Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
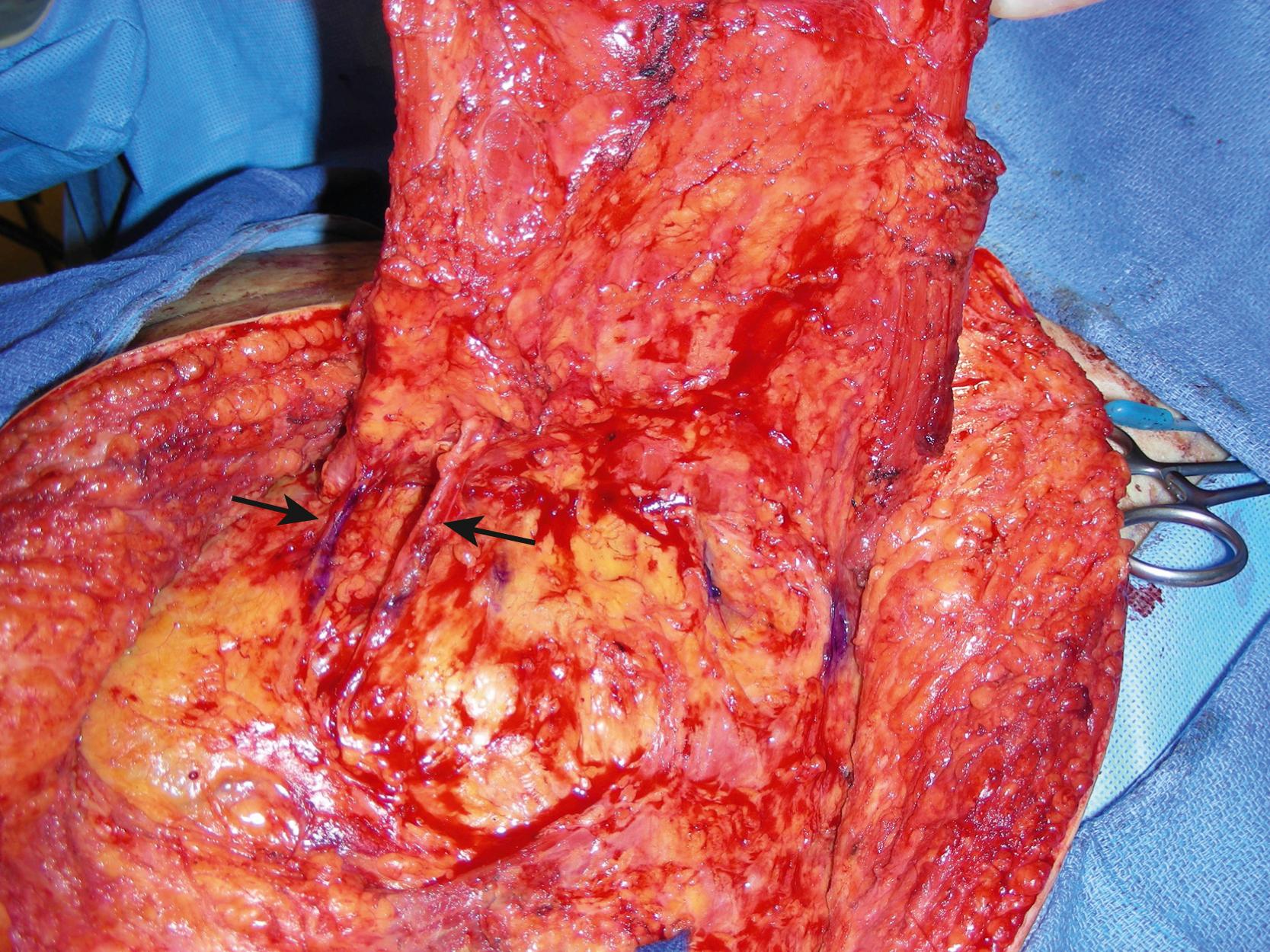
A 45-year-old White female sustained a chronic radiation wound, measuring 10 × 9 cm, over her upper lumbar area with exposed spinal processes ( Fig. 29.1 ). This wound was a complication of radiation to the area for treatment of a soft tissue sarcoma. She was referred by a surgical oncologist from outside hospital to our plastic surgery service for definitive soft tissue reconstruction. This patient also had a longstanding history of smoking. Therefore, her smoking history along with the location of this back wound would make this soft tissue reconstruction difficult and challenging ( Fig. 29.2 ).


There are only a few reconstructive options for such a large soft tissue defect in the middle back after adequate debridement. Although a free flap transfer with recipient vessels based on the superior gluteal vessels can be a valid option, a revised latissimus dorsi muscle flap was considered for this case. The flap, based on two or three large lower thoracic and upper lumber perforators, could be turned over, in a revised fashion, to cover such a large soft tissue defect in this location. Depending on the presence, size, and number of those perforators, the revised latissimus dorsi muscle flap can be used to provide a durable soft tissue coverage for a sizable middle or upper lower back wound.
