Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pain is highly prevalent in the oncology patient population, estimated to be more than 70% in advanced stages of disease. Pain is not necessarily associated with lower survival odds in patients with advanced cancer, but it does impact the overall quality of life. Different types of pain syndromes are present in all stages of cancer and are not adequately treated in 56% to 82.3% of patients. Painful metastases may respond to radiation, chemotherapy, hormonal therapy, and/or regional nerve blocks. Radiation therapy (RT) is 65% to 70% effective at relieving pain. It reduces the need for opioid medications and the subsequent risk of pathologic fractures. Given the increased survival due to novel cancer-directed therapies, a growing number of patients may experience persistent pain. Up to 10% of cancer survivors may experience chronic severe pain that interferes with daily function.
The goal of pain management in this setting is therefore to relieve pain to a level that allows an acceptable quality of life. It is not realistic to expect complete relief of pain, but rather a state of tolerable pain and improved quality of life. Patient-related factors that can predict a lower likelihood of achieving pain stabilization include neuropathic pain, incident pain, psychological distress, and comorbid substance use disorder. When the goal is the complete elimination of pain, the risk of unacceptable or unsafe adverse effects of the therapies typically begins to outweigh the benefits. The balance of pain management and acceptable level of risk can be best achieved through different mechanisms, depending on the etiology of the pain.
The first step to effective pain management is a global assessment and reassessment. Through this, a detailed history, physical examination, psychological assessment, and pain severity can be elucidated. This information will inform a diagnosis of the type and etiology of the pain, which is needed in order to effectively and safely choose a therapeutic regimen, accounting for patient-specific considerations. Nonpharmacological strategies can also help effectively address pain including, for example, such interventions as massage, acupuncture, exercise, cognitive behavioral therapy, and physical therapy.
There are various types of pain, and a general understanding of the etiology of the pain is critical to help guide therapy selection ( Table 26.1 ). Most patients with advanced cancer have at least two types of cancer-related pain. Pain may be nociceptive due to the stimulation of the pain receptors on normal sensory nerve endings. Nociceptive pain is further categorized into visceral or somatic pain. Visceral pain is secondary to the tumor itself when located in the abdominal cavity, and is generally responsive to a combination of opioids, adjuvants, and steroids. , Pain may be somatic; bony lesions are a prime example. While radiation is aimed at relieving the pain from bony lesions, it can take up to 10 days to start to work and may even result in a short-term increase in pain. Pain flares in the initial days following treatment are associated with a significant impact on activities of daily living and insufficient relief from increases in pain medications. Nonsteroidal antiinflammatory drugs (NSAIDs) and corticosteroids, together with opioids, are most effective for this type of pain, with the addition of bisphosphonate therapy for moderate pain relief and the prevention of skeletal-related events. , , , Radionuclide therapy may also offer some pain relief in select patients.
| Type of Pain | Nonpharmacologic Treatments | Pharmacologic Treatments | Comments |
|---|---|---|---|
| Somatic (i.e., bone pain) |
|
Nonsteroidal antiinflammatory drugs; steroids; opioids | Bone pain is best treated with steroids or NSAIDs. Dexamethasone 8 mg preferred daily dose—short-term treatment only. Topical NSAIDs may offer some local relief. |
| Visceral (i.e., abdominal tumor) | Hot compresses |
|
Opioids and steroids may help reduce tumor-associated pain and inflammation. If nerve compression, anticonvulsants can be considered. |
| Neuropathic (i.e., spinal cord compression; chemotherapy-induced peripheral neuropathy) |
|
|
First-line therapies—adjuvants and antidepressants. Tramadol and tapentadol may be considered. Opioids are second-line or as bridge to onset of first-line agents—consider methadone if refractory. |
| Mucositis | Frequent rinses, mouth hygiene |
|
Mouth rinses and gabapentin can help prevent and treat mucositis. Rinses may have antibiotic, antihistamine, antacid, opioid, and nonopioid (ketamine, doxepin) ingredients. Systemic opioids are used with variable efficacy and significant adverse effects. |
Neuropathic pain can come from a variety of sources. It may be due to nerve compression of a tumor pressing on a nerve, as can be seen with spinal metastases pressing on the nerve root. It may also be from a central source as a result of direct injury to the central nervous system (CNS), as can be seen with spinal cord compression. When neuropathic pain is peripheral in nature, it is due to a lowered firing threshold of the sensory nerves, as with chemotherapy-induced peripheral neuropathies. Mixed syndromes can also occur as a result of injury to both central and peripheral nerves, either from two different injuries or when an unrelieved peripheral injury leads to a centrally sensitized state. Finally, pain may be sympathetically maintained, as with complex regional pain syndrome following an acute fracture of trauma. Neuropathic pain is generally more difficult to treat and may require multiple trials of analgesics from different classes before finding a regimen that is effective.
