Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
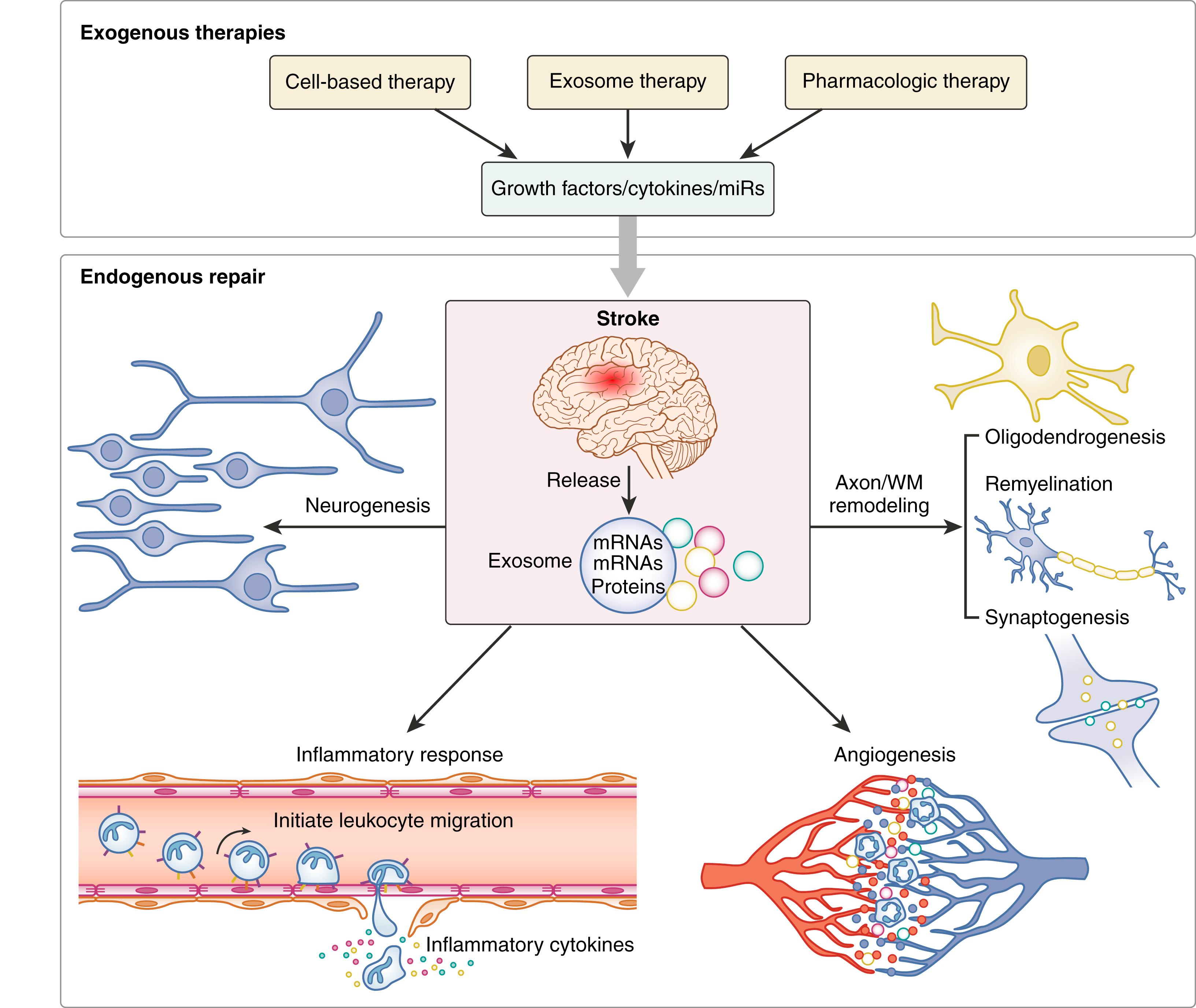
Angiogenesis, neurogenesis, axonal plasticity, oligodendrogenesis, synaptogenesis, and inflammatory response are major interwoven brain repair processes during stroke recovery.
microRNAs play an important role in mediating repair processes.
Exosomes, by transferring select RNAs and proteins, are mediators of intercellular communication, and their generation and molecular cargo are affected by stroke.
Cell-based and pharmacologically based therapies can amplify brain repair processes and lead to improvement of neurologic function after stroke.
