Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Lymph nodes are important. A methodical search may yield invaluable clues in cancer or systemic disease. Some “sentinel” nodes have even entered medical folklore, forever linked by eponyms to the physicians who first described them.
Which nodes are normally palpable in the healthy individual?
Out of a total of 600, only the submandibular, axillary , or inguinal nodes may at times be felt. Examiner’s skill is, of course, paramount, usually improving with time.
What is lymphadenopathy?
The presence of abnormal nodes because of size, consistency, or number. Adenopathy can occur in various conditions, affecting individuals of any age, and with or without symptoms. It may be happenstance (as incidental detection by the physician or patient during routine exam) or the first sign of malignancy, the presenting manifestation of a complex systemic disorder, or a self-limited finding. The differential diagnosis is always challenging.
How many adenopathies turn out to be “bad”?
Difficult to say, since data are scarce. In a Dutch study of 2556 patients presenting with unexplained lymph nodal enlargement to a primary care office, 10% were eventually referred to subspecialists, and 3.2% ultimately underwent biopsy. Only 29/2556 (1.1%) had a final diagnosis of malignancy. This low prevalence was confirmed by two separate US studies, suggesting that the much higher neoplastic prevalence of 40%–60% reported by many textbooks refers only to the 3% who underwent biopsy, thus grossly overestimating the likelihood of cancer. Hence, in primary care settings, unexplained adenopathy has a neoplastic risk of only 4% in patients 40 years or older and 0.4% in those younger than 40.
What is the first approach to adenopathy?
To sort out “serious” from benign. To do so, first separate generalized from localized , since these are distinct conditions with unique differential diagnoses.
What is a generalized adenopathy?
One that involves two or more noncontiguous sites (conversely, a localized adenopathy is one that involves only one site). Always make sure that the “localized” ones are not instead part of a generalized process. This may not be necessarily self-evident, since only 17% of all generalized adenopathies are correctly identified by primary care physicians. Hence, whenever you find an abnormal site, always evaluate all others.
Where should you look for enlarged nodes?
Submandibular and submental areas
Anterior and posterior cervical regions
Supraclavicular fossa
Axilla
Epitrochlear space
Inguinal/femoral sites
Important nodes also can be found in the popliteal fossa and paraumbilical region. Deeper ones (hilar, mediastinal, abdominal, and pelvic) are important, too, but inaccessible.
Which parts of the exam should be emphasized in cases of generalized adenopathy?
Those that may uncover signs of systemic disease , such as skin rash, mucous membrane lesions, hepatomegaly, splenomegaly, and arthritis.
What is the differential diagnosis of a generalized adenopathy?
One of three processes: (1) a disseminated malignancy , especially hematologic (lymphomas, leukemias, and angioimmunoblastic lymphadenopathy); (2) a collagen vascular disorder (sarcoidosis, rheumatoid arthritis [RA], and systemic lupus erythematosus [SLE]); or (3) an infectious process (mononucleosis, cytomegalovirus [CMV], acquired immunodeficiency syndrome (AIDS), toxoplasmosis, syphilis, tuberculosis (TB), histoplasmosis, coccidioidomycosis, brucellosis, and bubonic plague). Drug reactions can do it too as can intravenous drug abuse. Some medications (e.g., phenytoin) specifically cause lymphadenopathy; others (e.g., cephalosporins, penicillins, or sulfonamides) do it instead in the context of a serum sickness-like syndrome, with fever, arthralgias, and skin rash ( Table 16.1 ).
| Allopurinol (Zyloprim) | Penicillin |
| Atenolol (Tenormin) | Phenytoin (Dilantin) |
| Captopril (Capozide) | Primidone (Mysoline) |
| Carbamazepine (Tegretol) | Pyrimethamine (Daraprim) |
| Cephalosporins | Quinidine |
| Gold | Sulfonamides |
| Hydralazine (Apresoline) | Sulindac (Clinoril) |
Should a biopsy be done in patients with generalized lymphadenopathy?
Yes, especially considering the often serious (and systemic) character of the condition. Remember to always biopsy the largest node. If nodes are of similar size, choose in descending order: the supraclavicular, cervical, axillary, epitrochlear, and inguinal stations. The latter is the least helpful, since it often shows only reactive hyperplasia. Yet, do not disregard it. In one retrospective study (with careful patient selection), 53% of inguinal biopsies turned out to be diagnostic. Also, beware that some sites may be more prone to surgical complications than others. Sampling the parotid area, for example, can damage the facial nerve or its branches, while biopsying the posterior cervical triangle may injure the spinal accessory nerve.
Which is more common, localized or generalized adenopathy?
Localized. In a primary care setting, 75% of patients will present with localized involvement (head and neck, 55%; supraclavicular, 1%; axillary, 5%; inguinal, 14%).
Can the region of involvement narrow the diagnosis?
Yes. As in real estate, location is very important for nodes (as applied, of course, to regional or localized adenopathies). For the generalized form, differential diagnosis is another ballgame). Overall, regional adenopathy reflects localized infection or neoplasm. For instance, cat-scratch disease for cervical or axillary nodes, sexually transmitted diseases for the inguinal ones , and infectious mono for the cervical station. Finally, preauricular nodes (of any size) are usually more significant than similarly sized nodes in other locations.
Should one know the regions drained by the various lymphonodal stations?
