Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
All patients with injuries to the spinal column will require appropriate nonoperative management during their care.
The majority of spine fractures can be managed nonoperatively with excellent long-term results.
Those that require surgical treatment must be initially managed with appropriate, meticulous nonoperative techniques.
The integrity of the posterior ligamentous complex can be key to deciding on operative vs. nonoperative care in the adult patient.
Spinal orthoses remain a mainstay for nonoperative management of spinal injuries.
Spinal orthotics can be classified anatomically according to the spinal region restricted. These are cervical orthoses, cervicothoracic orthoses, thoracolumbar sacral orthoses, lumbosacral orthoses, and sacropelvic orthoses. Halo devices may be used to control the cervical spine and cranium with rigid pin-ring fixation.
Spinal braces typically span the point of instability, extending to the adjacent mobile regions to optimally reduce spinal motion.
Complications of bracing include soft tissue irritation or breakdown, inadequate stabilization, and a variety of halo-related complications.
We would like to acknowledge the authors of prior Spine chapters whose work greatly contributed to this version. Those authors include Mark L. Prasarn, Glenn R. Rechtine II, Eric J. Woodard, Robert J. Kowalski, and Nicolas Marcotte.
Optimal management of spinal injuries requires the integration of nonoperative and operative care. Nonoperative management of spinal injuries remains a mainstay of management for most spinal injuries, despite modern advances in surgical techniques. Nonoperative treatment modalities should be employed wherever goals of treatment can be met without exposing the patient to the inherent risks of surgery. When surgery may be required for decompression and stabilization of the spine, bracing or other nonoperative stabilization techniques may be used to temporize physiologically unsuitable patients until they are prepared for surgery. The objectives of nonoperative management of spine injuries are the same as those for operative treatment. These include (1) preservation of neurological function, (2) improvement in neurological deficit if already present, (3) reduction of spinal deformity and maintenance of acceptable alignment, (4) minimization of loss of spinal mobility, and (5) achievement of a healed and stable spinal column. As an ancillary benefit, nonoperative stabilization may provide a degree of pain relief. In most cases of spinal injuries these objectives can be met with nonoperative care.
Nonoperative treatment techniques are employed in all spinal injuries, first and foremost at the initial evaluation and management at the scene of the accident. In most cases, nonsurgical principles are extended as a definitive treatment plan. In addition, during every step of diagnosis and treatment, strict adherence to principles of immobilization must be followed to minimize motion to the injured spine and prevent neurological injury or deterioration. It is important to recognize that bracing can also have adverse effects and to spare its use in cases where it is not required. The purpose of this chapter is to review the use of nonoperative modalities for management of spinal column injuries across the continuum of care, including in acute management, in definitive management, and as an adjuvant to operative care.
According to advanced trauma life support (ATLS) protocols, life-threatening compromise to airway, breathing, and circulation should be promptly addressed. Although the greatest risk for spinal cord injury occurs at the time of high-energy impact, neurological deficits can develop afterwards during treatment. In 1983, Podolsky and colleagues reported that up to 25% of spinal cord injuries had been caused by or aggravated after the patient had come under medical care. Proper immobilization of the injured spine is the key to preventing such catastrophic decline.
The care of spine trauma patients at the scene has dramatically improved over the past several decades. Extrication and transport of trauma patients with immobilization techniques and adherence to ATLS protocols for resuscitation have been credited with this improvement. ATLS protocol mandates that a spine injury be assumed for all injured patients, and that rigid immobilization employed. At the scene, the patient should be immobilized with a cervical collar, head immobilization device, and spine backboard.
The patient should arrive in the emergency department on a backboard with a cervical collar in place. In the face of a global instability, motion can still occur in spite of all attempts at rigid immobilization. The patient should be moved on and off the backboard as few times as possible until the stability of the spine can be adequately assessed. For most injuries, the collar provides an increased level of stability. However, it does not provide complete immobilization and is only effective if well fitted, taking neck length into proportion, and worn properly with the chin secured at the chin rest. With a complete ligamentous disruption, the collar has minimal effect; the person stabilizing the spine plays a much more significant role in restricting motion.