New therapies, such as cell reprogramming, modification and targeting of cellular microRNAs, or engineering of exosomes to deliver enriched exosomal content of microRNAs, have potential for promoting brain repair and neurologic recovery after stroke.
The brain has limited repair capacity, and some degree of functional recovery is evident in nearly all stroke patients. Spontaneous repair and recovery processes are multifaceted and include angiogenesis, neurogenesis, axonal remodeling, oligodendrogenesis, synaptogenesis, and inflammatory response. These interwoven events rely on the interaction and coordination among the cells within the neurovascular unit (NVU). , The NUV incorporates neurons, vascular cells (endothelial cells and pericytes), and glial cells (astrocytes, oligodendrocytes, and microglia). , To ensure adequate cerebral blood flow (CBF) and functional neuronal activity, the cross-talk among these cells are tightly regulated, and important mediators of this cross-talk and communication network are exosomes. Exosomes are nanosized vesicles (∼30–100 nm in diameter) that carry and deliver complex cargos of biomolecules (nucleic acids such as DNAs, ribosomal RNAs, circular RNAs, long noncoding RNAs and microRNAs [miRs], proteins, and lipids) and shuttle lipids, cytokines, and nucleic acids between cells. Studies suggest that the miR cargo of exosomes play an important role in mediating intercellular communication within the NUV after stroke. MiRs are single-stranded, 20–30 nucleotides-long noncoding RNAs, and they control multifaceted biologic processes by post-transcriptionally regulating expression of many genes. Stroke impacts brain and circulating miR levels. , The affected miRs further regulate the repair processes after stroke. Here, we will review the post-stroke endogenous brain repair mechanisms as well as the effects of exosomes and miRs on the regulation of these repair and remodeling events.
Emerging preclinical data indicate that exogenous neurorestorative therapies facilitate and amplify endogenous restorative processes, thereby improving functional outcome after stroke. Since the last edition of this book, much progress has been made on developing exogenous cellular and molecular therapies for stroke. New approaches such as direct cell reprogramming, stem cells, and stem-cell derived exosome therapies have opened up the possibility of remodeling neural circuits and obtaining better outcomes post stroke. Direct cell reprogramming can directly convert somatic cells into neurons bypassing the pluripotent stage. Stem cell therapies such as using human umbilical cord blood cells (HUCBCs) and mesenchymal stem cells (MSCs) induce favorable therapeutic effects in stroke animal models. Cell-derived exosomes have been shown to be the primary mediators of therapeutic benefit of the cell-based therapies. , Cell-harvested exosomes provide at least equivalent therapeutic effects compared to the original cellular sources, and exosomes exhibit several advantages over their parent cells. Furthermore, new techniques involving engineering exosomes to modify their content are being developed to improve the efficacy and efficiency of exosome therapies. , In addition, pharmacologic therapies also show beneficial effects for stroke treatment. In this chapter, we summarize and discuss the current knowledge and the potentials of the exogenous cell-based and pharmacologic therapies in facilitating brain remodeling and neurologic recovery after stroke.
After onset of stroke, the induced hypoxic and inflammatory environment triggers endogenous repair mechanisms including angiogenesis, neurogenesis, synaptogenesis, and axon remodeling to rewire the neuronal network. , Here, we will briefly describe these processes ( Fig. 11.1 ).
Vascular responses are initiated as early as 1 hour post stroke and persist for days to weeks. The hypoxia milieu stimulates angiogenic factors to induce the sprouting of capillaries from pre-existing vessels, a multistep process known as angiogenesis. Physiologic angiogenesis ceases in adult rodent brain. However, stroke can reignite angiogenesis in both human and rodent brain. , The ischemic penumbra is the hypoperfused region around the ischemic foci and may potentially be rescued from irreversible infarction. Angiogenesis may increase the microcirculation in the ischemic region, which provides a favorable environment for neuronal plasticity in the penumbra and beyond, thereby yielding an improved neurologic outcome in both experimental stroke and in stroke patients.