Yes, since this may unlock the underlying cause. After detecting an enlarged node, always examine the region drained by it ( Table 16.2 ). Look for infections, skin lesions, or tumors.
| LOCATION | LYMPHATIC DRAINAGE | CAUSES |
|---|---|---|
| Submental | Lower lip, anterior floor of mouth, tip of tongue, skin of cheek, teeth, nose | Mononucleosis-like syndromes, Epstein-Barr virus, CMV, toxoplasmosis |
| Submandibular | Tongue, submaxillary gland, lips and mouth, conjunctivae | Infections of head, neck, sinuses, ears, eyes, scalp, pharynx |
| Anterior cervical (jugular) | Tongue, tonsil, pinna, parotid, larynx, thyroid, upper esophagus | Pharyngitis organisms, rubella, upper respiratory infections, cancer of tongue, larynx, thyroid and cervical esophagus |
| Posterior cervical | Scalp and neck, middle ear, skin of arms and pectorals, thorax, cervical and axillary nodes | Mononucleosis, toxoplasmosis, tuberculosis, rubella, otitis media, scalp infections and dandruff, Kikuchi’s disease, lymphoma, head and neck malignancy |
| Preauricular | Eyelids and conjunctivae, temporal region, pinna | Disease external auditory canal, ipsilateral conjunctivitis (Parinaud’s syndrome), lymphoma |
| Postauricular | External auditory meatus, pinna, scalp | Local infection, but also rubella |
| Occipital | Scalp and head | Local infection |
| Right supraclavicular node | Breast, lungs, esophagus mediastinum | Lung, breast, mediastinum |
| Left supraclavicular node | Breast, lungs, abdomen via thoracic duct, and pelvis | Lymphoma, thoracic, retroperitoneal, gastrointestinal or pelvic cancer, bacterial or fungal infection |
| Axillary | Arm, thoracic wall, breast | Arm infections, cat-scratch disease, tularemia, lymphoma, breast cancer, silicone implants, brucellosis, melanoma |
| Epitrochlear | Ulnar aspect of forearm and hand | Infections, lymphoma, sarcoidosis and connective tissue diseases, tularemia, secondary syphilis, leprosy, leishmaniasis, rubella |
| Inguinal | Penis, scrotum, vulva, vagina, perineum, gluteal region, lower abdominal wall, lower anal canal, extremities (benign reactive in shoeless walkers) | Infections of the leg or foot, STDs (e.g., herpes simplex virus, gonococcal infection, syphilis, chancroid, granuloma inguinale, lymphogranuloma venereum), lymphoma, pelvic malignancy, bubonic plague |
What are the general characteristics that can help interpret an abnormal node?
The mnemonic is ALL AGES :
A = A ge of patient
L = L ocation of the abnormal nodes
L = L ength of time the nodes have been present
A = A ssociated signs or symptoms, whether local or extranodal
G =Presence or absence of g eneralized lymphadenopathy
E = E xtranodal associations
S =Presence or absence of s plenomegaly and/or fever
Why does the patient’s age help?
Because it is the most important predictor of malignancy. Although lymphoproliferative disorders also may affect younger individuals, neoplastic nodes are usually more common in those older than 40 years ( Table 16.3 ). Yet some malignant-looking nodes may actually be benign. Infectious mononucleosis, for example, may often resemble Hodgkin’s disease.
| BENIGN | CARCINOMA | LYMPHOMA | |
|---|---|---|---|
| Nodes | |||
| All (n=925) | 60 | 28 | 12 |
| Abdominal (n=51) | 63 | 33 | 4 |
| Thoracic (n=149) | 73 | 26 | 1 |
| Peripheral (n=653) | 56 | 29 | 15 |
| Unspecified (n=72) | 61 | 25 | 14 |
| Ages a | |||
| All | 57 | 28 | 15 |
| <30 | 79 | 6 | 15 |
| 31–50 | 59 | 30 | 11 |
| 51–80 | 40 | 44 | 16 |
a Age distribution based on 628 patients with peripheral lymph node biopsies.
What about associated signs and symptoms?
They can be “local” or systemic ( Table 16.4 ). Local findings suggest infection or neoplasm in a specific site (like the swollen nodes and lymphangitic streaks of a skin infection). Conversely, systemic symptoms (such as fever, fatigue, night sweats, and unexplained weight loss) argue in favor of a collagen vascular, lymphoproliferative, or infectious disorder (e.g., TB). Still, lack of associated signs or symptoms does not exclude malignancy and thus should not stop a workup. Finally, remember that the adenopathy of Hodgkin’s disease may become painful after alcohol ingestion.