Moving the patient off the backboard for computed tomography (CT) should be coordinated so that imaging of the brain, spine, chest, abdomen, pelvis, sinus, or orbits or any other appropriate study is obtained in one trip to the scanner and one movement off and on the backboard. The risk of decubitus ulceration is directly proportional to the length of time on a backboard—8 hours on a backboard is associated with a 100% likelihood of a decubitus ulcer. The patient should be moved from the board as soon as possible. Appropriate spine immobilization must be continued at all times. Care must be taken not to force the patient into a flattened position, which can cause devastating neurological injury in the presence of a three-column fracture, such as those commonly found in stiff, kyphotic spines. Similarly, patients found in a chin-on-chest position should not be extended to force a collar into place. These patients should instead be immobilized in position with close neurological monitoring.
Contrary to all available evidence suggesting that the log roll is an ineffective and potentially dangerous technique for spine immobilization, it is still almost universally used. In fact, studies conducted before 2004 showed dramatic and unacceptable motion with a log roll. Since that time, many studies have reevaluated this controversial subject. The log roll maneuver has been shown to cause more segmental motion at the level of the unstable, injured segment than any other studied, reasonable method of transfer. Lift and slide techniques are far superior because they create less motion at the injured segment.
Following review of the initial CT scan, other assessments of spinal stability can be performed. In the absence of a facet dislocation and in the presence of significant spine injury, the appropriateness of magnetic resonance imaging (MRI) must be determined. The spinal motion necessary to transfer the patient on and off the MRI table must be kept in mind when deciding the necessity of this imaging modality. Additional transfers of a patient with spinal instability may increase the risk of neurological injury, particularly in hospitals that do not treat a high volume of spine-injured patients. The strongest argument for an MRI is a suspected neurological deficit that is not explained by the injury seen on the CT scan. Other indications for MRI include evaluation of the posterior ligamentous complex, which is important for spinal stability at all levels, and looking for disc herniations or soft tissue compression in patients undergoing closed reduction maneuvers. If a patient is indicated for surgery by an unstable injury identified clinically or by other imaging modalities, it is not necessary to obtain an MRI just to assess the dorsal ligamentous complex.
When a closed reduction of a dislocated segment is needed, it should be performed expediently in the awake and alert patient. Serial neurological examinations are performed during such a reduction maneuver. If the patient is obtunded, or reliable neurological examinations are impossible, then an emergent MRI should be obtained to rule out traumatic disc herniation, which could lead to compression of neurological structures during closed reduction.
Anteroposterior and lateral radiographs of the cervical, thoracic, lumbar, and sacral spine are standard imaging studies obtained in cases of high-energy impact with suspected spinal injury. In patients without evidence of gross instability or neurological compromise on CT or MRI, when performed, upright weightbearing radiographs are an important part of the assessment of spine trauma.