Local irritation from radiation treatment may also induce painful mucositis. Mucositis is the result of deep tissue damage resulting in epithelial damage and ulceration. The associated pain can be difficult to control but may be best relieved with mouth hygiene, medicated mouth rinses, opioid analgesics, and possibly, the anticonvulsant, gabapentin. There is also some evidence from a small study indicating that ketamine mouthwash (20 mg/5 mL) leads to a clinically meaningful decrease in mucositis-related mouth pain and pain with swallowing.
The European Society of Medical Oncology (ESMO), the National Cancer Consortium Network (NCCN), the World Health Organization (WHO), and the American Society for Clinical Oncology (ASCO) all have published guidelines for the management of cancer pain in adult patients. , , , There are general principles of cancer pain management that align with the guidelines and which should be considered best practices.
Treat the underlying cause with cancer-directed therapy, when possible. RT offers the benefit of pain relief and improved symptoms a few weeks after therapy is complete. During this time, pain and pain flares should be adequately managed using these principles.
Patients should take an active role in their therapy. When patients are involved in creation of the regimen, it is more likely to fit into their daily lives and allow for increased adherence. Involving a patient in pain management improves communication and pain relief. , Pain assessment should be integrated into standard care for cancer patients.
Pain needs to be assessed and reassessed regularly, as it can change constantly and medications may accumulate or become intolerable or less effective over time. Ongoing reassessments of pain will help tailor the analgesic regimen and will also allow for medical workup of new or worsening pain.
Always consider the psychosocial, psychological, spiritual, and cultural beliefs that make up the pain experience.
In patients presenting with moderate to severe pain, opioids are first-line therapies. The initial strength and/or dose of the opioid should be chosen to align with the severity of the pain.
Breakthrough pain is defined as “a transitory flare of pain that occurs on a background of relatively well-controlled baseline pain” and in general is moderate to severe in intensity, comes on quickly, and is of short duration.
Around-the-clock (ATC) analgesics, along with rescue analgesics, prevent the onset of pain and gaps in analgesia, treat breakthrough pain, and allow for dose titration in order to prevent end-of-dose failure.
The oral route should always be preferred when it is able to be used, exceptions include severe vomiting, bowel obstruction, severe dysphagia or confusion, or when needing rapid dose escalation with intravenous medications.
The treatment of mild pain should begin with acetaminophen and/or NSAIDs, if not contraindicated. , , Acetaminophen and NSAIDs can be added to opioid therapy for moderate to severe pain.
Despite multiple guideline recommendations for use in the cancer population experiencing mild pain, there is limited evidence regarding acetaminophen in the treatment of cancer-related pain. Additionally, the exact mechanism of action of acetaminophen is still uncertain. It is theorized that acetaminophen has peroxide-dependent cyclooxygenase (COX) inhibition, serotonergic pathways, and endocannabinoid activity that contribute to centrally-mediated analgesia but not to peripheral antiinflammatory activity. , Although the mechanism of action of acetaminophen is unclear, there are well-documented risks associated with acetaminophen use—primarily dose-related liver toxicity. The maximum dose of all prescription opioid combination products is 325 mg per tablet, due to an increased risk of acetaminophen toxicity associated with the opioid/acetaminophen combination products. The maximum US Food and Drug Administration (FDA) recommended daily dose of acetaminophen is still 4000 mg/day, but even this is different from the manufacturer’s maximum daily recommended dose of 3000 mg/day. For patients with liver dysfunction or who have alcoholic cirrhosis, the maximum recommended daily dose is 2000 mg. Despite the lack of evidence for use in cancer-related pain, acetaminophen is best used on a regular schedule as pain is often too severe for it to be effective when taken as needed.