| DISORDER | ASSOCIATED FINGINGS |
|---|---|
| Common Causes of Lymphadenopathy | |
| Mononucleosis-type syndromes | Fatigue, malaise, fever, atypical lymphocytosis |
| Epstein-Barr virus a | Splenomegaly in 50% |
| Toxoplasmosis a | 80%–90% asymptomatic |
| Cytomegalovirus a | Often mild symptoms; patients may have hepatitis |
| Initial stages of HIV infection a | “Flu-like” illness, rash |
| Cat-scratch disease | Fever in 30%; cervical or axillary nodes |
| Pharyngitis (group A Streptococcus , gonococcus) | Fever, pharyngeal exudates, cervical nodes |
| Tuberculosis lymphadenitis a | Painless, matted cervical nodes |
| Secondary syphilis a | Rash |
| Hepatitis B a | Fever, nausea, vomiting, icterus |
| Lymphogranuloma venereum | Tender, matted inguinal nodes |
| Chancroid | Painful ulcer, painful inguinal nodes |
| Lupus erythematosus a | Arthritis, rash, serositis; renal, neurologic, hematologic disorders |
| Rheumatoid arthritis a | Arthritis |
| Lymphoma a | Fever, night sweats, weight loss in 20%–30% |
| Leukemia a | Blood dyscrasias, bruising |
| Serum sickness a | Fever, malaise, arthralgia, urticaria; exposure to antisera or medications |
| Sarcoidosis | Hilar nodes, skin lesions, dyspnea |
| Kawasaki disease a | Fever, conjunctivitis, rash, mucosal lesions |
| Less Common Causes of Lymphadenopathy | |
| Lyme disease a | Rash, arthritis |
| Measles a | Fever, conjunctivitis, rash, cough |
| Rubella a | Rash |
| Tularemia a | Fever, ulcer at inoculation site |
| Brucellosis a | Fever, sweats, malaise |
| Plague | Febrile, acutely ill with cluster of tender nodes |
| Typhoid fever a | Fever, chills, headache, abdominal complaints |
| Still’s disease a | Fever, rash, arthritis |
| Dermatomyositis a | Proximal weakness, skin changes |
| Amyloidosis a | Fatigue, weight loss |
What about splenomegaly ?
It occurs in only 5% of adenopathies, and when it does it argues in favor of sarcoidosis, acute leukemia, chronic lymphocytic leukemia (CLL), Hodgkin/non-Hodgkin lymphoma, or a mononucleosis-like syndrome. It is instead uncommon in metastatic cancer.
What about fever?
It usually suggests infection or lymphoma. Still, the differential diagnosis can be quite wide, since many infectious processes may present with febrile adenopathy (TB, mononucleosis, toxoplasmosis, histoplasmosis, salmonellosis, AIDS, CMV, syphilis, and subacute bacterial endocarditis). Many cancers can do it, too (CLL, Waldenström’s, multiple myeloma, and Kaposi’s sarcoma), and so can systemic disorders (sarcoid, SLE, RA, Kawasaki, and Whipple disease).
Are there any epidemiologic clues that might narrow the differential diagnosis?
Yes. Occupational exposure, recent travel, or high-risk behavior may all contribute ( Table 16.5 ).
| EXPOSURE | DIAGNOSIS |
|---|---|
| General | |
| Cat | Cat-scratch disease, toxoplasmosis |
| Undercooked meat | Toxoplasmosis |
| Tick bite | Lyme disease, tularemia |
| Tuberculosis | Tuberculous adenitis |
| Recent blood transfusion or transplant | Cytomegalovirus, HIV |
| High-risk sexual behavior | HIV, syphilis, herpes simplex virus, cytomegalovirus, hepatitis B infection |
| Intravenous drug use | HIV, endocarditis, hepatitis B infection |
| Occupational | |
| Hunters, trappers | Tularemia |
| Fishermen, fishmongers, slaughterhouse workers | Erysipeloid |
| Travel-related | |
| Arizona, southern California, New Mexico, western Texas | Coccidioidomycosis |
| Southwestern United States | Bubonic plague |
| Southeastern or central United States | Histoplasmosis |
| Southeast Asia, India, Central or West Africa | Scrub typhus |
| Central or West Africa | African trypanosomiasis (sleeping sickness) |
| Central or South America | American trypanosomiasis (Chagas’ disease) |
| East Africa, Mediterranean, China, Latin America | Kala-azar (leishmaniasis) |
| Mexico, Peru, Chile, India, Pakistan, Egypt, Indonesia | Typhoid fever |
Which node characteristics can be clinically helpful?
In addition to location , six features may help the diagnosis:
Size: this is easily measured by a plastic caliper or ruler. It can predict its nature and guide biopsy. Although there is no “normal” size (since this depends on age and background antigenic exposure), some authors have defined the upper limits of normal as a node >1 cm that has been present outside the inguinal region for more than 1 month. Yet, inguinal nodes can be normal up to 1.5 cm, whereas preauricular and epitrochlear nodes are suspicious even if 0.5–1 cm. Moreover, large but benign nodes are quite common in IV drug users. In fact, some authors have even suggested raising the threshold of suspicion to 1.5 × 1.5 cm. Finally, although no specific diagnosis can be based on size, some valuable predictions can be inferred. For example, in 213 adults with unexplained lymphadenopathy, nodes <1 cm were never neoplastic. Conversely, cancer was the final diagnosis in 8% of 1–1.5 cm nodes and 38% of >1.5 cm. In children, nodes >2 cm (along with an abnormal chest x-ray and absence of ear, nose, and throat symptoms) argue in favor of granulomatous diseases (TB, cat-scratch disease, sarcoid) or cancer (mostly lymphomas).
Duration: the longer the node has been present, the less its risk of being neoplastic or granulomatous. Still, lymphomatous nodes can regress, albeit temporarily.
Consistency: soft nodes are usually infectious or inflammatory, whereas rock-hard ones tend to be neoplastic, often metastatic. Exceptions include the nodes of Hodgkin’s, which are firm but rubbery. Fluctuant nodes reflect instead bacterial lymphadenitis with necrosis. They feel like a tense balloon or grape, are typically tender, and may even fistulize through the skin, forming open sinuses that are a common feature in TB. Nodes of this type, especially in groins or axillae, are often referred to as buboes (from the Greek term for swollen groin) and used to be typical of infectious processes, such as gonorrhea, syphilis, TB, and, of course, the “bubonic” plague of old.