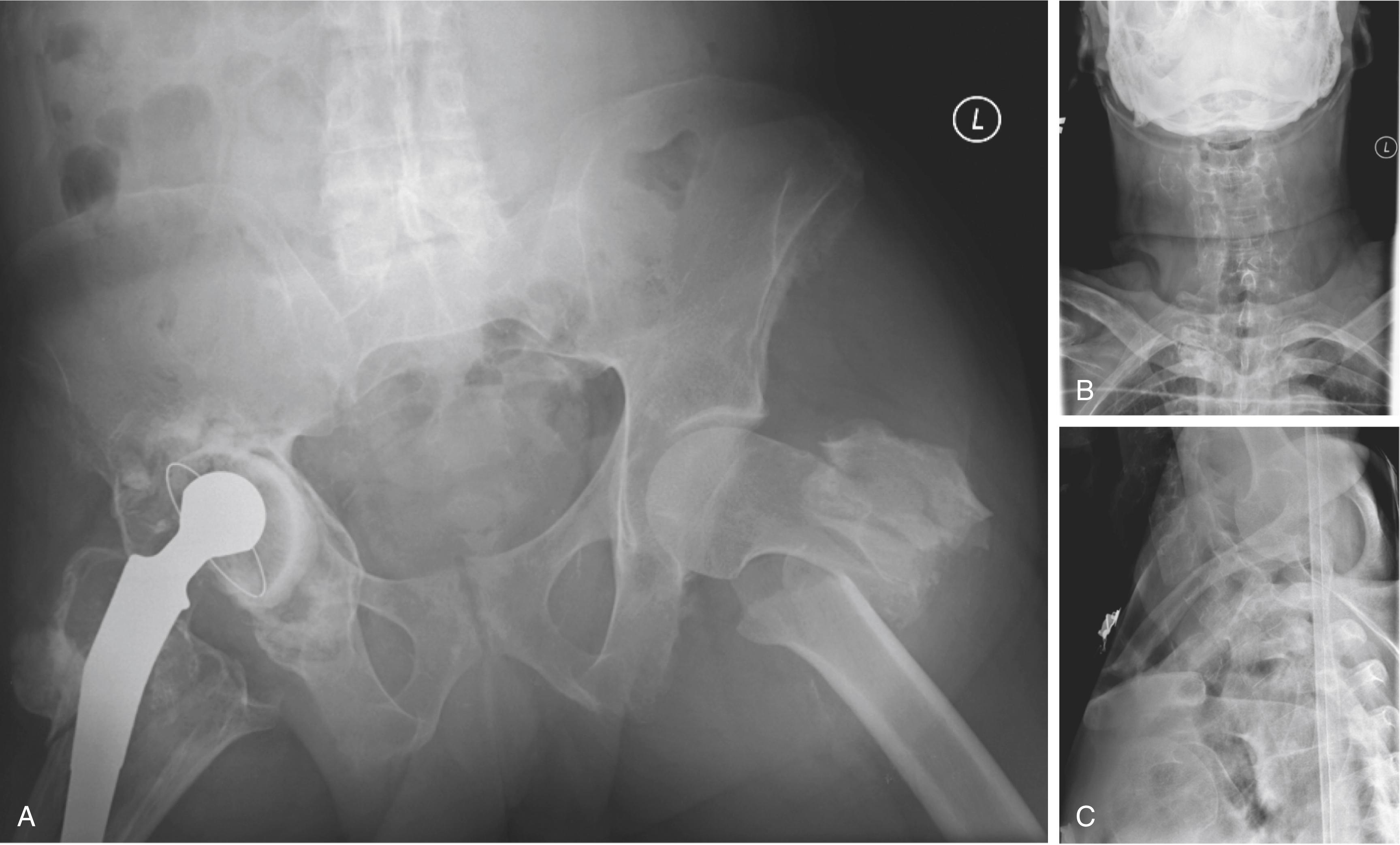
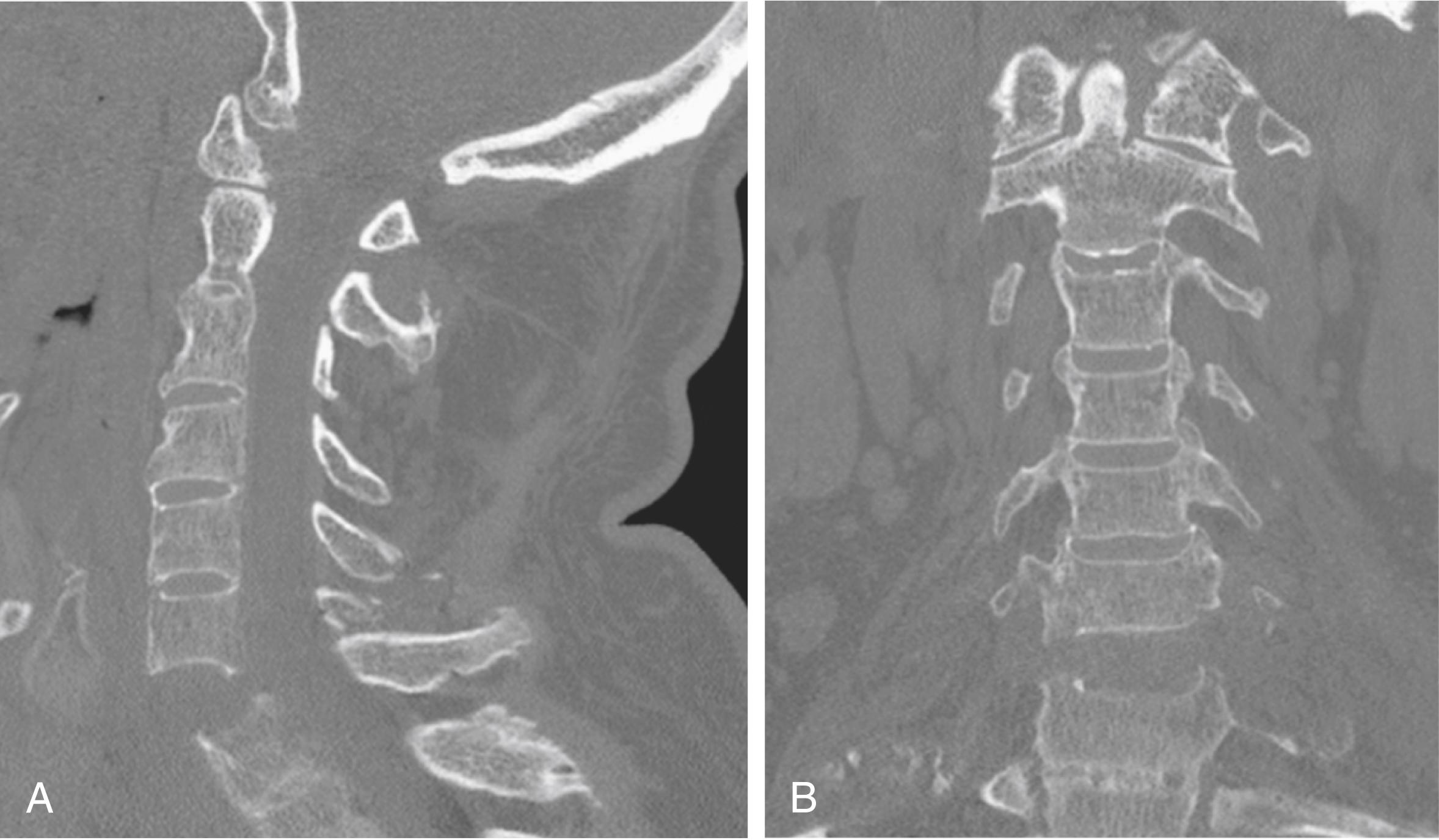
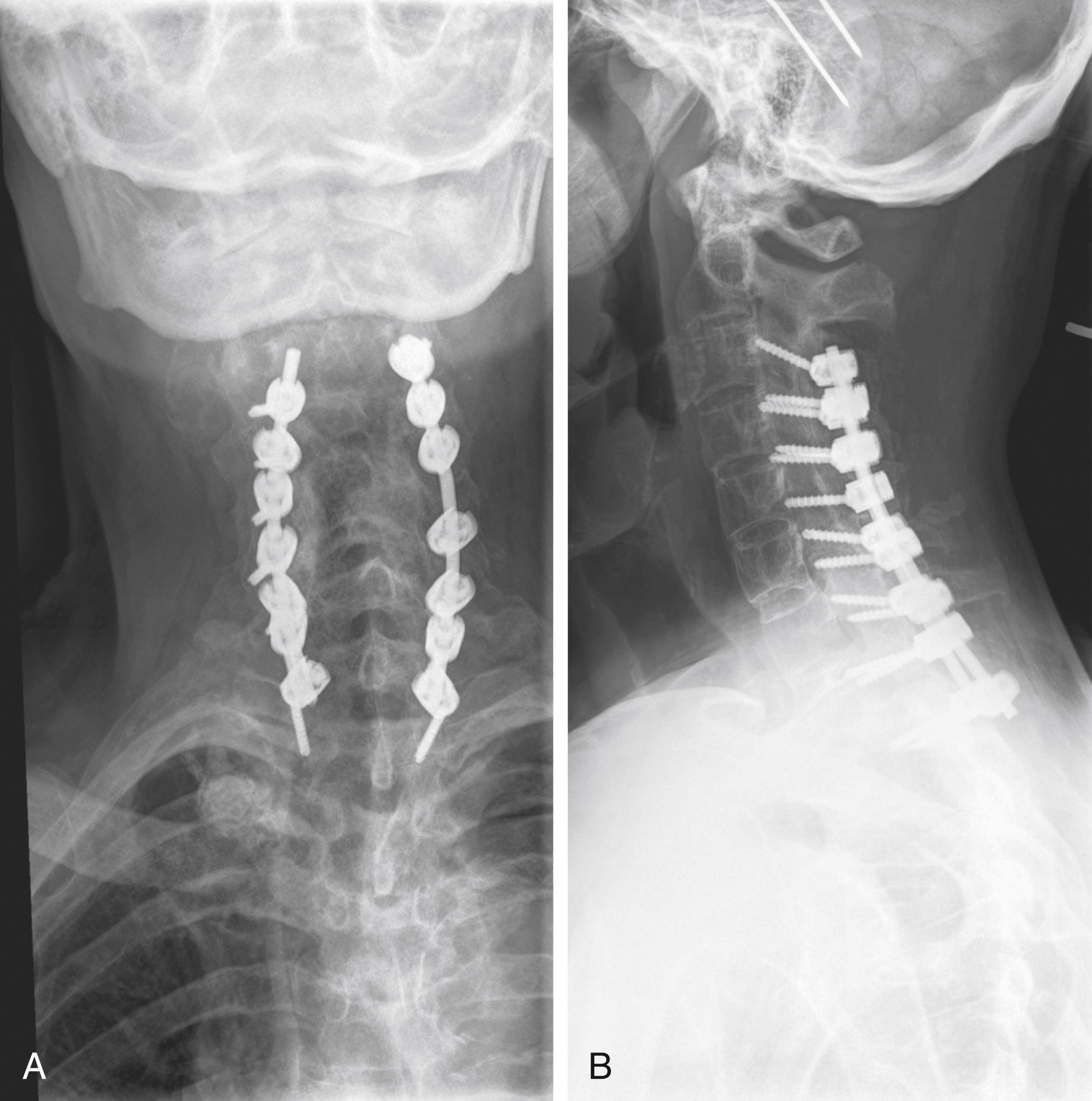
Distracting injuries can often mask symptoms secondary to significant spine injury, and meticulous assessment of the spine must always be performed ( Figs. 164.1 to 164.3 ). It is necessary to image the entire spinal column, owing to a 10% incidence of noncontiguous spinal injuries. Specific injury mechanisms and fracture patterns should prompt the treating team to search for commonly associated nonspinal injuries. Flexion-distraction injuries are highly associated with potentially life-threatening intraabdominal injuries, and patients with transverse process fractures at L5 have a 61% incidence of a pelvic fracture. Falls from a height with resulting burst fractures are often associated with significant lower-extremity fractures, in particular of the tibia and calcaneus.
Closed reduction is a means of reducing cervical spine deformity, indirectly decompressing neural elements, and providing stability. It has been shown to be safe and can dramatically improve neurological status if performed within the first few hours following injury. In animal studies, Carlson and colleagues showed that decompression within 3 hours was associated with better and quicker neurological recovery. A small series of patients with no cord function who received reduction in an emergent manner immediately began to recover. Although this is anecdotal, it is extremely important. The timing question is answered after consideration of the risk-benefit ratio between waiting to obtain a prereduction MRI and proceeding directly with reduction.