NSAIDs also comprise the first tier of the analgesic ladder and are recommended in addition to opioids in moderate and severe pain. Cochrane reviews assessing the literature on NSAIDs for cancer-related pain demonstrate inconclusive evidence for the use of NSAIDs alone or in combination with opioids for the treatment of any severity of cancer-related pain. There is limited evidence that 25% to 50% of cancer patients with moderate or severe pain may achieve relief within 1 to 2 weeks of treatment, as was demonstrated in 4 out of 11 studies. NSAIDs are generally effective and recommended for the treatment of bone pain due to metastases. , ,
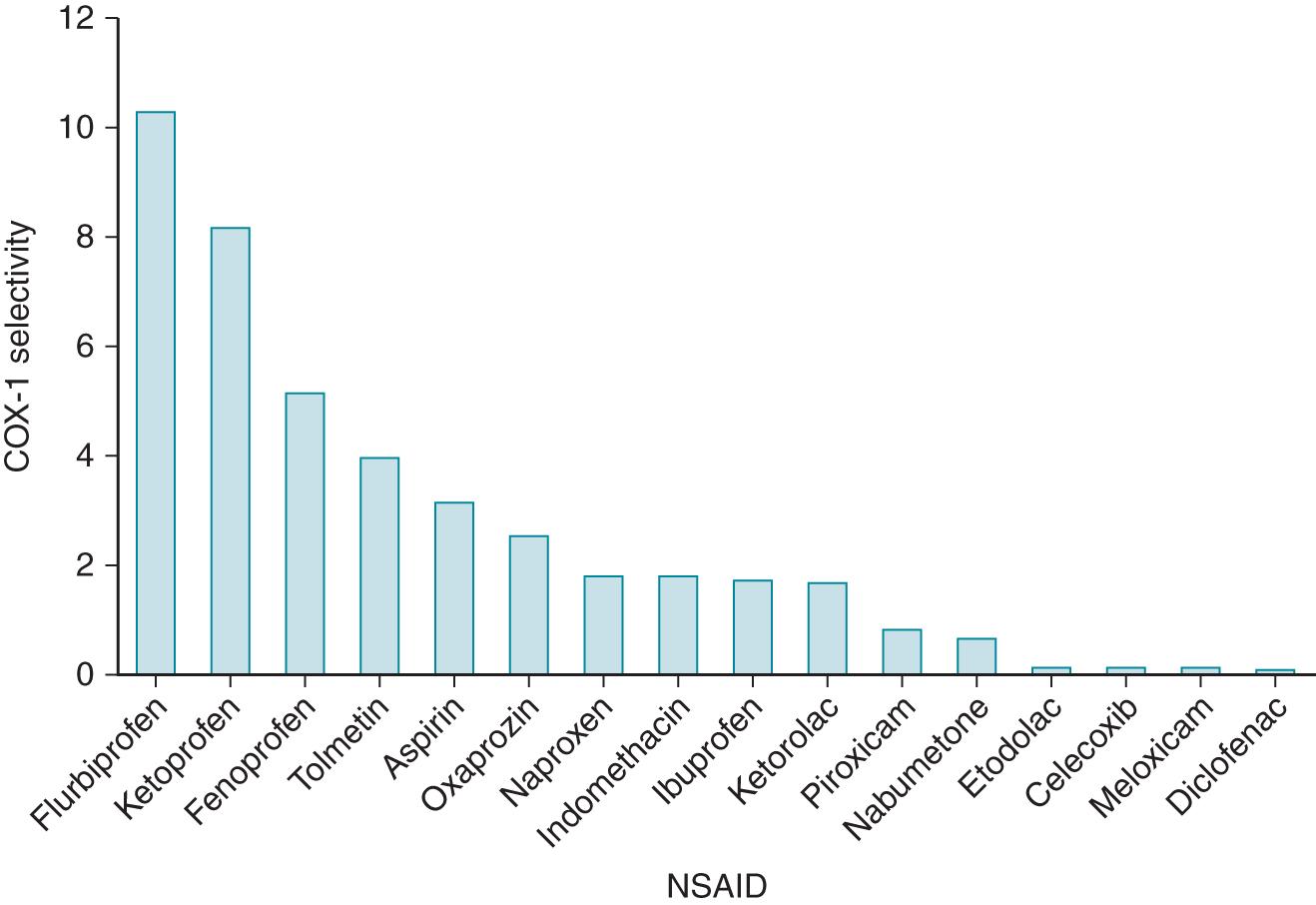
There is also no evidence for which NSAID is preferred for the treatment of cancer-related pain. NSAIDs inhibit the COX enzymes 1 and 2 with varying agent-specific selectivity for each receptor ( Fig. 26.1 ). The COX enzymes are key in the inflammatory cascade, and inhibition results in decreased inflammation leading to decreased overall pain. Those agents that are more COX-1 selective are associated with an increased risk of bleeding, and those that are more COX-2 selective are associated with increased cardiovascular risks, such as myocardial infarction and thrombotic stroke. , All NSAIDs are associated with an increased risk of renal failure. The use of NSAIDs may thus be limited in many cancer patients due to the occurrence of thrombocytopenia and the increased bleeding risk or neutropenia and the risk of masking fevers. In general, the lowest effective dose for the shortest duration possible should be implemented in order to minimize the risk of adverse effects. For patients at high risk for gastrointestinal bleed, the addition of a proton-pump inhibitor for the duration of NSAID therapy should be employed.