Matting: fusion into a scalloped mass transforms individual nodes into large conglomerates. This is usually a neoplastic feature (metastatic carcinoma or lymphomas), but also can occur in inflammatory processes (like sarcoid) and chronic infections (like TB and lymphogranuloma venereum).
Relationship to surrounding tissues: adherence to overlying skin, subjacent tissues, or both does not separate inflammation from neoplasm but does exclude benignity.
Pain/tenderness: this reflects rapid growth with painful capsular stretching. It is a sign of suppurative inflammation but also may reflect hemorrhage into the necrotic center of a rapidly expanding neoplastic node. Hence, tenderness does not reliably differentiate benign from malignant ones. The same applies to sinus tract formation, which can occur in infections (actinomycosis and TB) as well as cancer.
Pearl : benign nodes tend to be small, soft, nontender, mobile, and discrete (well demarcated). Neoplastic nodes are large, nontender, matted, fixed, and rock-hard. Inflammatory nodes are tender, firm (but not rock-hard), occasionally fluctuant, and often matted and fixed.
What is the best way to deal with adenopathy?
Start with history and physical exam (H&P), since they can often identify the etiology (upper respiratory infection [URI], pharyngitis, periodontal disease, conjunctivitis, insect bites, focal infection, recent immunization, cat-scratch disease, tinea, or dermatitis), thus preempting the need for further workup.
H&P also can offer a presumptive diagnosis and guide the workup (Epstein-Barr virus [EBV], HIV, lymphoma, syphilis).
Once the initial evaluation is complete, some patients may still have either unexplained lymphadenopathy or a presumptive diagnosis unconfirmed by labs and clinical course. In this case, if the adenopathy is localized (and the clinical picture is reassuring [i.e., a benign history, an unremarkable exam, and no constitutional symptoms]), allow 3–4 weeks of observation before resorting to biopsy. If the clinical picture is instead worrisome (risk factors for malignancy, constitutional signs/symptoms) or the lymphadenopathy is generalized , do further testing and get a biopsy. Still, avoid biopsy in patients with probable viral illness, since their pathology may simulate lymphoma.
What is unexplained lymphadenopathy?
One that remains perplexing after initial evaluation. In this case, pursue a specific diagnosis based on the patient’s age, but also the nodes’ duration, characteristics, and location.
What is the differential diagnosis of an unexplained lymphadenopathy?
Usually infectious, neoplastic , or autoimmune – which also is the differential diagnosis for fever of unknown origin or an elevated sedimentation rate. A helpful mnemonic is CHICAGO :
C=C ancers: hematologic malignancies (Hodgkin’s disease, non-Hodgkin’s lymphoma, acute and chronic leukemia, Waldenström’s macroglobulinemia, multiple myeloma [uncommon], systemic mastocytosis) and metastatic “solid” tumors (breast, lung, renal cell, prostate, other)
H = H ypersensitivity syndromes: serum sickness, drug sensitivity (diphenylhydantoin, carbamazepine, primidone, gold, allopurinol, indomethacin, sulfonamides, others), silicone reaction, vaccination-related, and graft versus host disease
I = I nfections: viral (infectious mononucleosis [EBV], CMV, infectious hepatitis, postvaccinal lymphadenitis, adenovirus, herpes zoster, HIV/AIDS, human T-lymphocyte virus 1), bacterial (cutaneous infections [staphylococci, streptococci], cat-scratch fever, chancroid, melioidosis, TB, atypical mycobacteria, primary and secondary syphilis), chlamydial (lymphogranuloma venereum), protozoan (toxoplasmosis), mycotic (histoplasmosis, coccidioidomycosis), rickettsial (scrub typhus), helminthic (filariasis)
C = C onnective tissue disorders: RA, SLE, dermatomyositis, mixed connective tissue disease, Sjögren syndrome
A = A typical lymphoproliferative disorders: angiofollicular (giant) lymph node hyperplasia (Castleman disease), angioimmunoblastic lymphadenopathy with dysproteinemia, angiocentric immunoproliferative disorders, lymphomatoid granulomatosis, Wegener granulomatosis
G = G ranulomatous lesions: TB, histoplasmosis, mycobacterial infections, cryptococci, silicosis, berylliosis, cat-scratch fever
O = O ther unusual causes of lymphadenopathy: inflammatory pseudotumor of lymph nodes, histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis), sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease), vascular transformation of sinuses, progressive transformation of germinal centers
Which clinical presentations may help identify the cause of lymphadenopathy?
Mononucleosis-type syndromes: adenopathy plus fatigue, malaise, fever, and increased atypical lymphocyte count. Differential diagnosis includes EBV (mononucleosis), toxoplasmosis, CMV, streptococcal pharyngitis, hepatitis B, and acute HIV.
HIV infection: any persistent generalized lymphadenopathy (i.e., one of at least 3 months’ duration, involving two extrainguinal sites or more) should suggest an early stage of HIV infection. Generalized adenopathy in HIV suggests Kaposi, CMV, toxoplasmosis, TB, cryptococcosis, syphilis, and lymphoma.
Ulceroglandular syndrome: regional adenopathy plus skin lesions. The classic cause is tularemia, acquired by contact with an infected rabbit or tick. More common, however, are streptococcal infection (impetigo) and cat-scratch and Lyme diseases.