Considerable controversy surrounds the order of the reduction and obtaining an MRI in an acute cervical spine dislocation. Eismont et al. reported on a series of six patients with herniated disc material protruding into the spinal canal after subluxation or dislocation of a cervical facet. For the first patient in this series, no myelogram or CT scan was performed, and the patient awoke with complete quadriplegia following dorsal open reduction and internal fixation. Following a myelogram and ventral decompression surgery, the cause was identified as an extruded intervertebral disc. The authors recommended obtaining an MRI in all patients before attempted closed reduction and definitive surgery. Several other cases with neurological deficits after open reduction under general anesthesia have been reported. , In another report by Wimberly et al., a patient developed acute quadriparesis during closed reduction while the patient was awake, which resolved after immediate cervical decompression and fusion surgery.
The group from Thomas Jefferson University advocates performing immediate closed reduction in the patient who is awake and can reliably participate in serial neurological examinations. Vaccaro and associates published their series of 11 patients who underwent successful awake closed reduction without any neurological worsening. In their series, two patients had herniated discs before reduction, and another five had herniated discs following reduction. Darsaut and colleagues attempted to determine the effect of disc herniation during closed reduction in a series of 17 patients who had a cervical dislocation that was reduced under MRI monitoring. They demonstrated that, at least in the research setting, this technique was feasible.
A commonly used algorithm is based on the patient’s neurological status. If the patient is unable to participate reliably in the physical examination, then an MRI is obtained as expediently as possible. The principal disadvantage of obtaining an MRI, in addition to the risks of additional transport and transfer of a spine-injured patient, is the loss of potentially valuable time, which can prolong compression of neurological structures and lead to further permanent deficits. If the patient has minimal or no neurological dysfunction, an MRI should be obtained. If the patient has an American Spinal Injury Association (ASIA) A, B, or C injury and is able to cooperate with the reduction and serial neurological examinations, consideration should be given to an immediate, rapid reduction. In this situation, the MRI would be obtained after reduction. In the setting of a patient who is obtunded or otherwise unable to provide a reliable neurological examination, an MRI should be obtained before attempting any reduction maneuver.
Reduction of a cervical spine dislocation must be performed under image guidance and in a very controlled manner. Gardner–Wells tongs may be applied, with the pins placed 1 cm above the pinna of the ear just below the equator of the head. Pins are tightened to 3.6 kg of pressure. This is indicated once the precalibrated indicator pins protrude a measured amount. If using weights over 25 kg, titanium pins and MRI-compatible tongs are insufficient. Weights of over 60 kg have been used safely for closed reduction of such injuries. In such instances, stainless-steel pins or two sets of tongs must be used. Another option includes the use of a halo that provides four titanium pins to distribute the forces over more pins. The major disadvantage of stainless steel pins is their MRI incompatibility.
It is recommended that the initial applied weight be no more than 4.5 kg. Using more weight can be catastrophic if the patient has an unrecognized instability, such as an occipital cervical dislocation. After applying the initial 4.5 kg, a neurological examination should be performed, followed by a radiograph. Weight should be added incrementally until reduction is obtained. Serial examinations, as well as serial x-rays, are performed to look for any neurological deficit following each addition of weight. After reduction, the weight should be decreased to the minimum needed to maintain the reduction. Routine examinations are continued, as are efforts to stabilize the instability when medically appropriate. Pulmonary and skin issues can be addressed with use of a kinetic treatment table until surgery.