Angiogenesis begins with vasodilation of existing vessels that is accompanied by increased vascular permeability and degrading of the extracellular matrix. As a result, proliferating endothelial cells can be recruited to form vascular lumen. , Vascular endothelial growth factor (VEGF) acts on its receptor VEGFR2 to initiate angiogenic sprouting. Migration of invading endothelial cells ensues followed by the proliferation and differentiation of endothelial cells. Angiopoietin 2 released from angiogenic endothelial cells induces the detachment of pericytes, thereby promoting vascular destabilization and further vascular sprouting. , Matrix metalloproteinases (MMPs) secreted by activated endothelial cells and other activated parenchymal cells facilitate pericyte detachment from the vascular wall, cleave endothelial cell-cell adhesions, and degrade the extracellular matrix. , Angiopoietin 1, expressed by various cells, stabilizes the newly formed vascular network and mediates vascular remodeling that results in the formation of vessels with increased diameter. In rodent ischemic brain tissue, the upregulation of VEGF, angiopoietins, and their respective receptors, VEGFR2 and Tie2, persist for at least 28 days. Patients have high serum concentrations of VEGF at 7 days post stroke, which persist up to ∼14 days post stroke. Notably, VEGF, in the acute phase of stroke, induces vascular hyperpermeability that, on one hand, allows extravasation of plasma proteins that serve as a provisional scaffold, paving the way for the sprouting endothelial cells, while on the other hand, results in immature and leaky vessels that can evoke edema and vessel regression over time, especially in diabetic stroke with poor blood supply. , , , As a potential therapy, timing of VEGF activity and administration may differentially affect neurologic outcome post stroke. Preclinical studies demonstrate within 24 hours after onset of ischemic stroke, administration of VEGF induces immature angiogenesis and aggravates the blood-brain barrier (BBB) leakage. , However, either long-term prophylactic administration of VEGF before stroke or late administration (48 hours) after stroke, respectively, have shown improvement of CBF and subsequent improvement of neurologic recovery. , Therefore, as a therapeutic approach, the timing of VEGF administration or inhibition should be thoroughly considered and investigated.
Exosomes participate in post-stroke angiogenesis. In experimental stroke, exosomes derived from NSCs harvested from stroke rat brain promote capillary tube formation of endothelial cell migration compared to the exosomes from non-ischemic brain. In addition to exosomes, proangiogenic miRs are increased in both the brain and circulation post stroke. , , For example, miR-126 is a highly enriched miR in vascular endothelial cells and positively regulates the response of endothelial cells to angiogenic signals. MiR-126 suppresses negative regulators of VEGF pathways such as the Sprouty-relate protein SPRED1 and phosphoinositol-3 kinase regulatory subunit2 (PIK3R/p85-β). By doing so, miR-126 promotes proangiogenic actions of VEGF and fibroblast growth factor (FGF) to induce endothelial cell differentiation and proliferation during vessel development. , During vessel maturation, miR-126 potentiates Ang-1 activity to stabilize the angiogenic vessels. , The circulating level of miR-126 is markedly downregulated in patients with ischemic stroke. MiR-126 expression in both serum and brain tissue is decreased, accompanied by reduced vascular and white matter remodeling in experimental diabetic ischemic stroke. Treatment of diabetic stroke in mice with HUCBCs significantly attenuates miR-126 decline and leads to improvement of neurologic functional outcome. Furthermore, miR-126 deficiency compromises cardiac function after stroke in mice, suggesting a potential role of miR-126 in brain-heart interactions. Thus, therapies elevating miR126 expression may be beneficial to both heart and brain after stroke.
Other miRs likewise may impact angiogenesis and functional recovery post stroke. MiR-146a regulates neuroinflammation , and oligodendrocytosis, and also induces angiogenesis and promotes proliferation and migration of endothelial progenitor cells (EPCs) after ischemic stroke. MiR-146a targets the downstream Toll-like receptor (TLR) signaling pathway that is associated with poor outcome of stroke patients. Therapies targeting TLR signaling remarkably abolish miR-146a decline that stems from stroke-induced fibrin deposition on cerebral vessels. Recently, dysregulation of circulating miR-15a/16-1 cluster was described in stroke patients. Overexpression of miR-15a/16-1 in endothelial cells decreases stroke-related angiogenesis, expands infarction, and aggravates neurologic deficits in mice. Collectively, miRs regulate multiple physiologic and pathophysiologic processes post stroke, importantly, among which is angiogenesis, an important therapeutic target. As additional miR profile studies are conducted, an increasing role of miRs in stroke will likely be further identified, and thereby more precise and specific stroke therapies may be established.