Oculoglandular syndrome: preauricular adenopathy with conjunctivitis. Common causes include viral keratoconjunctivitis and cat-scratch disease from ocular lesions.
How do you palpate cervical nodes?
By using the pads of your fingertips, the hands’ most sensitive parts. Examine both sides of the head and neck simultaneously , by sliding your fingers over the area of attention. Apply steady and gentle pressure. Explore all cervical sites by following the anterior and posterior aspects of the underside of the jaw and neck. Large nodes are often visibl e, presenting as localized skin bulging. Involvement of only one side of the neck makes these swellings even more visible.
What are the important head and neck stations?
There is a fair amount of variability and overlap in pathways of drainage ( Fig. 16.1 ). Overall, you should examine nodes in the following order:
Submental: just below the chin. They drain the teeth and intra-oral cavity.
Submandibular: along the underside of the jaw, on either side. They drain the structures in the posterior floor of the mouth.
Anterior cervical (both superficial and deep): also called “jugular chain nodes,” these lie on top of and beneath the sternocleidomastoid muscles (SCM) on either side of the neck, from the angle of the jaw to the top of the clavicle (the SCMs allow the head to rotate to the opposite side and can be easily identified by asking the patient to turn the head). They drain the internal structures of the throat as well as part of the posterior pharynx, tonsils, and thyroid gland.
Posterior cervical: also called “posterior triangle nodes,” these extend in a line posterior to the SCMs, but in front of the trapezius, from the mastoid bone to the clavicle. They drain the skin on the back of the head and are frequently enlarged during URIs (mononucleosis).
Tonsillar: just below the angle of the mandible. They drain the tonsillar and posterior pharyngeal regions.
Preauricular and postauricular: respectively, anterior and posterior to the ear. Swelling of the preauricular node in a setting of conjunctivitis-like “pink eye” represents Parinaud’s (oculoglandular) syndrome, occurring in various conditions, including tularemia and cat-scratch disease ( Bartonellosis ).
Occipital: common in childhood infections, but rare in adults – except in a setting of either banal scalp infection or, more ominously, generalized lymphadenopathy from systemic disease (HIV) .
Supraclavicular: in the hollow above the clavicle, just lateral to where it joins the sternum. They drain part of the thoracic cavity and abdomen (see Questions 31–36).
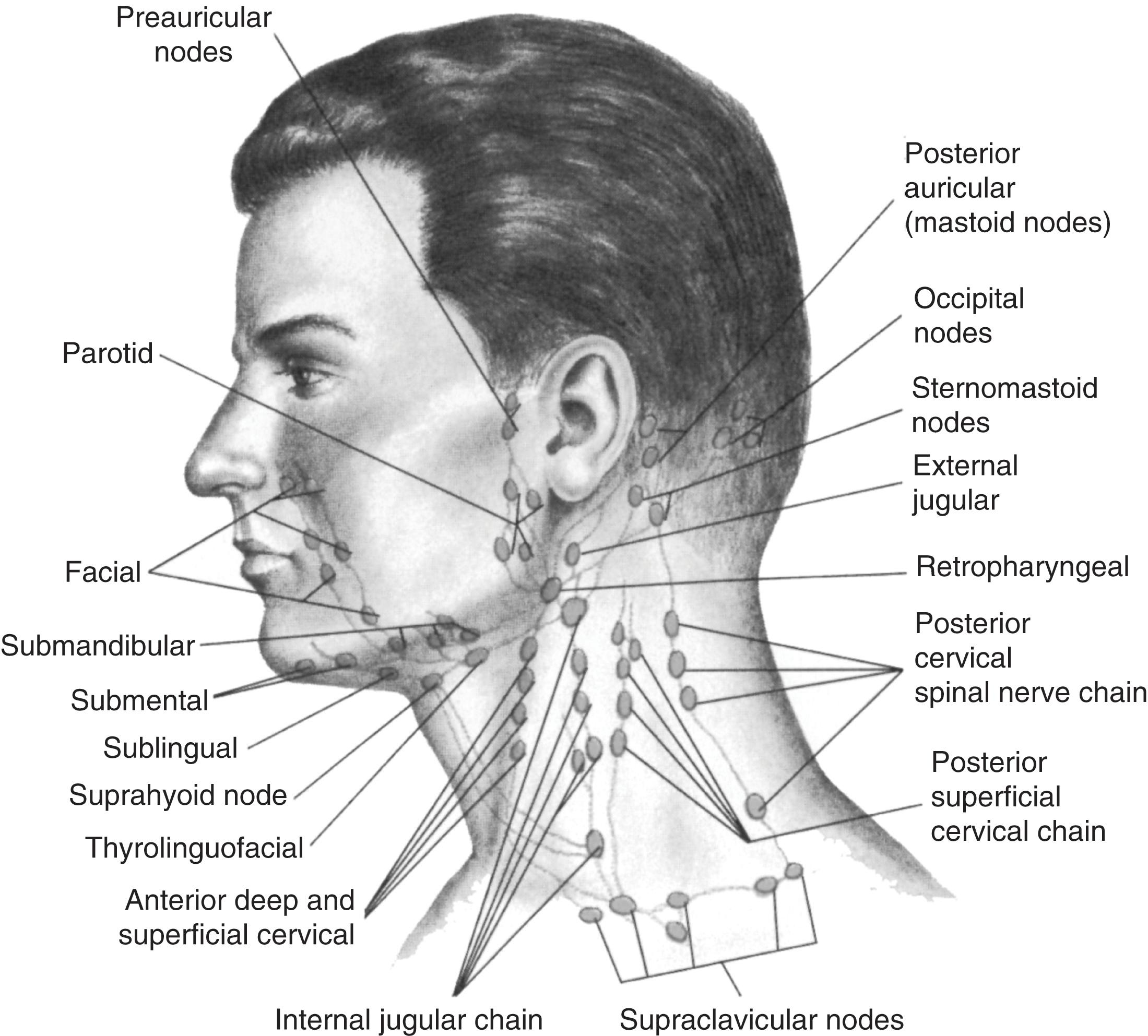
Palpation of other cervical groups also may be indicated in cases of disease affecting specific regions. For example, preauricular and postauricular nodes (just in front or behind the ears) may enlarge because of infections of the external ear canal.