Any opioid may be considered for pain relief—efficacy is dependent on dosing and tolerability. , The correct dose of opioid is the dose that relieves the patient’s pain to an acceptable level. Knowledge of the pharmacokinetic and pharmacodynamic considerations for individual agents will help in guiding the selection of opioids to optimize safety and efficacy.
All opioids are metabolized by the liver. When selecting an agent for a patient with liver dysfunction (known or anticipated due to cancer or cancer treatment), the dose and frequency are most important to consider. Lower starting doses (50% of initial recommended opioid-naïve dosing) and extended durations (every 6 hours instead of every 4 hours) may allow for increased tolerability and safety initially and then doses and frequencies can be adjusted as tolerated.
Patient preference should also be taken into consideration. If a medication has worked in the past, it will be likely to be effective once again, and tolerability will have already been established in the patient. Ease of administration and frequency of dosing are important variables that must fit into the patient’s lifestyle and schedule.
Patients may report allergies to select opioids. True opioid allergy is anaphylaxis and occurs in less than 2% of patients. Many reported opioid allergies are intolerances to the medications. It is important to make a distinction between true allergies and intolerances. In the setting of a true opioid allergy, fentanyl, methadone, tramadol, and tapentadol are fully synthetic and are preferred as they are not likely to have cross-reactivity with an allergy to morphine or the other semi-synthetic agents.
When selecting an agent, it is important to consider that the efficacy of the weak opioids (tramadol, tapentadol, codeine) is limited. Data does not support a significant difference between using weak opioids in combination with nonopioids versus using nonopioids alone. Low doses of strong opioids may be preferred and have supporting evidence in the treatment of cancer-related pain.
Opioids can be administered via oral, sublingual, buccal, transdermal, intravenous, subcutaneous, and rectal routes. Agent-specific availability will vary. The route should be based on the patient’s needs, but oral is always the preferred route when it is possible. , , Concentrated forms of morphine and oxycodone are commercially available and can be administered sublingually or buccally. The absorption is dependent on the lipophilicity of the drug. Oxycodone and morphine are not lipophilic and so they are mostly absorbed via the gastrointestinal (GI) tract, the concentrated form allows for a small volume to be delivered in the setting of difficulty swallowing, to avoid the risk of aspiration. Fentanyl and buprenorphine are highly lipophilic and as such, are commercially available in transmucosal products. Methadone is available as a concentrated solution and can also be absorbed through the oral mucosa if permitted sufficient time to absorb in the oral cavity. Subcutaneous dosing is an alternative to sublingual dosing when the parenteral route is preferred but the intravenous route is not available. Subcutaneous dosing is equal to that of intravenous dosing and can be used for a short duration of therapy. Subcutaneous lines can administer up to 3 to 5 mL/h and retain integrity for up to 7 days, at which point they will need to be rotated to a different site. Specific considerations about product availability will further be discussed by individual agent.
