Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
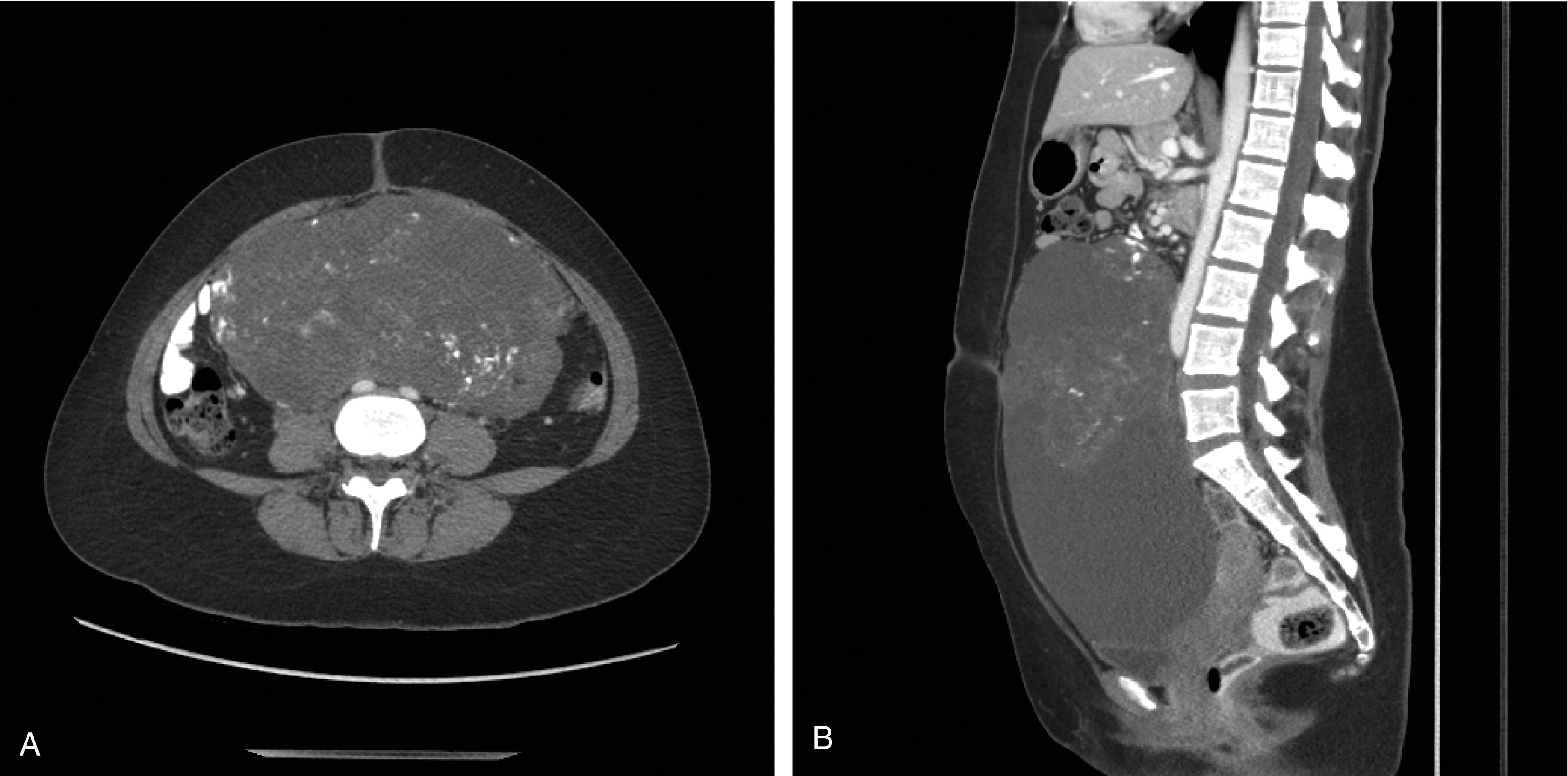
A 22-year-old G0 presents to an emergency department with pain and vomiting. CT scan of the abdomen/pelvis reveals a complex mass with cystic and solid components, including scattered calcifications, which occupies a large portion of the abdomen and pelvis and measuring up to 24 cm ( Fig. 1.1 ). There is also a small amount of pelvic fluid and an enlarged paraaortic lymph node in the aortocaval region measuring 1.5 × 0.8 cm. Tumor markers were drawn and are as follows: CA-125 127; Inhibin A 9.8; Inhibin B 27; Beta-hCG 3.4; AFP 3506; LDH 200. The patient undergoes an exploratory laparotomy, right salpingo-oophorectomy (RSO) with omentectomy, right paraaortic lymphadenectomy, and pelvic peritonectomy with no gross residual disease. Final pathology reveals a mixed ovarian germ cell tumor [20% high-grade immature teratoma (IT); 20% yolk sac tumor (YST); 60% mature teratoma] with metastatic YST in 1 paraaortic node and in a cul-de-sac nodule. How would you now manage this patient?
