, and poor concentration/hyperactivity. Schizophrenia has been described in some cases. Ataxia, poor coordination, and imbalance are common. The retinal dystrophy is atypical in that the macula is affected early with disc pallor and generally results in problems with night vision already in childhood, constricted visual fields, abnormalities of color vision, and extinguished or minimal rod-and-cone responses on electroretinography. Visual acuity deteriorates with age. Approximately 15% of patients show an atypical retinal pigmentation by 5 to 10 years of age. However, by age 20, 73% of patients are blind. Most patients have mild problems in renal function with partial defects in urine concentration and renal tubular acidosis. Renal malformations or decline in renal function occurs in more than half of the patients. Around 8% of patients go on to develop end-stage renal disease requiring dialysis or transplantation, most often before age 5. Anemia, polyuria, and polydipsia are the most common presenting symptoms of renal involvement.
Insulin resistance and the metabolic syndrome are common; hypertension is present in 60%. The hypogonadism, which is hypogonadotropic, is evident in males with small genitalia. Although only a few males have fathered children, females have often given birth to children. Normal development of secondary sexual characteristics is the rule in women, but vaginal and uterine malformations may be present. Irregular menstrual periods are common. Asthma has occurred in 25% of cases. An increased prevalence of renal malformations and renal cell carcinoma has been described in unaffected relatives of affected individuals.
Mutations in 22 Bardet-Biedl syndrome (BBS) genes have been identified and more are predicted. The known genes account for 80% of cases. Panel testing of all causal genes or whole exome sequencing is an efficient method for molecular testing owing to the high genetic heterogeneity. Bardet-Biedl belongs to the group of the ciliopathies; major structural defects and functional alterations result from ciliary dysfunction during development. The previously held concept that Bardet-Biedl syndrome is a Mendelian recessive disorder may be too simplistic because, in at least some cases (< 10%), two mutations in one BBS gene and a third mutation in another BBS gene are required for manifestation of the clinical phenotype (oligogenic triallelic inheritance). From a practical standpoint, recurrence risk for unaffected parents who have had one affected child is 25%. Prenatal ultrasound presentation manifests with postaxial polydactyly (82%), renal cysts (78%), and other less-common findings.
The gene for BBS6 ( MKKS ), located on chromosome 20p12, encodes chaperonins and is also responsible for McKusick-Kaufman syndrome, a disorder strikingly similar to Bardet-Biedl syndrome with overlapping features, including vaginal atresia, cardiac defects, and postaxial polydactyly, but lacking intellectual disability, obesity, retinal dystrophy, and deterioration of renal function. Significant difficulty exists differentiating between the two disorders in patients prior to 3 to 5 years of age. At that age, obesity, retinal dystrophy, and intellectual disability begin to manifest in Bardet-Biedl syndrome. Mutations in several BBS genes are also responsible for other ciliopathies, such as Meckel-Gruber syndrome, Joubert syndrome, Senior-Loken syndrome, and Leber congenital amaurosis. All of these conditions are considered disorders of ciliary function and are referred to as ciliopathies.
Initially described in a single case by Wiedemann in 1989, the second affected child, a boy, was not reported until 2000 by Steiner and Marques. Approximately 30 cases have subsequently been published.
Performance. Intellectual disability, ranging from mild to severe, with speech delay. Delayed developmental milestones.
Growth. Pre- and postnatal short stature.
Facial. Lateral eyebrow flare; hypertelorism; long eyelashes and thick eyebrows; short, downslanting palpebral fissures; broad nasal tip and bridge; long, smooth philtrum.
Other. Hypertrichosis cubiti (elbow) as well as over the back and legs; small, fleshy hands and feet; fifth finger clinodactyly.
Autism, hyperactivity, aggressive behavior, seizures; Immunodeficiency, preaxial polydactyly, microcephaly; hypoplasia of corpus callosum; strabismus; ptosis; low-set ears; thin vermilion border of upper lip; hypodontia, premature dental eruption, widely spaced teeth; micrognathia; cardiac defects, including patent ductus arteriosus and atrial septal defects; renal defects; congenital hip dislocation; intestinal elongation with malrotation; scoliosis; rib anomalies; 2-3 toes syndactyly; tapering fingers, broad thumbs, high fingertip pads; advanced bone age.
Failure to thrive occurs frequently in the first few years of life. Constipation and feeding difficulties are often a problem. Urinary tract infections are more common than those occurring in the general population.
Wiedemann-Steiner syndrome is caused by heterozygous mutations in KMT2A (lysine [K]–specific methyltransferase 2A, previously called MLL) located at chromosome 11q23.3.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here