Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Crowding, disorder, and atypia of epidermal keratinocytes
Arises from the basal layer
Solar elastosis typically present
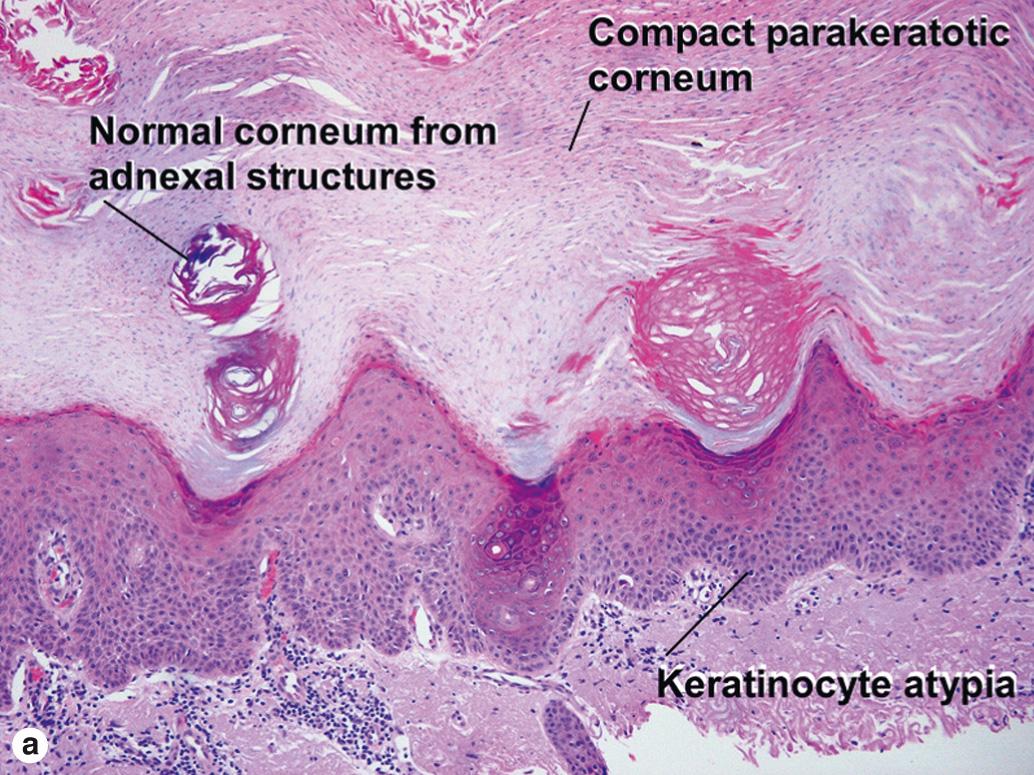
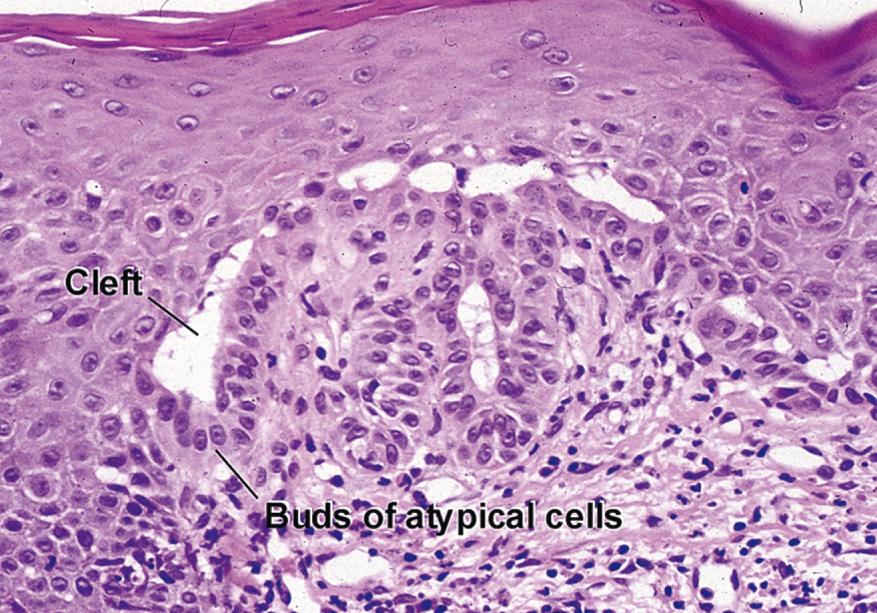
Atypical cells commonly surround the follicular infundibulum. In two-dimensional sections, they appear to form a shoulder zone peripheral to the benign follicular epithelium. The overlying stratum corneum may be normal or may have features of a “malignant horn.” A