Malignant ovarian germ cell tumors (MOGTs) are overall rare, accounting for only 3%–5% of ovarian cancers. Additionally, the incidence of germ cell tumors varies greatly depending on age. The incidence of MOGTs rises steadily in young girls from age 9 to peak in the late teens between the ages of 15 and 19. This incidence then steadily declines after that, and malignant germ cell tumors are extremely rare after age 40. A SEER database study identified 2451 women with MOGTs between 1978 and 2010. The median age at diagnosis was 22 years old, and 93% of the women were under age 40 at diagnosis. Germ cell tumors make up 75% of ovarian cancers in women less than 20 years old but less than 5% of ovarian cancers in adult women. The most common germ cell tumors are benign mature cystic teratomas which can account for 20% of all ovarian tumors. When looking specifically at malignant germ cell tumors, the most common histologies are dysgerminoma, IT, and YST ( Table 1.1 ). Rarer histologies are mixed tumors, embryonal carcinomas, and nongestational choriocarcinomas.
| Histology | Percent of malignant ovarian germ cell tumors |
|---|---|
| Dysgerminoma | 33% |
| Immature teratoma | 36% |
| Yolk sac tumor | 15% |
| Mixed germ cell tumor | 5% |
| Embryonal carcinoma | 4% |
| Choriocarcinoma | 2% |
A major risk factor for development of germ cell tumors is gonadal dysgenesis. Swyer syndrome is a condition in which a woman or girl is phenotypically female but has a 46XY karyotype. These patients generally have intraabdominal streak gonads. There can be an up to a 30% risk of development of germ cell tumors such as gonadoblastoma and dysgerminoma with a much smaller risk of a mixed germ cell tumor. More rarely, germ cell tumors have been described in women with Turner syndrome (45X) and mosaicism which can lead to gonadal dysgenesis. These women appear to be at risk of gonadoblastomas and dysgerminomas, but dysgerminomas are very rare compared to gonadoblastomas, which have a generally benign course. MOGTs have no relation to hereditary cancer syndromes, such as BRCA or Lynch syndrome. The only other risk factor may be geographic location. There seems to be an increased risk for development of MOGTs in southeast Asian countries, especially in adolescent girls. The exact mechanism for this, genetic or environmental, is not clear.
Dysgerminomas are usually large (~ 15 cm) and have a fleshy, yellow, solid and lobulated appearance. Areas of cystic degeneration, hemorrhage, and necrosis may also be seen. Calcification may indicate the presence of a gonadoblastoma. Bilateral ovarian involvement occurs in relatively small proportion of cases.