The majority of neurons are generated during the embryonic phase. After birth, mature neurons are continually replenished via the proliferation and differentiation of neural stem cells (NSCs) and neural progenitor cells (NPCs) that reside throughout life in the subgranular zone of hippocampal dentate gyrus and the subventricular zone of the lateral ventricle (V/SVZ), a process called adult neurogenesis. , Physiologically, this process is under strict control via cell apoptosis and proliferation. , Post stroke, neurogenesis is activated by multiple ways. Gene profile analysis shows that stroke induces NPC proliferation by upregulating the gene expression of cyclin-dependent kinase (CDK) while downregulating its inhibitors such as p27kip1. In rodent models of stroke, 2 days after stroke, a higher (31%) than usual (15%–21%) percentage of NPCs in V/SVZ entering the cell cycle increases NPC proliferation to a peak level between 4 and 7 days post stroke. This increase may be attributed to a decline in G1 phase of cell cycle that shortens the cell-cycle length from 19 hours to 11 hours, and concomitantly retains the newly divided daughter cells within the cell cycle, expanding the progenitor pool of SVZ. Fourteen days post stroke, the cell-cycle length returns to normal level with lengthening of the G1 phase, allowing increased numbers of daughter cells to enter the cell cycle and differentiate into neuroblasts. , Neuroblasts then migrate in chains or individually to reach the ischemic boundary zone (IBZ) along a lateral path, distinct from the usual dorsal and ventral migration in normal brain. , In the process, neuroblast division persists and NSCs facilitate both generation and migration of NPCs. ,
Exosomes and miRs also participate in neurogenesis after stroke. Exosomes derived from cerebral endothelial cells harvested from ischemic rat brain enhance NPC proliferation and their differentiation to neurons. Populations of mature miRs in the NPCs within the SVZ are upregulated and downregulated after stroke. The miR-17-92 cluster regulates both neurogenesis and angiogenesis. , The miR-17-92 cluster modulates NPC proliferation not only during development but also during neurologic disorders such as stroke. The miR-17-92 cluster is robustly upregulated in the V/SVZ NPCs after stroke, overexpression of which enhances stroke-induced NPCs proliferation, whereas knockdown of the miR-17-92 cluster yields opposite results. , This positive effect of miR-17-92 on neurogenesis is partially attributed to suppression of phosphatase and tensin homolog deleted on chromosome 10 (PTEN), a protein negatively regulating embryonic NSC proliferation and survival. , The miR-17-92 cluster is regulated by the sonic hedgehog (Shh) signaling pathway whose downstream protein, c-Myc, binds to the promoter region of the miR-17-92 cluster in NPCs, and this binding is enhanced after stroke. , Exogenous administration of Shh further upregulates the miR-17-92 cluster expression in V/SVZ NPCs and subsequently amplifies NPCs’ proliferation.
MiR-124a, a brain-enriched microRNA, mediates neuronal differentiation by suppressing the expression of SRY-box transcription factor 9 (SOX9). MiR-124 is significantly decreased within 24 hours after stroke onset, and serum miR-9 is decreased in patients with larger stroke. Both serum miR-124 and miR-9 levels within 24 hours post stroke were negatively correlated with infarct volume and plasma high-sensitivity C-reactive protein levels. Stroke lowers miR-124a expression in SVZ NPCs, which enhances NPC proliferation by targeting Jagged-1, a ligand that activates the Notch receptors. The Notch signaling pathway plays a key role in the maintenance of the embryonic NSC pool and gliogenesis, and activation of Notch increases NPC proliferation by stroke, whereas blockage of Notch abolishes stroke-stimulated progenitor cell proliferation. , , Additionally, stroke downregulates Let-7 and miR-9, both of which mediate adult neurogenesis by regulating the balance between the proliferation and differentiation of NSCs through the orphan nuclear receptor TLX. , , Stroke also alters the expression of Wnt signaling and bone morphogenic protein (BMP) family genes that regulate neurogenesis in adult brain. Wnt/β-catenin signaling represses Let 7 in tumor cells, and miR-92 regulates BMP signals. , MiR-145 is another miR whose expression is increased after stroke, and it guides NSC differentiation via the Sox2-Lin28/let-7 signaling pathway. , Accordingly, these miRs and related signaling pathways may form a network that controls the adult neurogenesis after stroke. Further investigations are warranted regarding individual miRs and signaling pathway as well as their interaction in the progression from the SVZ stem cell to neurons.