malignant horn is a compact, eosinophilic stratum corneum with hyperchromatic bricklike parakeratosis. The brightly eosinophilic zones alternate from left to right with pale, basophilic lamellar keratin originating from adnexal structures (flag sign). Broad-based buds of atypical keratinocytes are commonly seen extending downward from the epidermis. The budding can become complex, and separation from superficially invasive squamous cell carcinoma may sometimes be difficult.
Crowding, disorder, and atypia of epidermal keratinocytes
Acantholysis in areas of atypia
Overlying “malignant horn” may be present
Complex epidermal budding may be present
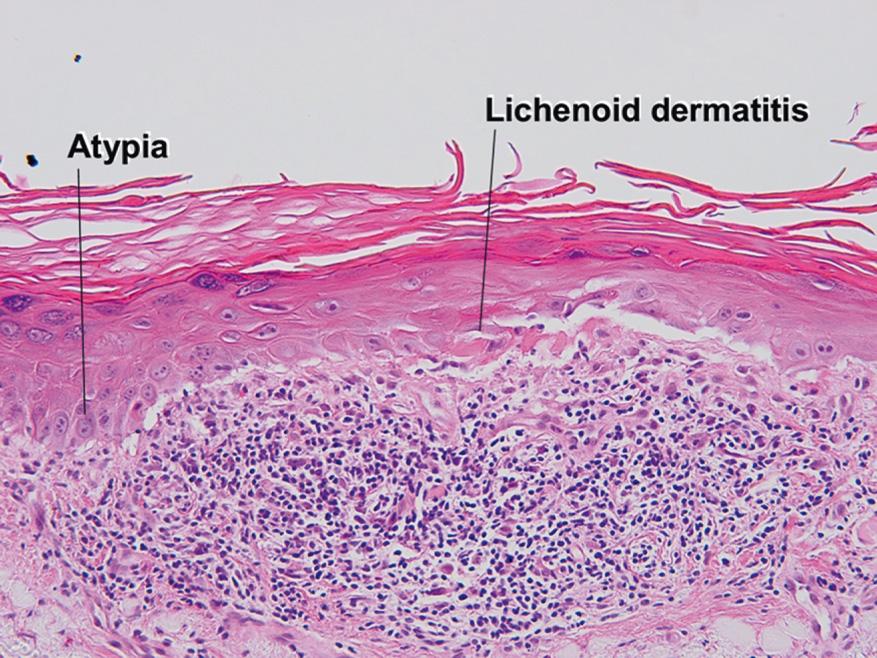
Crowding, disorder, and atypia of epidermal keratinocytes
Areas of lichenoid interface dermatitis
Overlying “malignant horn” may be present
Crowding, disorder, and atypia of epidermal keratinocytes
Prominent overlying “malignant horn”
Acanthosis, often with complex epidermal budding
Red, fibrotic stroma often displaces solar elastosis downward