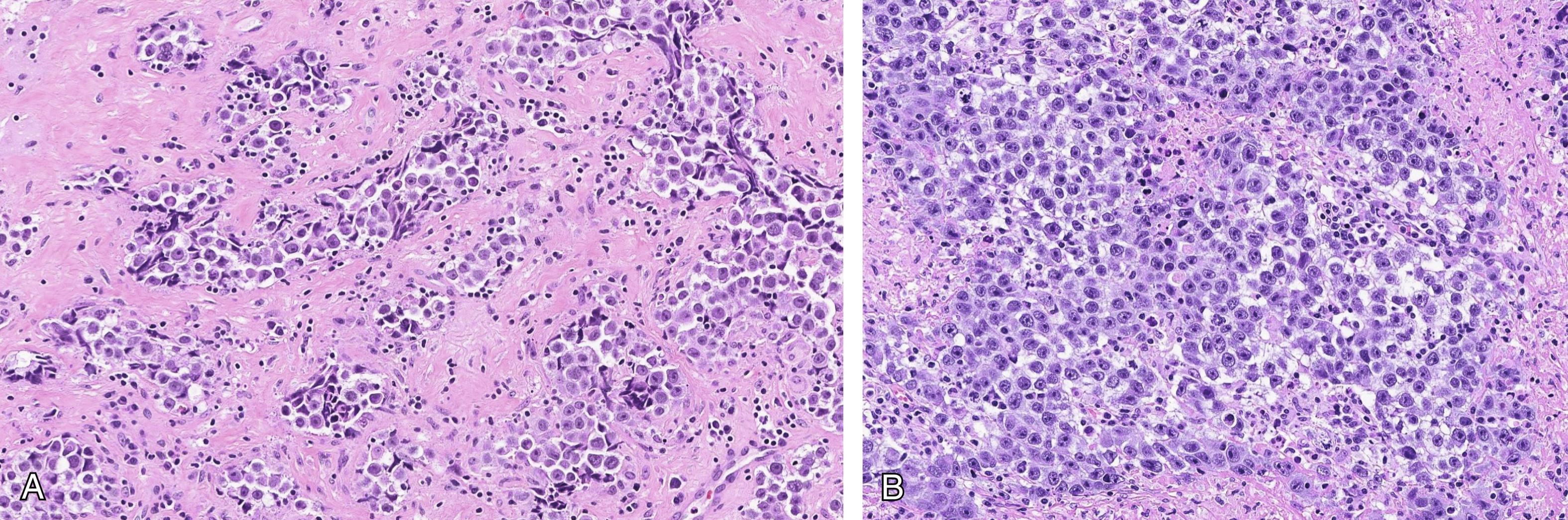
Dysgerminomas are histologically characterized by sheets, nests, and cords/trabeculae of tumor cells with intervening lymphocyte-rich fibrous septae ( Fig. 1.2 A and B). Poorly formed granulomas may be present in the surrounding stroma. The tumor cells are monotonous with clear or eosinophilic cytoplasm, well-defined cell borders, and a central nucleus with one or two macronucleoli. Mitotic figures are often conspicuous. Scattered syncytiotrophoblastic cells may be found in a minority of tumors. When seen in cytologic preparations, dysgerminomas classically show a “tigroid” background.
Immunohistochemical markers of dysgerminoma include SALL4, OCT4, c-kit (CD117), D2-40, and PLAP. They may exhibit focal staining for cytokeratins, and hCG could be used to highlight syncytiotrophoblastic cells, if present. Dysgerminomas are negative for EMA, AFP, Glypican-3, and CD30.
The morphological differential diagnosis for dysgerminoma includes other germ cell tumors (YST, embryonal carcinoma, and mixed germ cell tumor), epithelial primary ovarian tumors (clear cell carcinoma, undifferentiated carcinoma), and metastatic/secondary tumors involving the ovary (melanoma, lymphoma). Dysgerminomas, especially when large, must be well sampled to exclude other mixed germ cell components such as YST or embryonal carcinoma. YSTs have variable architecture with papillary, glandular, reticular, and solid patterns, unlike dysgerminomas that are usually solid and monotonous. Immunostains such as AFP and glypican-3 are positive in the former, and OCT4 and CD117 will be positive in the latter. Embryonal carcinoma has higher-grade nuclei and is positive for CD30. Clear cell carcinoma can be particularly challenging on morphology, but markers such as PAX8 and napsin-A (positive in CCC), and SALL4 (positive in dysgerminoma) will help in the differential. Lymphomas and melanomas are distinguished from dysgerminoma using characteristic immunostains of these entities. Distinction between the above entities at the time of intraoperative consultation can be particularly challenging.
Chromosome 12 amplification or isochromosome 12p is present in 80% of dysgerminomas, and KIT mutation or amplification is present in 30%–50% of cases.
YSTs are usually unilateral, large (> 10 cm), solid and cystic. The external surface is usually smooth. The solid cut surface has a tan yellow appearance, frequently with areas of hemorrhage and necrosis. The polyvesicular vitelline areas may grossly have a spongy/honeycomb-like appearance.