Along with angiogenesis and neurogenesis, axonal remodeling is important for the neurologic recovery after stroke. , Several molecules promote the axonal outgrowth. ATRX, an ATP-dependent DNA modifying enzyme, is necessary for post-stroke axonal sprouting, and insulin-like growth factor-1(IGF-1) helps maintain cortical neurites after stroke. Weeks after stroke, there is a steady and sizable increase in numbers of axons and the apical dendrite density in the brain penumbra of rodents , and new axonal initial segments are formed within the peri-infarct cortex in a rodent model of focal cortical stroke and white matter stroke. Thus axonal sprouting is induced by stroke; however, this occurs within a hostile environment for axonal remodeling. Oligodendrocytes and myelin debris restrict axonal outgrowth by releasing myelin-associated inhibitors that include Nogo-receptor (NgR), myelin-associated glycoprotein (MAG), , oligodendrocytes myelin glycoprotein (OMgp), , transmembrane semaphoring 4D (sema4D), Ephrin B3, 118 and ephrin-A5. The post-stroke reactive astrocytes secrete chondroitin sulphate proteoglycans (CSPGs), a class of extracellular matrix macromolecules, to inhibit the axonal outgrowth. The CSPGs are expressed most abundantly within the core of the lesion and diminish gradually to the lesion boundary. The exact inhibitory mechanisms of CSPG are not completely clear. The proteoglycans may serve as a physical barrier that indirectly prevents neurons being exposed to neurite-promoting components of the extracellular matrix. We note, however, that the roles of CSPGs on axonal outgrowth are multifaceted. Certain proteoglycans like laminin, fibronectin, and neural cell adhesion exert positive regulation on neurite growth. Therefore, further insight into the mechanisms targeting CSPG and myelin are still needed to facilitate the therapies for axon remodeling.
In addition to axon outgrowth, the remyelination of demyelinated axons or newly sprouted axons are essential to reinstating salutatory conduction, restoring axonal integrity, and rebuilding the lost neuronal circuitry. , Oligodendrocytes mediate myelination. Oligodendrocytes are differentiated from non-myelinating oligodendrocyte progenitor cells (OPCs) that are widely distributed throughout the adult central nervous system (CNS). In adult mouse brain, OPCs maintain a proper density by balancing active growth with self-repulsion and generation of oligodendrocytes, albeit less frequently. They also promote angiogenesis to secure sufficient blood supply for the proper postnatal myelination in the white matter via hypoxia-inducible factor (Hif) and Wnt pathways. In addition to OPCs, the oligodendrocytes can also be generated by GFAP positive astrocytes, NSCs, and NPCs in the V/SVZ of adult mice brain.
Oligodendrocytes are vulnerable to stroke. Since mature oligodendrocytes are unable to proliferate and the injured ones are no longer functional, achieving remyelination requires generation of new oligodendrocytes. , , Using genetic fate mapping strategy in adult mice NPCs, studies show that oligodendrocytes involved in post-stroke white matter remodeling are derived from the OPCs in white matter and from the NPCs in the SVZ. During the first 2 weeks after onset of stroke, OPCs robustly increase in ischemic boundary regions of mouse brain. Two months later, a portion of OPCs in peri-infarct white matter are found to display oligodendrocyte morphology and express protein components of myelin, cyclic nucleotide 3′-phosphodiesterase (CNPase), and myelin basic protein (MBP) in rodent models of stroke. , Another study on a rodent model of white matter stroke reported that OPCs proliferate after stroke, but reach a peak level at day 4 post stroke, earlier than previous studies, and then decline at day 14 post stroke. This study shows that the majority of the proliferating OPCs are retained in the progenitor stage and a minority of them adopt an astrocytic fate rather than maturing into oligodendrocytes. No initial remyelination is detected in white matter stroke, even in the candidate peri-infarct zone where intact axons reside, leaving unmyelinated fibers in the corpus callosum. This phenomenon is more pronounced in aged mice and involves the NgR1 signaling, blockage of which reduces the OPC astrocytic transformation, enhances oligodendrogenesis, and improves behavioral recovery after stroke. , The OPCs that are able to differentiate most likely originate from the resident OPC pool in the white matter where SVZ lineage cells make no contribution, regardless of the proximity of the peri-infarct zone to the SVZ. These discrepancies may be due to the differences in stroke subtypes and study design, and therefore the distinct progression of different white matter injuries should be considered. For inflammatory or toxic white matter injury, SVZ-derived OPCs can promote oligodendrogenesis, a mechanism also seen in rodent models of middle cerebral artery occlusion (MCAo) stroke. , , By contrast, in white matter stroke, local OPCs replenish the required oligodendrocytes. , ,