And so, what is the overall significance of cervical lymphadenopathy?
It depends on location but may suggest either infection or malignancy .
Infections: bacterial pharyngitis, dental abscesses, otitis media or externa, infectious mono, gonococcal pharyngitis, CMV, HIV, TB, rubella, toxoplasmosis, hepatitis, and adenovirus
Malignancies: non-Hodgkin lymphoma, Hodgkin’s disease, and squamous cell carcinoma of the head and neck
Note that one of the processes responsible for isolated posterior cervical and occipital adenopathy is Kikuchi-Fujimoto disease (histiocytic necrotizing lymphadenitis). This is a syndrome of unknown etiology first described in 1972 in Japan. The classic patient is a young woman who presents with unilateral painless lymphadenopathy of the posterior cervical region, typically resolving in 3 months.
Can cervical nodes remain permanently enlarged after an infection?
Yes. In this case, they are rather small (<1 cm), never tender, and with a rubbery consistency. For example, small palpable nodes in the tonsillar submental and submandibular regions may often occur in otherwise healthy individuals, representing the sequelae of past pharyngitis or dental infections. Conversely, rock-hard nodes should always suggest malignancy, whose location depends on the site drained by the corresponding nodes.
What are “shotty” nodes?
They are small nodes that feel like shotgun pellets, or tiny peas. They are typically nontender, firm but not stony-hard, small but equal, mobile, round, and well demarcated. Usually found in the cervical chain of children with viral illnesses (with location reflecting the original site of infection), they may outlast the illness by several weeks and are usually of no clinical consequence. The expression “shotty” was commonly used in 19th-century lay language but is now quite obsolete—except, of course, for medical jargon.
What is scrofula?
An old term for cervical tuberculous lymphadenitis: swollen nodes that make the patient’s neck resemble that of a piglet ( scrofa , sow in Latin). Scrofula used to be very common in children, since it was spread by unpasteurized milk from infected cows. It was typically treated by the king’s touch , which consisted in having the children’s neck healed by the laying on of his/her majesty’s hands (usually of either England or France). This “cure,” of course, reflected the overall benign nature of the disease rather than the healing power of royalty. Note that chronic mycobacterial (or fungal) infections also can cause supraclavicular adenopathy.
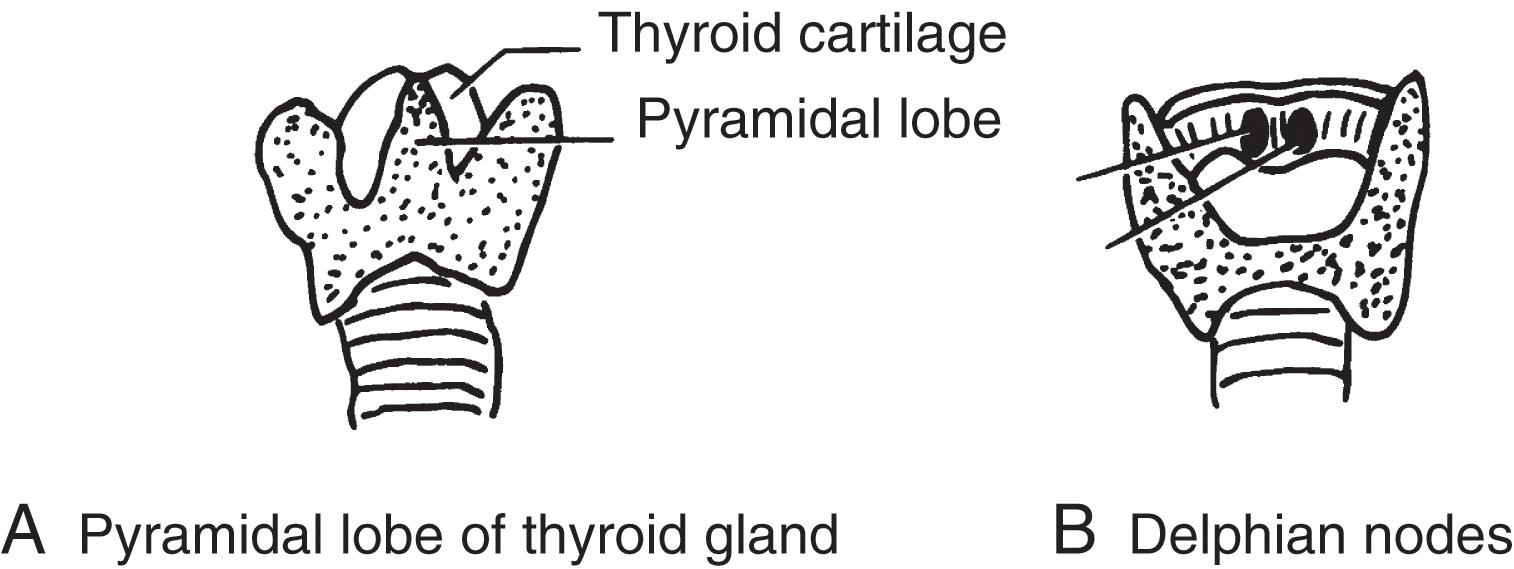
What are Delphian nodes?