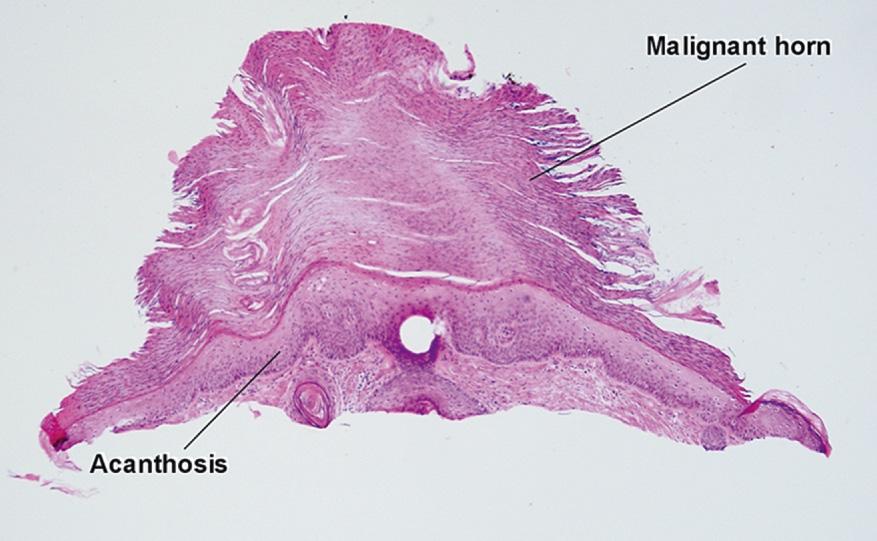
Focal, full-thickness atypia
Unlike Bowen disease, bowenoid actinic keratosis never demonstrates anaplastic nuclei, clonal nesting, buckshot intraepidermal scatter of atypical cells, or full-thickness follicular involvement.
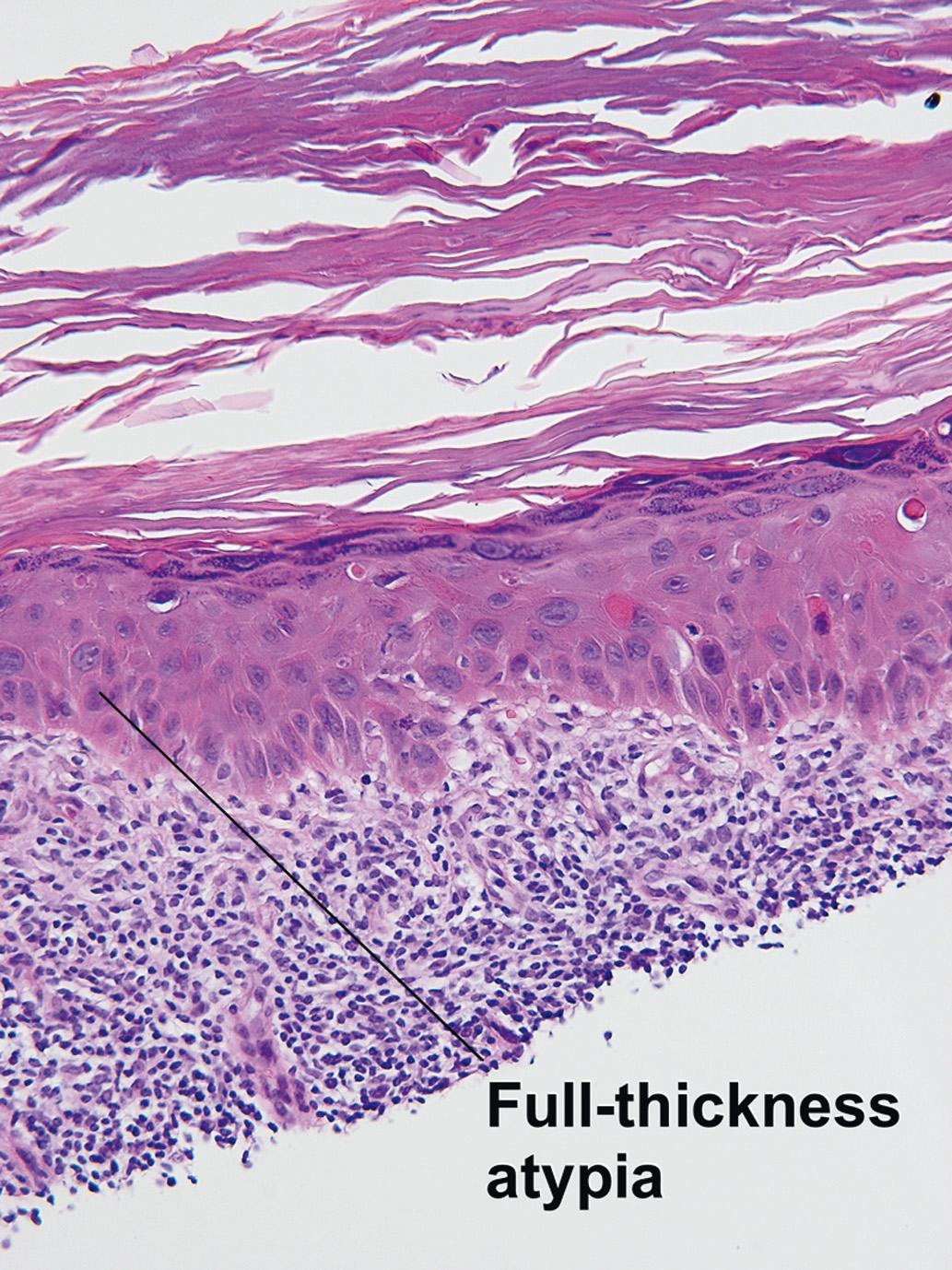
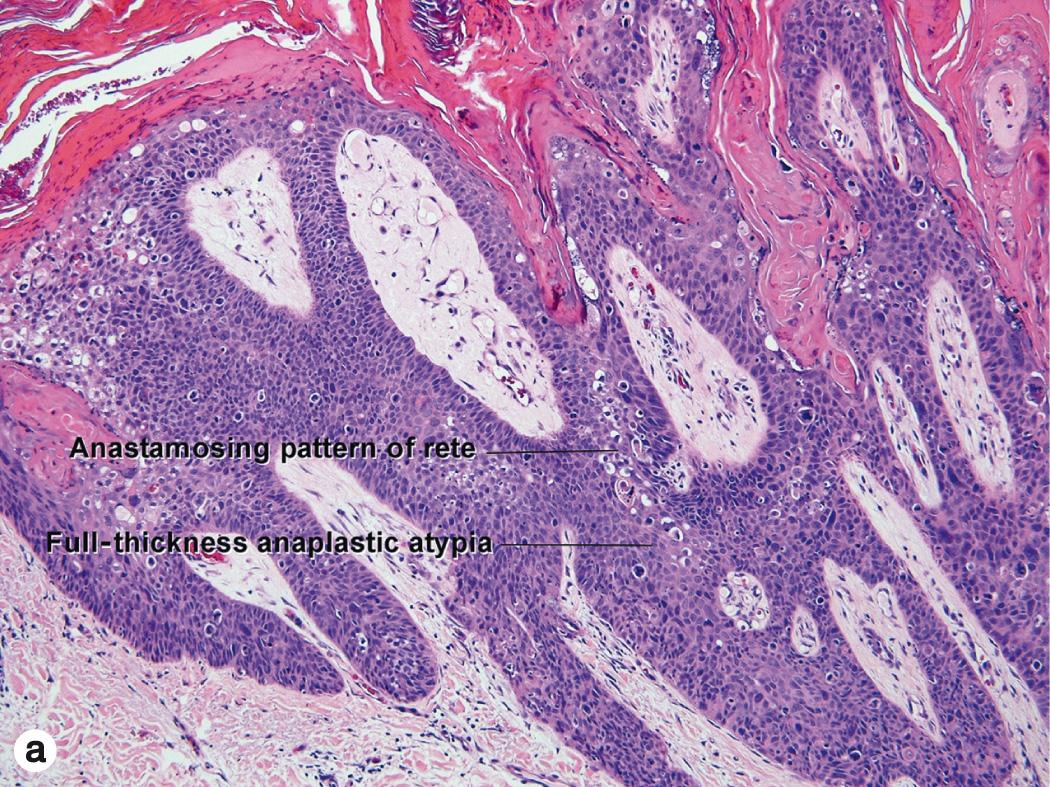
Full-thickness atypia with loss of normal maturation (wind-blown pattern)
Malignant horn typically present
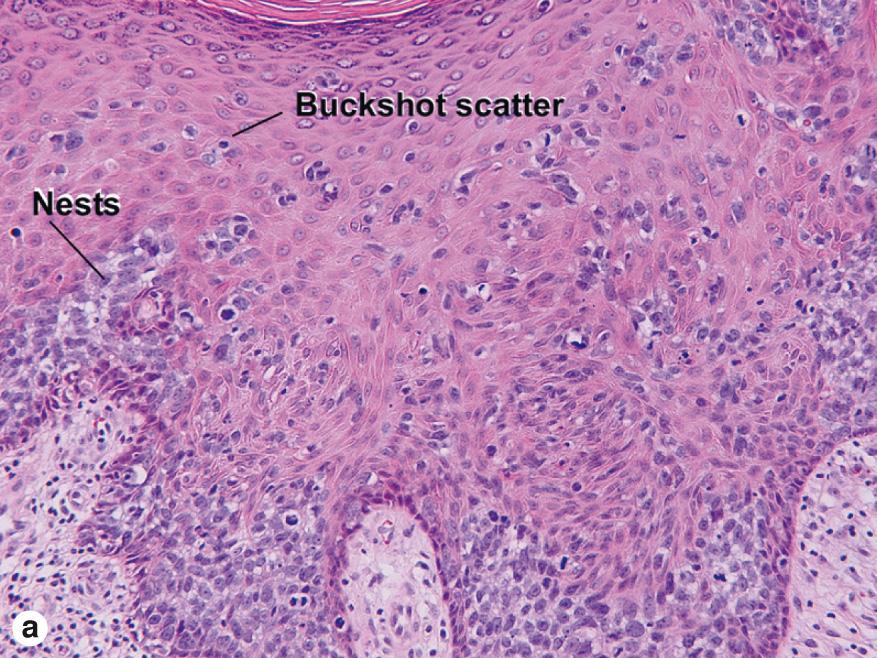