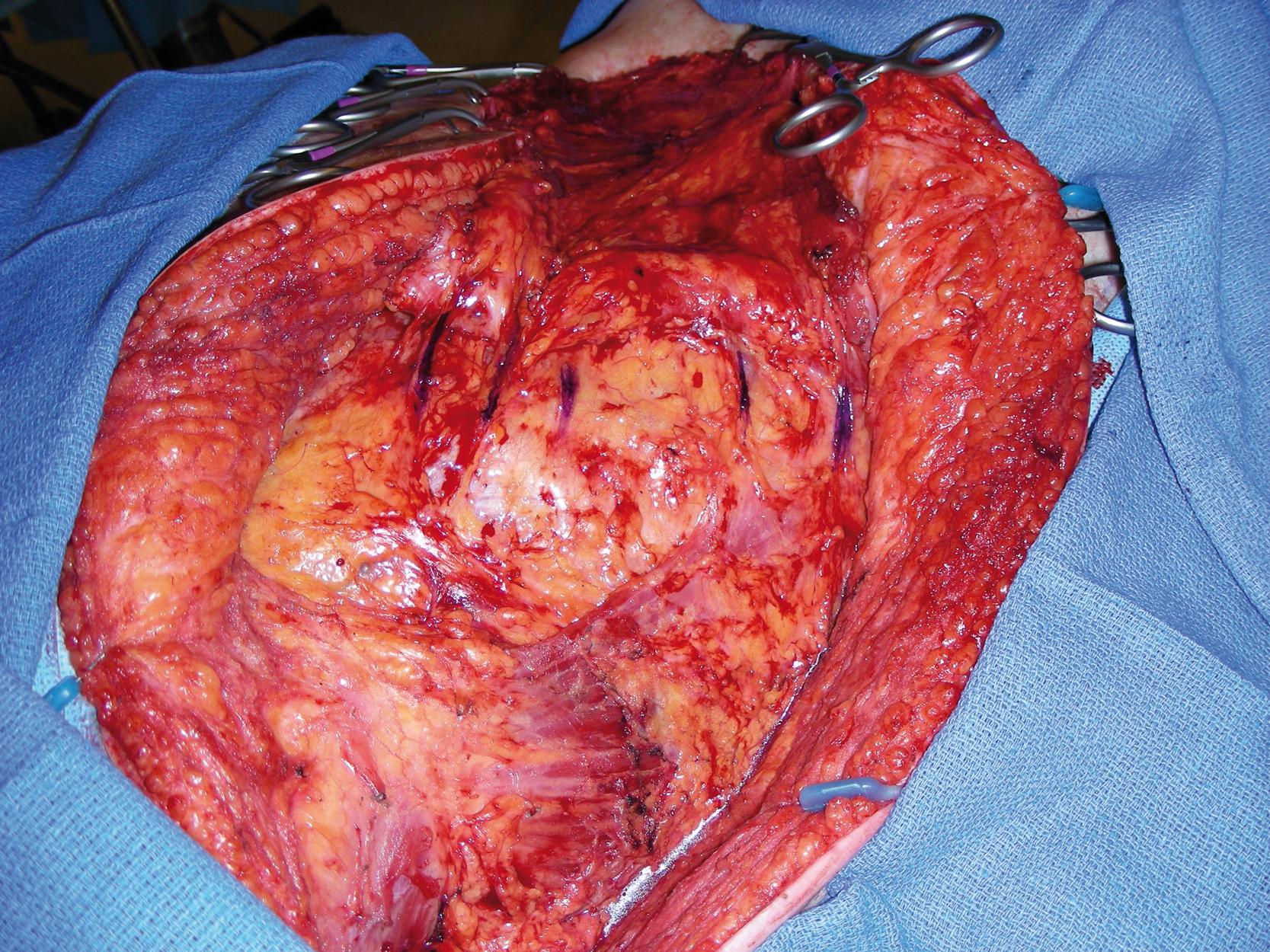
Under general anesthesia with the patient in a prone position, the wound was debrided by the neurosurgery service. The wound was located from T12 to L4 and measured 10 × 9 cm ( Fig. 29.2 ). There were necrotic tissues on the surface with fibrotic tissues along all the edges of the wound. The wound was sharply debrided and all the visible necrotic or colonized tissues were removed. The wound was then irrigated thoroughly with Pulsavac.
