Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() For videos accompanying this chapter see ExpertConsult.com . See inside cover for access details.
For videos accompanying this chapter see ExpertConsult.com . See inside cover for access details.
The lower eyelid and midcheek are areas that patients commonly present with, usually with the complaint of eye bags or just “looking tired.” Intuitively, it should be appreciated that these patients are actually looking for rejuvenation of the midcheek and to look more youthful, not merely for the elimination of the eye bags. The eye bags – bulging of the preseptal segment of the lower lid – is perhaps one of the earliest signs of facial aging, accordingly the patients come in complaining of the deformity. It is, however, certainly not the sole physical change responsible for the features of the aging midcheek. Collectively, these changes result in the “tired” look. Accordingly, removal of the eye bags alone, without concomitantly addressing other aspects of the aging midcheek, will lead to disappointment for the patient and the surgeon. In order to rejuvenate the midcheek, each component that changes with aging has to be addressed. Accordingly, technique selection depends on the specific aging changes needing to be addressed for the individual patient. Understanding the surgical anatomy is the key to the development of anatomically sound surgical approaches, that are effective, while minimizing trauma from the surgery and thereby reducing downtime and complications. ,
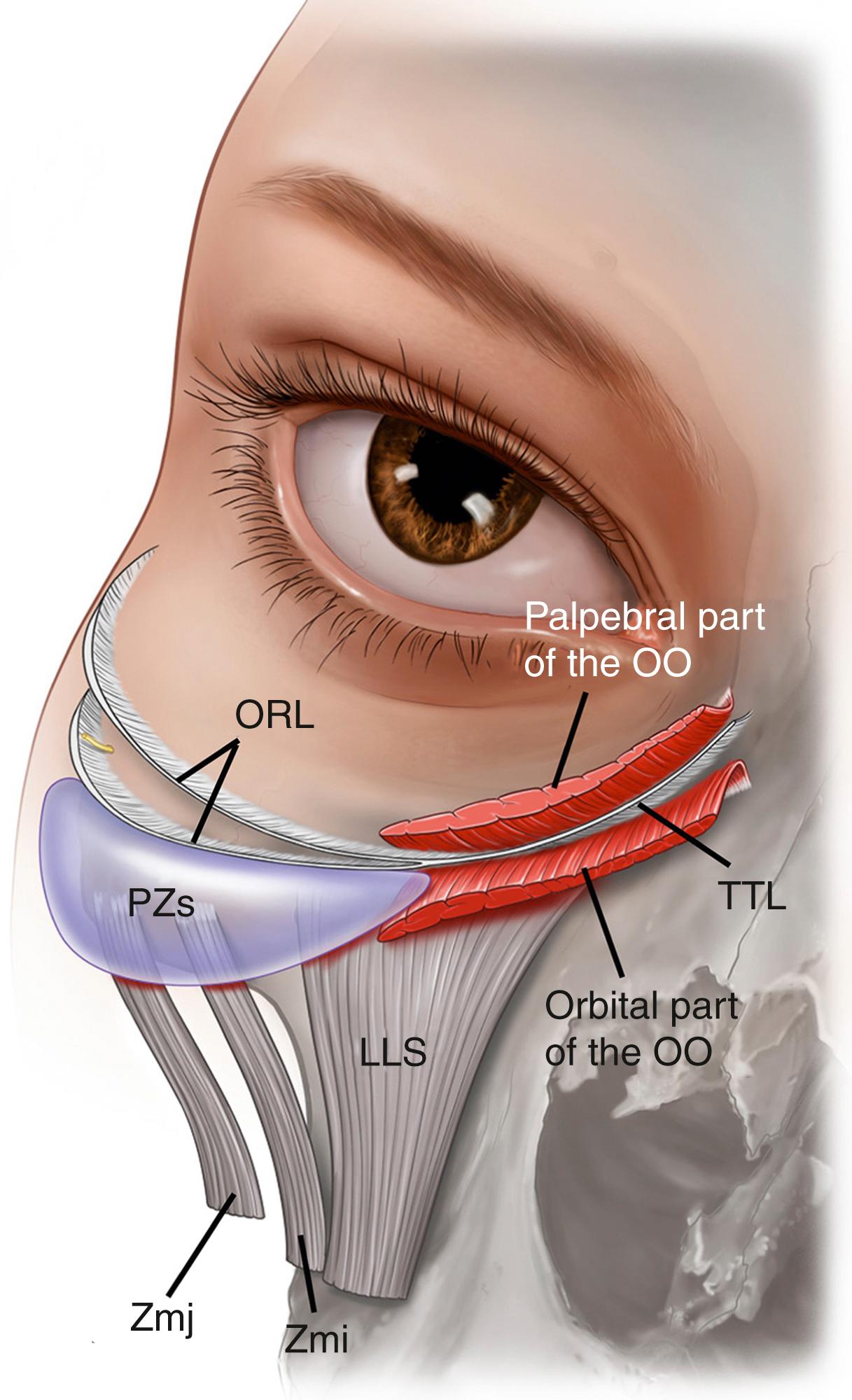
The principles of the construction of the facial soft tissues and the key concepts of facial gliding planes, called facial soft tissue spaces, and facial retaining ligaments have been discussed in our chapter on facial aging ( Chapter 62 ). The youthful midcheek is full and firm located high on the cheeks. The contour is smooth, without surface grooves or bulges. The pretarsal bulge, anatomically the pretarsal part of the orbicularis oculi, may be prominent relative to the preseptal part, and is the visual location of the junction of the lower eyelid and cheek – the so-called lid–cheek junction. What is called the youthful lid–cheek junction is high and actually on the lid itself, above the midcheek! This high lid–cheek junction appearance is so profound that it dominates over other aging areas of the face for the overall perception of youth and vigor.
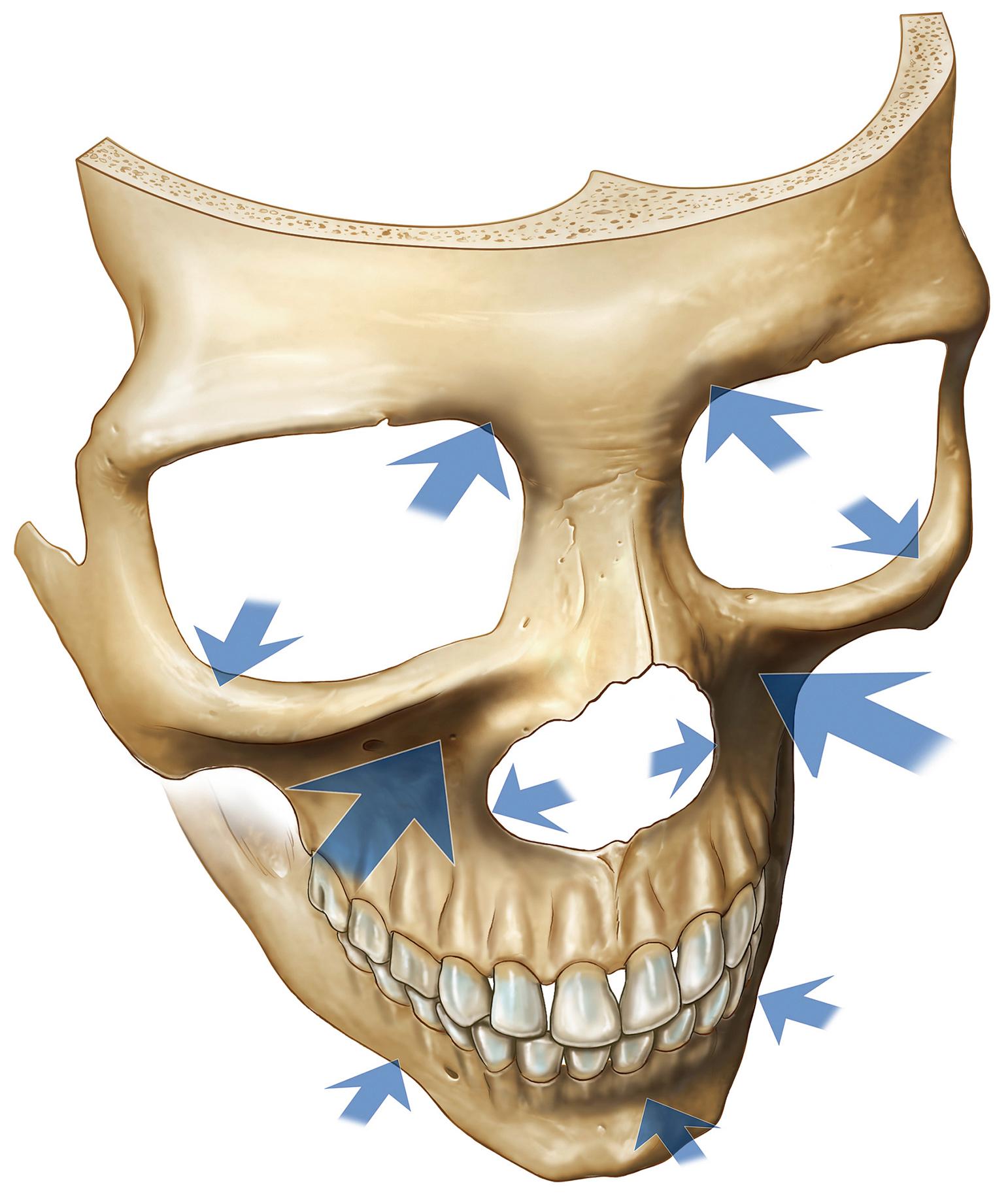
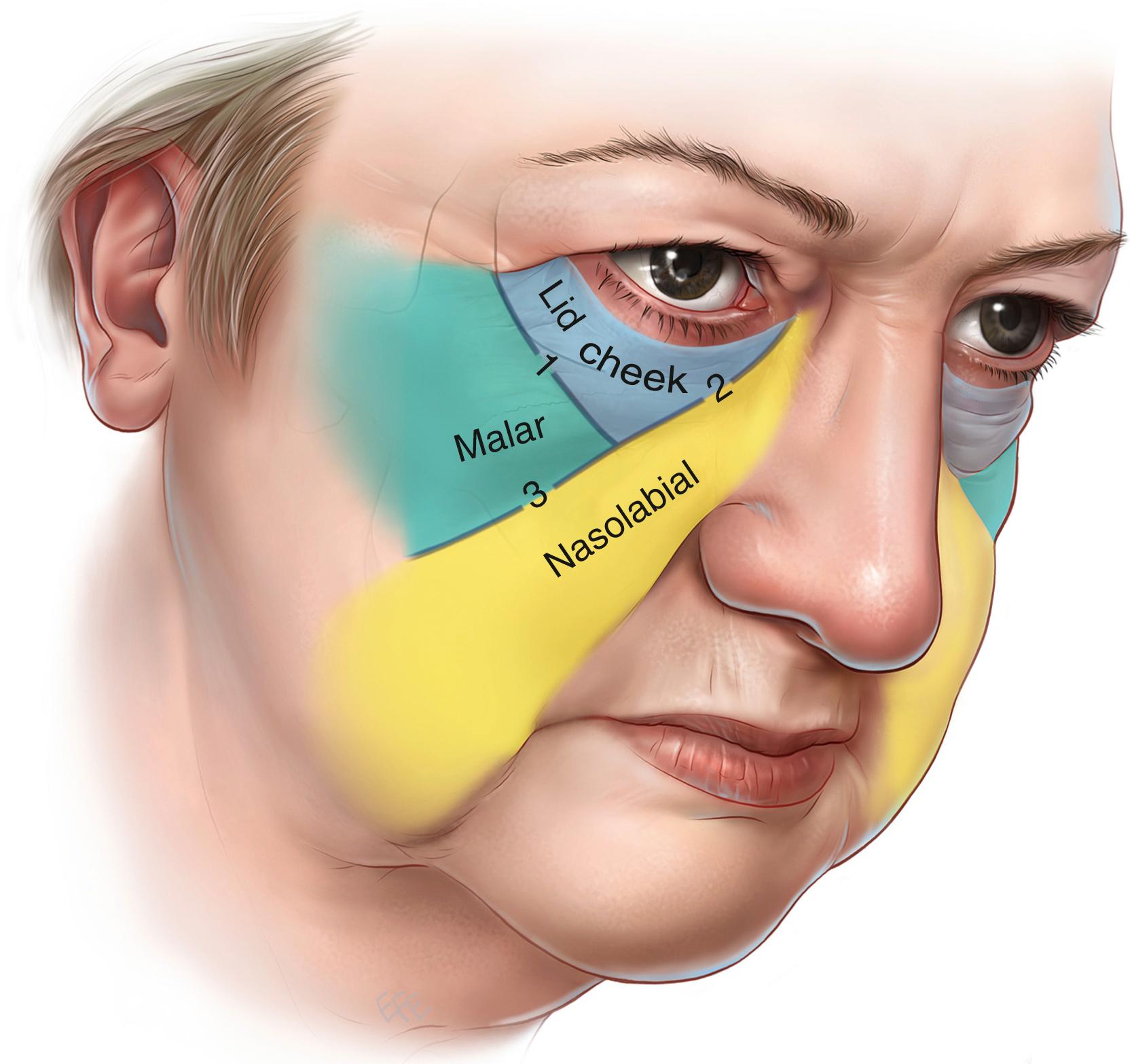