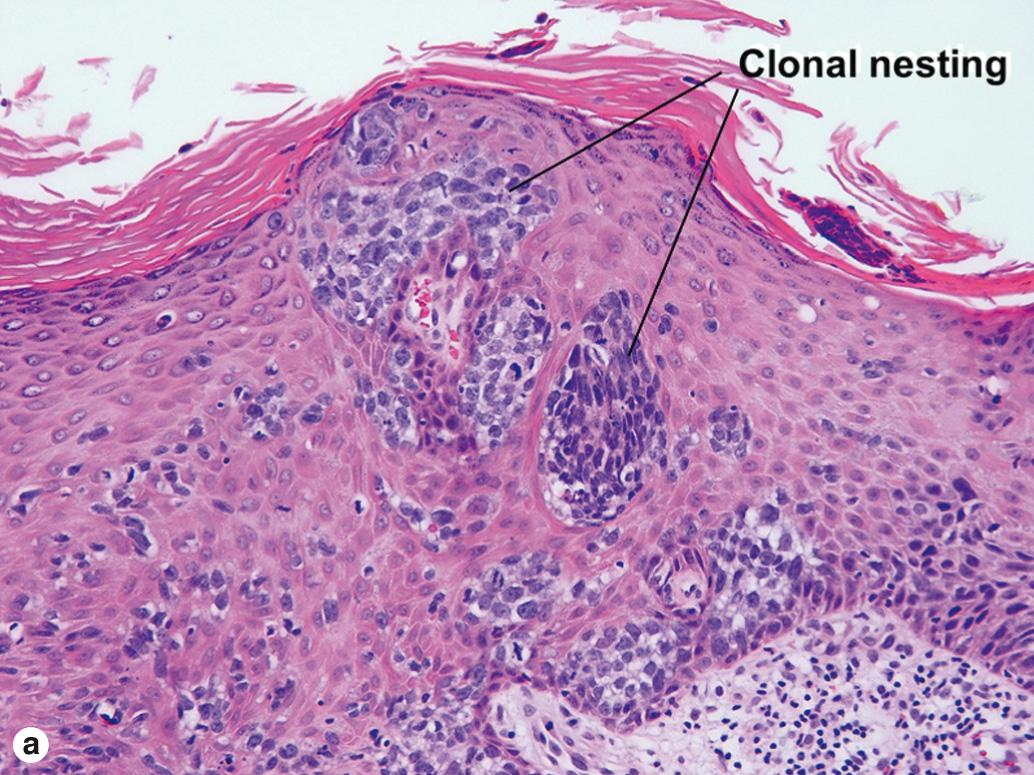
Atypical cells may occur in an intraepidermal buckshot or nested pattern
Full-thickness atypia commonly involves follicles
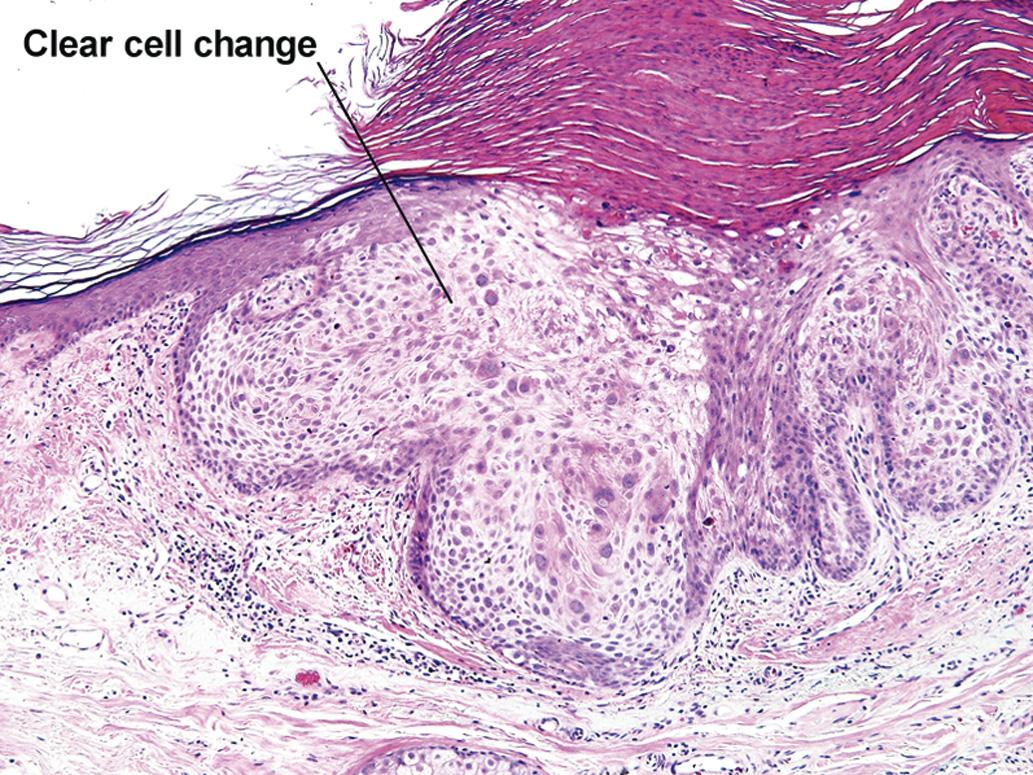
Bowen disease is a form of squamous cell carcinoma in situ. The malignant cells probably originate in the follicular epithelium. As the malignant cells migrate into the epidermis, they create a buckshot or nested pattern. With time, they involve the full thickness of the epidermis. This is the stage most commonly represented in biopsy specimens. It resembles bowenoid actinic keratosis, except that the cells tend to be more anaplastic with a higher nuclear-to-cytoplasm ratio. Areas with a nested or buckshot pattern may persist. Clear cell change or cells with ample glassy eosinophilic cytoplasm may sometimes be present instead of anaplastic cells. Bowen disease tends to involve the full thickness of at least some follicles. Some examples show full-thickness involvement of multiple follicles with relative sparing of the overlying epidermis.