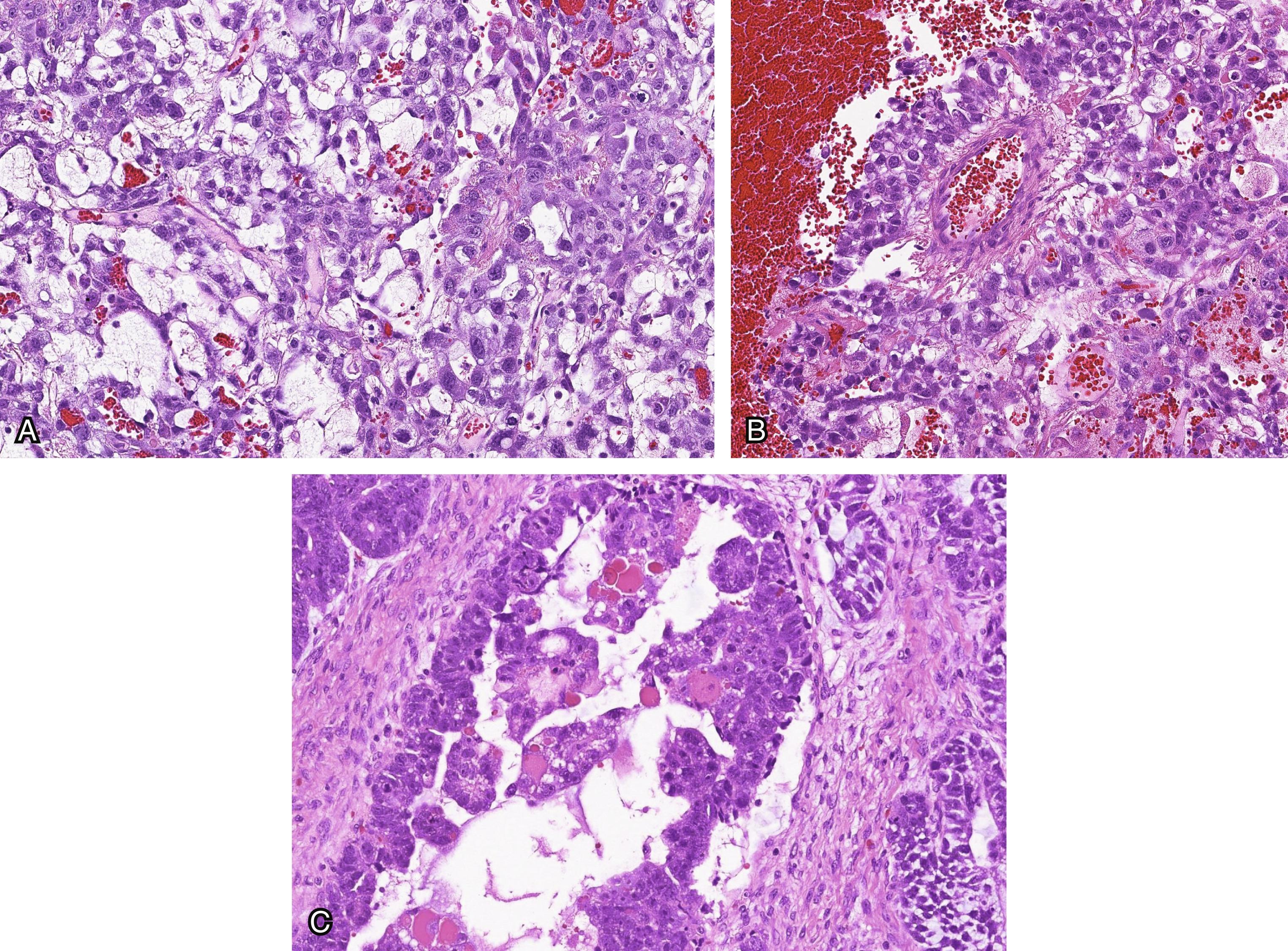
There is considerable heterogeneity in the histologic appearance of YST and a number of architectural patterns have been described including microcystic/reticular (most common), ( Fig. 1.3 A) endodermal sinus (with Schiller–Duval bodies), polyvesicular-vitelline, glandular, papillary, solid, and others. Schiller–Duval bodies ( Fig. 1.3 B) are characterized by the presence of a cystic space that envelops a central papillary structure with a fibrovascular core that is lined by a layer of tumor cells. The tumor cells usually exhibit clear cytoplasm and large nuclei with prominent nucleoli. Hyaline globules are often present ( Fig. 1.3 C).
Immunohistochemical markers of YST include SALL4, AFP, Glypican-3, CDX2 (in tumors with intestinal differentiation), HepPar-1 (in tumors with hepatoid differentiation) and TTF1 (in tumors with foregut/respiratory differentiation). YSTs are negative for EMA, CK7, ER, PR, OCT4, D2-40, and CD30.
Given the extraordinary morphologic variability that YSTs may exhibit, depending on the morphologic appearance of the tumor, the differential diagnosis is quite broad. In addition to other germ cell tumors (dysgerminoma and embryonal carcinoma, in particular), clear cell carcinoma and endometrioid carcinoma can also share significant morphologic overlap with YST. Clear cell carcinomas and YSTs can have papillary, glandular and solid patterns with cytoplasmic clearing. Immunostains such as CK7, napsin-A and above described markers of YST will allow the distinction. YST can have a prominent glandular pattern mimicking endometrioid carcinoma. The presence of squamous morules and lower grade cytology in conjunction with positive staining for PAX8 and hormone receptors (ER and PR) will confirm endometrioid carcinoma. Other tumors that may enter into the differential diagnosis include Sertoli–Leydig cell tumor (intermediate or poor differentiation) or the rare hepatoid carcinoma (which resembles hepatocellular carcinoma). Somatically derived YSTs are admixed with an epithelial tumor and can be difficult to diagnose. Subtle histologic features typical of YST must be looked for to make the correct diagnosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here