A cluster of small and midline prelaryngeal nodes ( Fig. 16.2 ). These are typically located on the thyrohyoid membrane – just anterior to the cricothyroid ligament, and just above the thyroid isthmus. Given their pretracheal and superficial location, they are easily palpable if enlarged, even though at times they may be confused with the pyramidal lobe of the gland. They drain the thyroid and larynx , and like Delphi in ancient Greece, they have traditionally been considered an oracle – of thyroid disease or laryngeal malignancy (even though objective supportive data are lacking). They also are the first to be exposed during surgery, thus foretelling the nature of the underlying illness. Delphian nodes reflect a range of thyroid involvement, including subacute thyroiditis, Hashimoto’s, and thyroid cancer. If due to laryngeal carcinoma, they give the disease a more ominous connotation.
What is the clinical significance of a palpable supraclavicular node?
An ominous one. A localized node in either the right or left supraclavicular fossa carries a 90% risk of malignancy for patients older than 40 and a 25% risk for younger patients.
Right supraclavicular nodes usually indicate metastatic involvement from ipsilateral breast or lung (but also mediastinum and esophagus). Because of bilateral crossed drainage, a right node also may reflect lung cancer of the left lower lobe.
Left supraclavicular nodes have instead a much wider differential diagnosis, since the left supraclavicular fossa drains not only the thorax but also various abdominal and pelvic sites. Hence, it functions as a sentinel for distant metastases.
What is Troisier’s node? What is its significance?
Troisier’s node (or sign) is another name for a palpable single left supraclavicular node. Frequently located just behind the clavicular head of the sternocleidomastoid, it suggests metastasis from a deep-seated carcinoma. Sources include not only the thorax (esophagus or ipsilateral breast and lung) but also the abdomen (stomach, liver, gallbladder, pancreas, kidneys, intestine) and pelvis (ovaries, endometrium, testes, and prostate).
Who was Troisier?
Charles E. Troisier (1844–1919) was a graduate of the University of Paris and, subsequently, a professor at the same institution. A well-respected pathologist and clinician, he mostly contributed to the understanding of lymphatic spread by cancer, but also rheumatoid nodules, meningitis, venous thrombosis, and hemochromatosis. In fact, bronzed diabetes (or hemochromatosis) is still referred to as Troisier’s syndrome.
What is Virchow’s node?
A left-sided Troisier’s node due to gastric carcinoma.
Who was Virchow?
Rudolf Ludwig Karl Virchow (1821–1902) was a graduate of the Friedrich-Wilhelm Institute for Army Doctors in Berlin, which he joined after realizing that his voice was not strong enough to support a career as a preacher. Preaching, however, remained one of his lifelong interests. In fact, after multiple rejections by various journal editors, he founded his own journal, which became known as Virchow’s Archiv , earning its pontificating editor the nickname “The Pope.” Virchow’s contributions to medicine were nonetheless staggering: he was the first to describe (and name) leukemia and understand thrombosis (see Virchow’s triad). He also was the first to recognize cerebral and pulmonary embolism (named that too) and the nature of arterial plugs in malignant endocarditis. He discovered amyloid, myelin, and neuroglia and contributed scores of papers to the understanding of cerebral hemorrhage, meningitis, and various congenital anomalies of the nervous system. By contrast, he had little interest in the emerging germ theory of disease and deeply detested evolution, which he tried to ban from school curricula. Although academically autocratic and reactionary, Virchow was politically very liberal – in fact, almost socialistic. He even helped construct some of the barricades during the 1848 Berlin uprising, a feat that cost him his job. Later, he became an outspoken opponent of Bismarck, who went so far as to challenge him to a duel in 1865 (Virchow agreed but on one condition: that the duel be fought with scalpels). In fact, he never missed a chance to strongly castigate the social injustice and poor hygienic conditions of his time, which he considered responsible for the frequent and recurrent epidemics. In a report to the government that became almost a political indictment of the industrial revolution, he asked, “Shall the triumph of human genius lead to nothing more than to make the human race miserable?” Still, he didn’t limit himself to cursing the darkness, but also lit a few candles – such as securing a good sewerage system and water supply for Berlin. His extracurricular interests included anthropology, medical history, and, above all, archeology. He even accompanied his friend Dr. Heinrich Schliemann to Troy in 1859 (writing an account of his famous discoveries) and concocted the idea of x-raying mummies. When he finally died at 81 from complications of a hip fracture sustained while leaping from a moving tram, it was said that Germany had lost in one single man her leading pathologist, sanitarian, anthropologist, and activist.
What is the best way to palpate a supraclavicular node?