Paget disease
Melanoma
Intraepidermal porocarcinoma
Sebaceous carcinoma
The malignant keratinocytes of Bowen disease can keratinize and become part of the stratum corneum. In contrast, the malignant cells of Paget disease or melanoma often “spit out” into the stratum corneum intact. Bowen disease contains glycogen and is periodic acid–Schiff (PAS) positive and diastase sensitive. In contrast, Paget disease contains sialomucin and is PAS positive, diastase resistant. Bowen disease is negative for carcinoembryonic antigen (CEA), whereas Paget stains for CEA. Ducts and sebaceous differentiation distinguish porocarcinoma and sebaceous carcinoma.
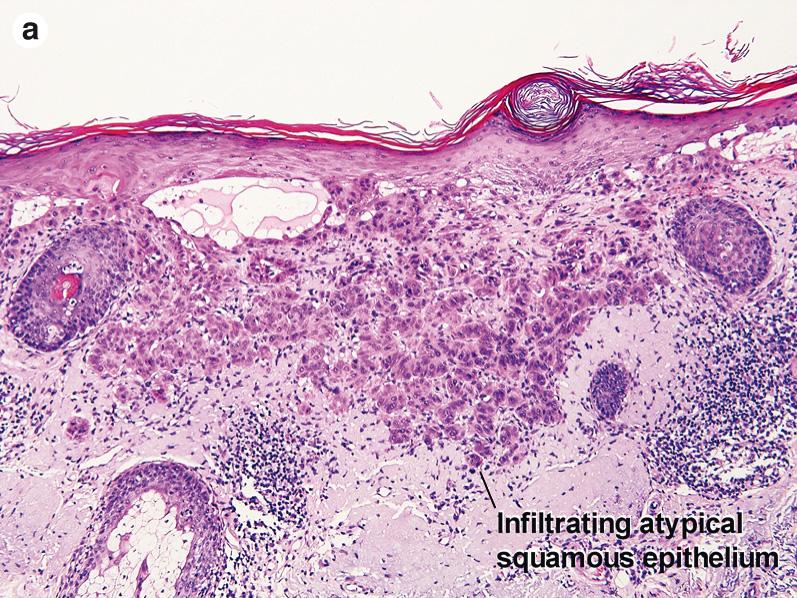
Atypical keratinocytes invading the dermis
Acantholysis may be present
Desmoplasia may be present
Well-differentiated invasive squamous cell carcinoma closely resembles the surface epidermis in staining characteristics, and keratinization is present. Pseudoepitheliomatous hyperplasia is often noted at the periphery of the tumor, and overlying changes of prurigo nodularis may be present in lesions that have been picked. An adequate biopsy is essential to avoid misdiagnosis.
Nodular lymphoid aggregates are an important clue to the presence of desmoplastic squamous carcinoma. Immunostaining can be used to confirm the presence of atypical squamous cells within the stroma.
Moderately differentiated tumors have a higher nuclear/cytoplastic ratio, but still keratinize. Poorly differentiated tumors are spindled or anaplastic. Keratin immunostaining is typically necessary to confirm the diagnosis of a poorly differentiated tumor.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here