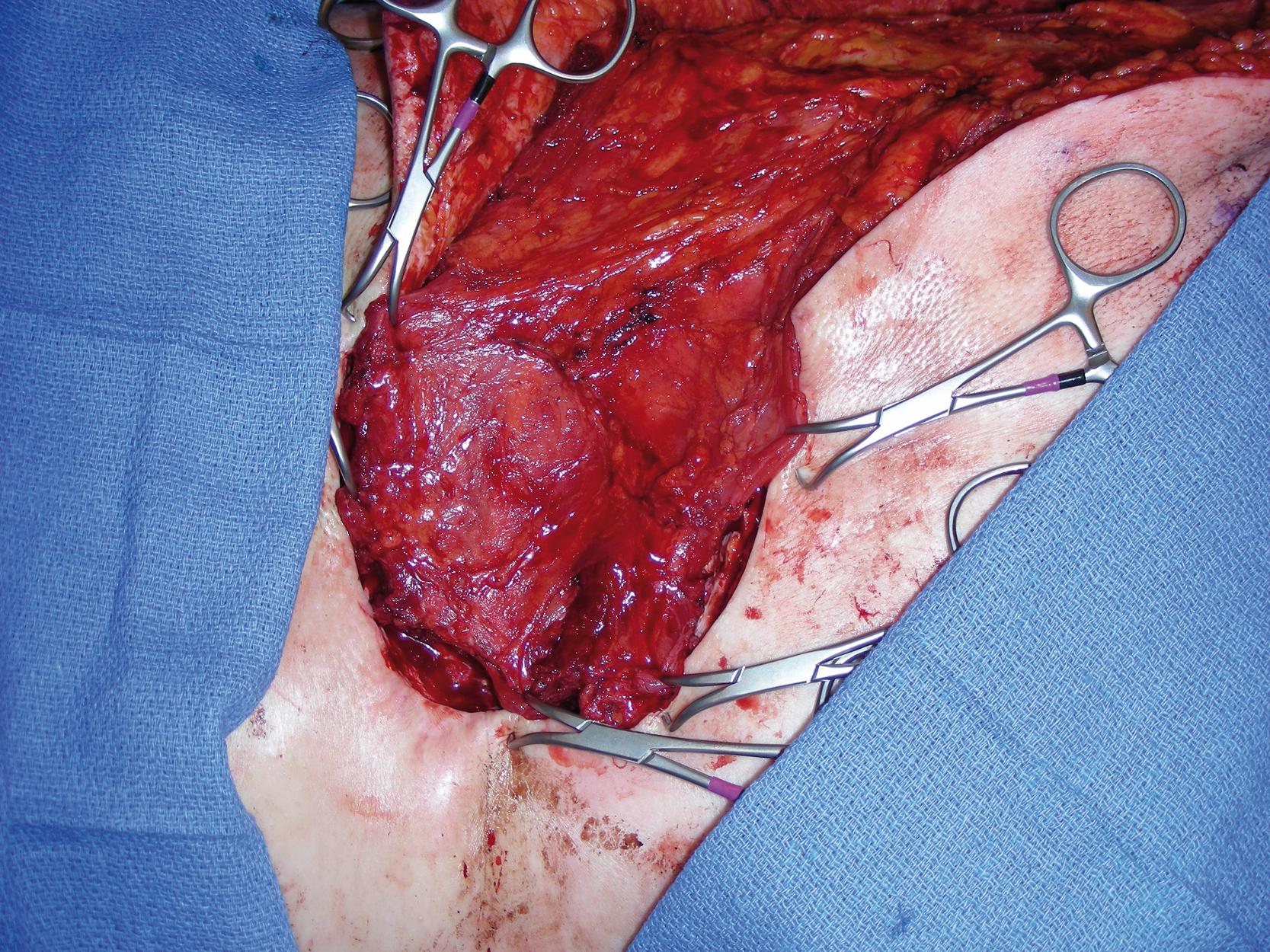
Several major perforators for each side of the latissimus muscle flap were identified by a duplex scan. This flap could be based on the 3–5 major perforators along the same side of the thoracic spine. Two larger perforators were identified on the left side and the left latissimus muscle was selected for the flap reconstruction ( Fig. 29.3 ). An oblique incision was made to explore the pedicle vessels of the left latissimus muscle. The skin flap was raised on either side of the latissimus muscle. Once the medial and the lateral border of the latissimus muscle had been identified, the dissection was performed toward the left axilla. The thoracodorsal vessels were identified and divided with hemoclips. The muscle was divided from its proximal insertion and elevated along with the submuscular tissue plane. By further dissection around those perforators, the latissimus dorsi muscle flap was turned over to cover the wound without too much tension ( Fig. 29.4 ).