Closed treatment remains the standard of care for most spinal injuries. In a few situations, surgical intervention is clearly required, including skeletal disruption in the presence of a progressive neurological deficit and purely ligamentous injuries in a skeletally mature patient. Such ligamentous injuries require spinal fusion to obtain stability. It should also be noted that the presence of a neurological injury is not an absolute indication for surgery. The remaining gamut of spinal injuries can be treated without surgery. Closed treatment options include bed rest, halo apparatus, external orthosis, or a cast. Many injuries can be treated with an initial period of bed rest in a kinetic treatment bed, followed by bracing and mobilization once some early healing has been achieved. The absence of significant pain should be the clinical indicator of the patient’s readiness to be cleared from the kinetic treatment bed and mobilized. Upright films in the external orthosis should be obtained to confirm that the spinal column is stable at this point.
Debate continues over the appropriate timing of traction or surgery in cases of acute spinal cord injury. It is difficult to demonstrate improvement in neurological function from acute surgical intervention. Patients with complete cord injuries and neurologically intact patients are likely to remain neurologically unchanged with appropriate surgical or nonoperative care. Incomplete lesions typically improve with either surgical or nonsurgical care. Late surgery with decompression of the spinal canal in incomplete cord injuries has been shown to improve neurological function even several years following the traumatic event. , In the acute setting, there has been sparse evidence supporting early surgery, although the Surgical Timing in Acute Spinal Cord Injury Study demonstrated that those undergoing decompression within 24 hours showed a 2.8 times greater likelihood of a two-grade ASIA Impairment Scale improvement as compared to those having late decompression. Surgery for the purpose of spinal canal decompression in a neurologically intact patient is difficult to defend, considering that several series have shown dramatic spinal canal remodeling over time in patients with and without surgery.
Occipitocervical injuries are most often fatal and typically found postmortem. When encountering a patient with such an injury, the treating physician must be vigilant about the diagnosis to ensure the patient’s survival. Initially, such patients should be meticulously immobilized on a backboard with a collar, and the head secured with sandbags and tape. Atlantooccipital disassociation may be stabilized with a halo vest until definitive surgical stabilization is performed. It should be noted that traction for type II injuries (axial distraction) can be catastrophic and is absolutely contraindicated. The injury is treated with dorsal occipital cervical fusion. Some authors advocate adjunctive halo vest immobilization. Occipital condyle fractures and Jefferson or atlas ring fractures are typically managed with an orthosis or a halo.
Management of odontoid fractures depend on location of the injury, and significant controversy remains regarding their management. Many can be treated with a rigid orthosis or halo vest. Type I and type III fractures typically heal uneventfully and have a good prognosis without surgery. Transverse type II fractures through the waist of the odontoid are associated with a high rate of nonunion, and there is much controversy regarding their treatment. A dorsally displaced odontoid fracture is more likely to be treated with surgery. Polin reported on a series of patients treated with a rigid collar as opposed to a halo. More nonunions were associated with the type II fractures. However, there was no statistically significant difference between the types of orthoses used. Chronic odontoid nonunions in the elderly can at times be followed and may not require surgical intervention. In a series of persistent nonunions, no progression of atlantoaxial instability or neurological deficit, or myelopathic symptoms were noted during the follow-up period. Contrary to this result, Kepler and coworkers observed a 17% incidence of new neurological deficits in a similar cohort. Each case must be treated on an individual basis, and decision making should involve the patient and oftentimes the family.
At later reassessment of stability, transverse ligament ruptures can be managed in an orthosis if a bony avulsion occurs. , If successful, this avoids the significant loss of motion following an atlantoaxial arthrodesis. Dickman and associates demonstrated a 100% failure to heal in complete ligamentous disruptions. These injuries often result in a significant incidence of neurological injury, and there is frequent association with other upper cervical injuries. They should be treated with C1‒C2 arthrodesis.
Most other axis injuries can be stabilized with an orthosis or a halo vest. Traumatic spondylolisthesis of the axis most commonly occurs secondary to a hyperextension and axial load mechanism. Neurological deficit rarely occurs, with the exception of the atypical fracture that occurs ventral to the dorsal vertebral body cortex. These atypical fractures may require surgery to prevent neurological decline. Severe hangman fractures with instability through the C2‒C3 disc space require surgery. Most other axis injuries can be managed successfully nonoperatively. , ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here