With aging, changes occur at the two fundamental levels: the midcheek skeleton and the overlying soft tissues . The midcheek skeleton, especially the maxilla medially, retrudes significantly with aging ( Fig. 65.1 ). , The resultant loss of projection and support for the overlying soft tissues predisposes to sagging of the tissue, which gives the visual impression of loss of soft tissue volume. Where the soft tissues overlie retaining ligaments the skin remains firmly attached to the underlying skeleton and manifests as surface grooves, given different names at different locations on the face. These include the nasojugal groove, so-called tear trough deformity, medially and midcheek furrow more laterally, whereas over the facial soft tissue spaces laxity in the roof of the space manifests as a surface bulge. In the lower eyelid, bulging over the preseptal space results in the development of eye bags. Laxity over the roof of the prezygomatic space is the anatomical basis for malar mounds or bags. This combination of relatively strong fixation in areas directly overlying retaining ligaments contrasted with laxity of tissue in the roof of adjacent soft tissue spaces results in segmentation of the midcheek into three segments – the lid–cheek, malar, and nasolabial segments ( Fig. 65.2 ). The visual location of the lid–cheek junction moves inferiorly to the groove formed by the tear trough ligament and the orbicularis retaining ligament, resulting in a lowered lid–cheek junction, which is a feature of aging.