Despite limited data on the use of tramadol in cancer patients, it is widely used in the treatment of cancer-related pain and in palliative care. There are no studies comparing tramadol to the other weak opioids. Tramadol is a weak mu opioid receptor agonist with 6000 times less affinity than that of morphine, and it exhibits inhibition of monoamine reuptake. Tramadol should be used with caution in patients with a history of or risk for seizures, with a history of substance abuse or suicide risk, and in older adults. It is also associated with significant drug-drug interactions, including other CNS depressant drugs or serotonin-modulating agents and moderate to strong inhibitors of cytochrome P450, 3A4, and 2D6. The main adverse effects are nausea, vomiting, constipation, dizziness, and somnolence. Tapentadol is a weak mu opioid receptor agonist, with 50% of the affinity of morphine for the mu receptor, and an inhibitor of adrenergic reuptake. There is also no evidence about the use of tapentadol for the treatment of cancer-related pain. It is associated with the same precautions as tramadol and similar adverse effects.
Codeine is a pro-drug that requires conversion in the liver, via the CYP 2D6 enzyme, to morphine. In patients who are poor metabolizers via this enzyme, codeine will not provide analgesia since it will not convert to its active form. In patients who are rapid metabolizers, codeine rapidly converts to morphine and can lead to increased adverse effects and risk of sedation and respiratory depression. The evidence for codeine in the treatment of cancer pain is also controversial. A Cochrane Review demonstrated some evidence that codeine is more effective than a placebo in the treatment of cancer-related pain, but at the expense of increased nausea, vomiting, and constipation and was unable to provide formal recommendations on the role of codeine in cancer pain management. Without strong evidence for efficacy and a significant risk of adverse effects, there is evidence suggesting consideration of using lower doses of strong opioids for mild to moderate pain instead.
The strength of an opioid is dependent on its dose. Low doses of oxycodone may be as effective as higher doses of morphine if dosed based on potency. The route of administration will also impact the strength of the dose as well as the onset of the medication. All of these elements must be considered when selecting a strong opioid. A select set of opioids will be reviewed as these are the most commonly utilized agents. For a complete list of strong opioids and considerations in opioid selection, see Table 26.2 .
| Opioid | Selection Considerations |
|---|---|
| Morphine | Metabolites accumulate in organ dysfunction. Can be given in ultra-low-dose for patients with intolerances to opioids. |
| Hydromorphone | May accumulate with continuous administration; five to seven times more potent than morphine |
| Oxycodone | Oral formulation only in the United States; may accumulate with long-acting administration in organ dysfunction. Extended-release product may be not be preferred based on insurance coverage. |
| Hydrocodone | In combination with acetaminophen in short-acting formulation. Acetaminophen limits dose titration. |
| Oxymorphone | Orally only in the United States, may accumulate with long-acting administration in organ dysfunction |
| Fentanyl | Safe alternative in true opioid allergy. Requires adipose tissue for adequate absorption. Preferred in renal dysfunction. |
| Methadone | Safe alternative in true opioid allergy. Preferred in renal dysfunction. Drug interactions, complex pharmacokinetics. Dosing and monitoring best left to specialists. |
Morphine is the gold standard mu opioid receptor agonist and the preferred opioid for the initial treatment of cancer-related pain. It is the only naturally-occurring opioid. Morphine is metabolized in the liver to morphine 6-glucuronide and morphine 3-glucuronide. In patients with renal insufficiency, these metabolites accumulate and can lead to an increased risk of toxicity, including myoclonus, seizures, and respiratory depression. Morphine is associated with histamine release from mast cells, which plays a role in opioid-induced pruritus. Morphine is available in an extended release formulation that lasts 8 to 12 hours, as well as long-acting capsules that can be opened and the granules administered in applesauce or in a gastric tube. It is also available in immediate release, liquid solution, concentrate, and parenteral formulations.
Oxycodone is a semi-synthetic opioid. It is metabolized to oxymorphone and noroxycodone. These metabolites are clinically insignificant unless in the setting of renal or liver insufficiency. Oxycodone is available in an immediate release and an extended-release product that lasts up to 12 hours. A small percentage of patients may need to have frequencies adjusted to every 8 hours if experiencing end-of-dose failure, or requiring higher doses that are better tolerated when given in a smaller amount as an extra dose. The extended-release product may not be preferred by many patients’ insurance carriers, as fentanyl and morphine are generally preferred agents. Oxycodone is only available orally in the United States and is available as a liquid and an oral concentrate if swallowing is a concern.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here