Like axonal outgrowth, oligodendrogenesis is controlled by both intrinsic and extrinsic inhibitory cues. Blood-derived factors, e.g. fibrinogen and fibrin, not only trigger the death of mature oligodendrocytes in an autophagy-dependent manner, but also inhibit the differentiation of OPCs. , Dysregulation of Wnt-β-catenin signaling in OPCs leads to profound delay of remyelination in the rodent CNS. In vitro and in vivo studies show that semaphorin 3A reversibly inhibits OPC differentiation and remyelination. Likewise, the Lingo 1 (leucine-rich repeat and immunoglobin-like domain-containing Nogo receptor interacting protein 1), myelin debris, and ECM such as hyaluronan , and CSPGs , all negatively regulate oligodendrocyte differentiation and myelination in a rodent model of demyelinating disease. Within the NVU, astrocytes may promote proliferation of OPCs via connexin47 and oligodendrogenesis by secreting brain-derived neurotrophic factor (BDNF). , Pericytes induce OPC differentiation during remyelination by releasing Lama2 that also promotes OPC survival. , Highly activated amoeboid microglia in white matter are essential to the hemostasis of both oligodendrocytes and OPCs in adult brain. After brain injury, microglia phagocytize the toxic myelin debris that hinders remyelination, and its anti-inflammatory subtype (M2 microglia) could further promote OPC differentiation. , Pro-inflammatory subtype of microglia (M1) could promote early postnatal oligodendrogenesis, but they may be detrimental during remyelination. ,
Emerging data indicate that miRs are required for maintaining OPCs in the undifferentiated state and for preserving myelin in mature oligodendrocytes. , MiR-146, miR-219, miR-138, miR-9, miR-200b, miR-23, miR-19b, and the miR-17-92 cluster participate in the regulation of oligodendrocyte survival, proliferation, and differentiation as well as myelin maintenance that impact the demyelination-related diseases (e.g., multiple sclerosis, ischemic stroke, and leukodystrophy). , For example, preclinical studies show that stroke considerably downregulates miR-9 and miR-200b in white matter and their levels inversely correlate with the expression of serum response factor (SRF), a transcription factor necessary to OPC differentiation. , MiR-17-92 cluster and miR-219 are abundant in human white matter and are expressed in cultured primary human oligodendrocytes. In mouse studies, embryonic deletion of the miR-17-92 cluster in OPCs causes a decrease of OPC proliferation and increased OPC death, which are likely attributed to inactivation of protein kinase B (Akt) signals induced by augmentation of PTEN proteins. , MiR-219 is enriched in myelinating oligodendrocytes compared to their levels in OPCs. , It plays a critical role in coupling differentiation to proliferation arrest in the oligodendrocyte lineage, enabling the rapid transition from proliferating OPCs to myelinating oligodendrocytes. , Elevation of miR-219 in OPCs propels OPC differentiation into mature oligodendrocytes by repressing genes of platelet-derived growth factor receptor α (PDGFRα), SRY (sex determining region Y)- box 6 (Sox6), and Hes family bHLH transcription factor 5 (Hes5), factors inhibiting OPC differentiation. , Notably, the effect of miRs on stroke-induced oligodendrogenesis is just beginning to be investigated. Additional in vivo experiments focusing on amplification of stroke-induced oligodendrogenesis by modulating miR levels are warranted.
Synaptogenesis is the process of generating new synapses between different neurites. Angiogenesis can improve synaptogenesis by providing increased oxygen supply. The expression of synaptophysin, a pre-synaptic vesicle protein indicating synaptogenesis, is increased after cell therapy treatment of stroke animals with a concomitant improvement in post-stroke functional outcome. , In vitro and in vivo studies show that miR-181 promotes synaptogenesis but reduces axonal outgrowth in cortical neurons. Inhibition of miR-181 benefits the long-term behavioral recovery in mice after stroke. In mouse brain, miR-29a/b curbs the differentiation of filopodial-like protrusions into mature dendritic spines on hippocampal neurons, but miR-29b is reduced in infarct tissue after stroke, which contributes to neural cell death and infarct size. , In addition, several miRs that are downregulated or upregulated in the circulation of stroke patients affect synaptogenesis. For example, in mice, miR-185 is required for spine formation and dendritic branching and growth. Circulating miR-185 is decreased in both the acute and subacute phase of stroke patients. In vitro and in vivo studies show that miR-132 increases dendritic length and widens dendritic protrusions, and miR-125 can promote the formation of long and thin dendritic protrusions. Both plasma levels of miR-132 and miR-125 are elevated in stroke patients. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here