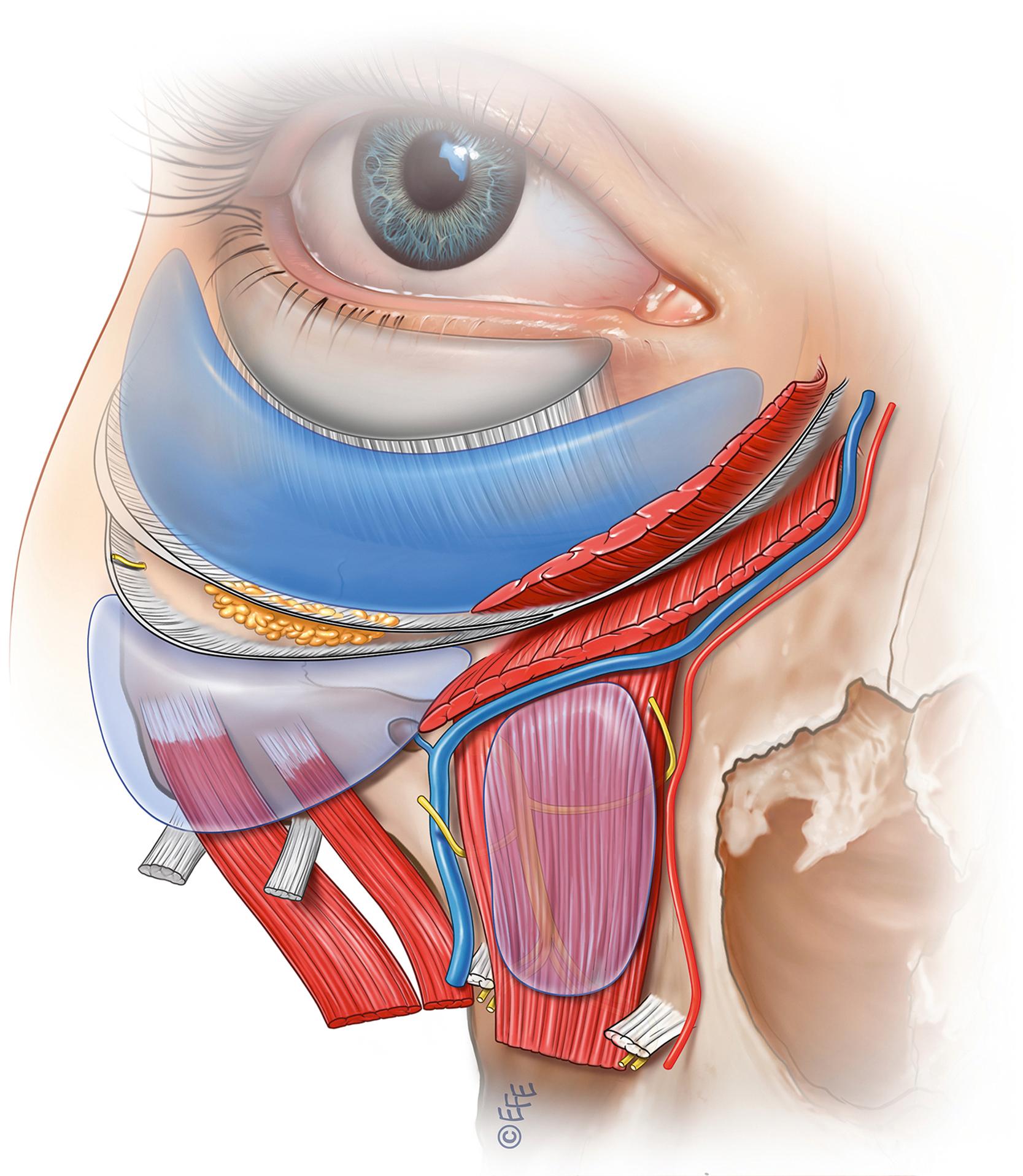
This combination of skeletal retrusion with the resulting weakening of the support for the overlying soft tissues and the propensity for the midcheek soft tissue to develop specific areas of laxity results in the prototypical and predictable changes seen with aging in the midcheek. To restore and rejuvenate the midcheek soft tissues, the logical approach is to surgically address these aging changes directly at the level these changes are occurring. To produce natural results and minimize downtime associated with surgical dissection, the key is to utilize the midcheek facial soft tissue spaces, which are preexisting gliding planes that are avascular with no vital structures traversing within ( Fig. 65.3 ). To access these spaces, the retaining ligaments in the boundary of the spaces must be sharply released. Once released, the surgeon will note the profound mobility of the roof with traction. This approach may be summarized as “through the facial soft tissues spaces with precise release of intervening retaining ligaments approach.” In terms of dissection plane, this is a sub-SMAS (superficial musculoaponeurotic system) dissection. This concept will be detailed in the surgical techniques below. Aging of the facial skeleton may be addressed by skeletal augmentation, using either hydroxyapatite bone substitute, structural fat grafting or facial fillers.
Patient selection is key in ensuring the delivery of results that are gratifying for the patient and surgeon. In general, patient with early aging changes may be treated with nonsurgical methods with good results. While noninvasive methods are appealing, it is a camouflage technique that provides no correction of the underlying anatomy for a long-term solution to rejuvenate the patient, and requires repeated treatments with associated risks. Modern advanced minimally invasive techniques (extended transconjunctival approach) are indicated for the majority of patients that one would consider for treatment with facial fillers. Significantly, the transconjunctival approach provides a long-term result compared with the use of fillers. It is up to the individual patient and plastic surgeon to decide on the approach to be used. For patients with more significant aging changes, a more aggressive approach incorporating some form of midcheek tightening is required to deliver a more profound rejuvenation.