Have the patient sit up, with head straight forward and arms down (to avoid mistaking a cervical vertebra or neck muscle for a node). Palpate from behind , since this allows optimal adaptation of your hand to the patient’s anatomy. Conversely, palpate from the front in the supine patient, where the lessened gravity may even mobilize the node and thus make it more accessible. End the exam by asking the patient to perform a Valsalva maneuver, or simply to cough. This may “pop” a deeply seated node, thus bringing it within reach of your fingers.
What is the best way to search for axillary nodes?
For the left axilla, grasp the patient’s left wrist or elbow with your left hand, and lift the arm up and out laterally. Then use the tip of your right fingers to palpate deep into the axillary fossa and roof. Do this first with the patient’s arm gently relaxed and passively abducted from the chest wall. Then repeat it with the arm passively and gently adducted. Examine the right axilla in a similar fashion, albeit with a reversed hand positioning. This technique allows the patient’s arm to remain completely relaxed, thus minimizing any tension in the surrounding tissues that could otherwise mask enlarged lymph nodes. It also is easy to carry out on the supine patient, very much as it would be if it were linked with the female breast exam ( Fig. 16.3 ).
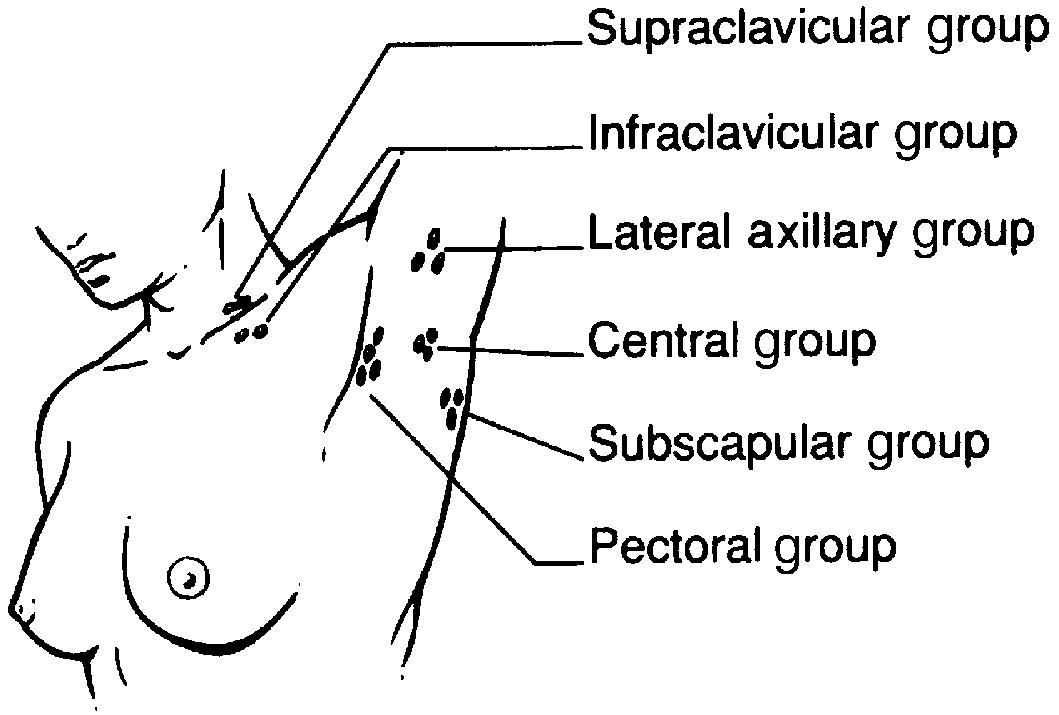
An alternative technique allows simultaneous examination of both axillae. To do so, ask the patient to lift both arms away from the chest. Then extend the fingers of both your hands and gently direct them toward the apices of the armpits. If you don’t want to place your fingers in direct contact with the axilla, you can do this through the patient’s gown. Now press your hands toward the patient’s body and move them slowly down the lateral chest wall. This allows you to explore the axillary regions in their entirety.
What is the clinical significance of axillary adenopathy?
Very much the same as that of cervical adenopathy: cancer and infection (with a sprinkle of systemic disorders, such as sarcoidosis). Note that axillary nodes should not be detectable, even though at times small , mobile, soft, and nontender nodes can be felt in normal people. Larger, tender, but still mobile axillary nodes usually reflect small wounds or infections of the arm (such as cat-scratch fever, tularemia, sporotrichosis, or staphylococcal and streptococcal infections, but also intravenous drug abuse). Conversely, harder, fixed, or matted axillary nodes indicate spread from malignancies, usually of pulmonary or breast origin (but lymphomas and melanomas, too).
How do you palpate an epitrochlear node?
By using your right hand to shake hands with the patient’s right hand, while at the same time “cupping” the patient’s elbow with the fingertips of your left hand. Palpate just above the elbow, along the inside of the upper arm, which is where the epitrochlear nodes reside. Then reverse hands and repeat the maneuver on the contralateral side.
What is the significance of epitrochlear nodes?
It depends on whether they are isolated or in a generalized setting (25% of adenopathies in other regions also will have palpable epitrochlear nodes). Either way, they are rarely benign. In a prospective study of 324 patients, the two most common causes were infectious mono and non-Hodgkin lymphoma/CLL , but also sarcoid, HIV, and dermatologic/connective tissue disorders. Historically, the condition has instead been associated with secondary syphilis, lepromatous leprosy, leishmaniasis, and rubella. Finally, an enlarged epitrochlear node also may reflect local inflammation of the hand/forearm. Hence, it is quite common in IV drug abusers.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here