Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Portal hypertension is most commonly a manifestation of underlying liver parenchymal disease and worsens with increasing severity of cirrhosis. It is responsible for complications, such as the development of varices and variceal hemorrhage, among chronic liver disease patients and often portends the need for liver transplantation. Fifty percent of patients with cirrhosis have gastroesophageal varices, and approximately one third of these patients will go on to develop variceal hemorrhage. The continuum of gastroesophageal varices to variceal hemorrhage is linearly correlated with hepatic function and mortality. Although advances in the management of acute variceal bleeding over the last decade have resulted in a reduction in overall mortality, acute variceal hemorrhage continues to have high morbidity and mortality. In fact mortality from variceal bleeding ranges from 5% to 68% among Child-Turcotte-Pugh class A and C cirrhotic patients, respectively. This correlation highlights the need for an algorithmic approach to caring for patients with cirrhosis with advanced portal hypertension and variceal bleeding.
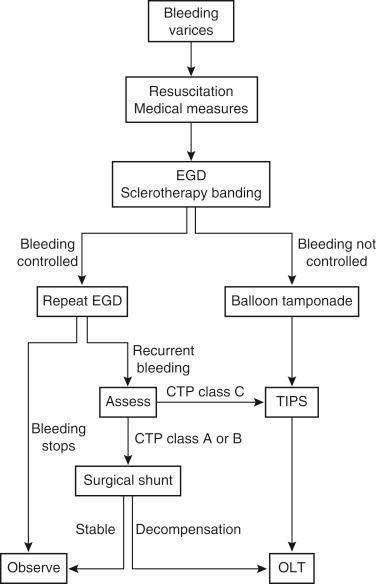
The presence of portal hypertensive varices is not reliably correlated with bleeding. More than 50% of patients with varices will not experience bleeding, and therefore varices are generally medically managed. Avoidance of hepatotoxins and the use of β-blockers are the mainstays of therapy. β-blockers reduce portal hypertension by constriction of splanchnic vasculature. Endoscopic therapies, such as injection sclerotherapy and banding, have been associated with a reduction in bleeding but have not been shown to improve mortality. Acute variceal hemorrhage, however, requires an algorithmic approach that involves emergent resuscitation, optimization of medical management, endoscopic diagnosis, and directed therapy ( Fig. 38-1 ).
When severe, acute variceal hemorrhage can be associated with hemorrhagic shock. Therefore resuscitation should be prompt and aggressive, including airway protection, large-bore intravenous access, and crystalloid and colloid product infusion, with a goal of maintaining hemodynamic stability. Although resuscitation of the acutely bleeding patient is of primary importance, if possible the central venous pressure should be kept less than 10 mm Hg with a target hemoglobin level of 7 to 8 ng/dL. In addition, octreotide and Protonix drips should be initiated. Octreotide is a synthetic analogue of somatostatin and serves as a splanchnic vasoconstrictor through inhibition of glucagon and other vasodilatory peptides. Protonix suppresses gastric acid secretion through inhibition of the parietal cell hydrogen-potassium adenosine triphosphate (ATP) pump. Interestingly, bacterial infection has been associated with variceal bleeding and is an independent risk factor for failure to control bleeding, early rebleeding, and death. Intravenous ceftriaxone or oral norfloxacin should be administered in the setting of an acute variceal hemorrhage.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here