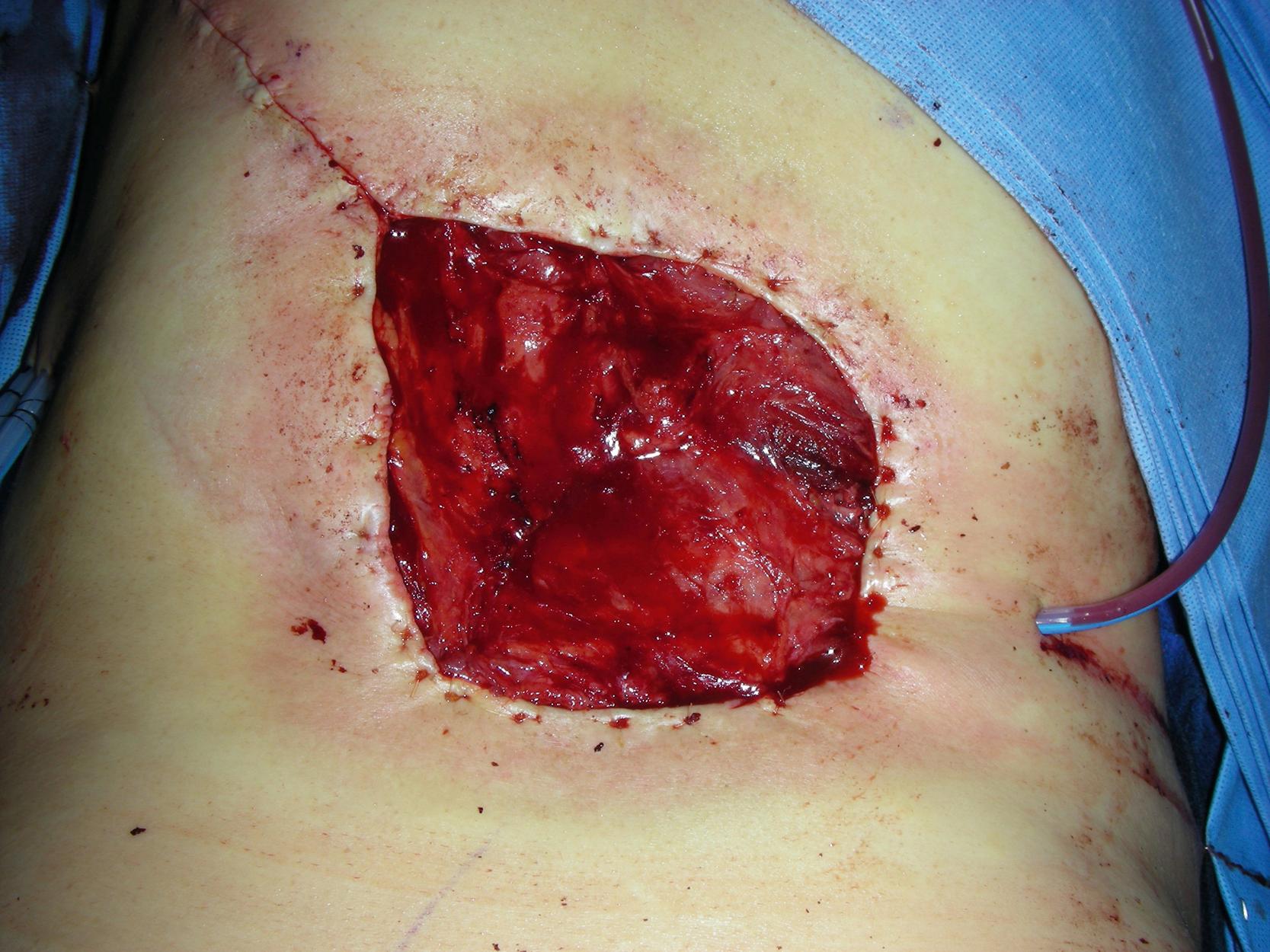
The flap was temporarily inset into the defect and secured temporarily with several small towel clips ( Fig. 29.5 ). At this point, fluorescein (500 mg) was injected intravenously and the fluorescein test was performed to assess the circulation to the flap based on the three perforators but in a turnover fashion. The intraoperative fluorescein test showed that most of the flap appeared to be well perfused. Therefore, the intraoperative decision was made to proceed with the final flap inset and a skin graft to the muscle flap.
The flap was inset into the wound defect. Two drains were placed in the left latissimus dorsi muscle flap donor site. One additional drain was inserted under the muscle flap. The flap was inset into the adjacent rest of the normal-looking skin with several interrupted 3-0 Monocryl sutures in horizontal mattress fashion. The left back latissimus dorsi muscle flap donor site was approximated with several interrupted 2-0 PDS sutures for deep dermal closure and the skin was closed with skin staples ( Fig. 29.6 ).
A split-thickness skin graft was harvested from the left upper thigh with a Zimmer dermatome. The skin graft was meshed to 1:1.5 ratio and placed on the muscle flap and secured with multiple skin staples. Several chromic sutures were used as a quilting suture to secure the skin graft ( Fig. 29.7 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here