A nonsurgical approach has become extremely popular with doctors of various expertise levels performing these procedures. Nonsurgical technique for rejuvenation of the midcheek is primarily delivered via the use of fillers. Fillers may be broadly classified into synthetic and autologous materials. The most commonly used synthetic fillers are hyaluronic acid (HA)-based. A variety of semi-permanent and permanent fillers are available in different markets. The authors recommend the use of HA-based fillers only as in the event of adverse outcomes or complications an antidote (Hylase) is available to dissolve and remove the unwanted filler material. Fat grafts are an autologous filler. The benefits of autologous tissues are they integrate with the facial soft tissue, are long lasting (when done correctly), and give benefits beyond volumization from mesenchymal stem cells in the transferred fat. The disadvantages are that harvesting of the fat is required and the procedure is more technically demanding. Fat grating, however, is usually used as an adjunct to surgical treatment and the discussion below pertains specifically to the use of HA-based fillers.
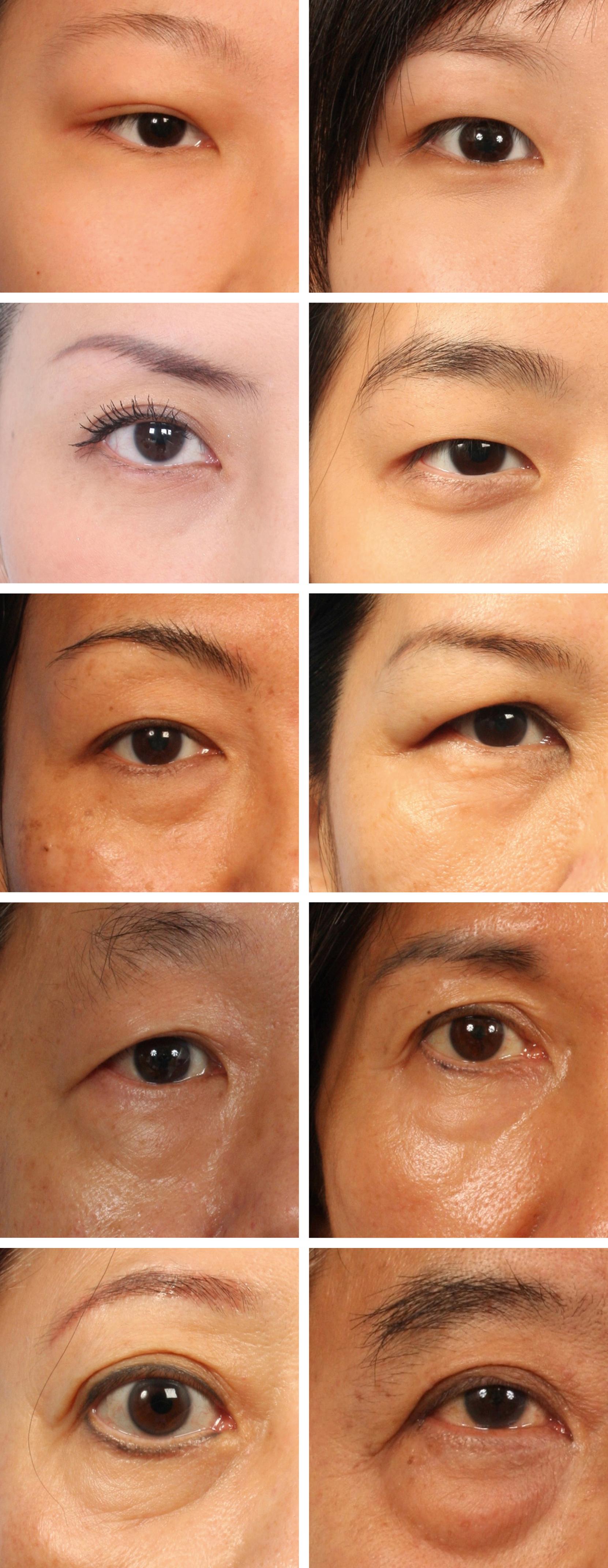
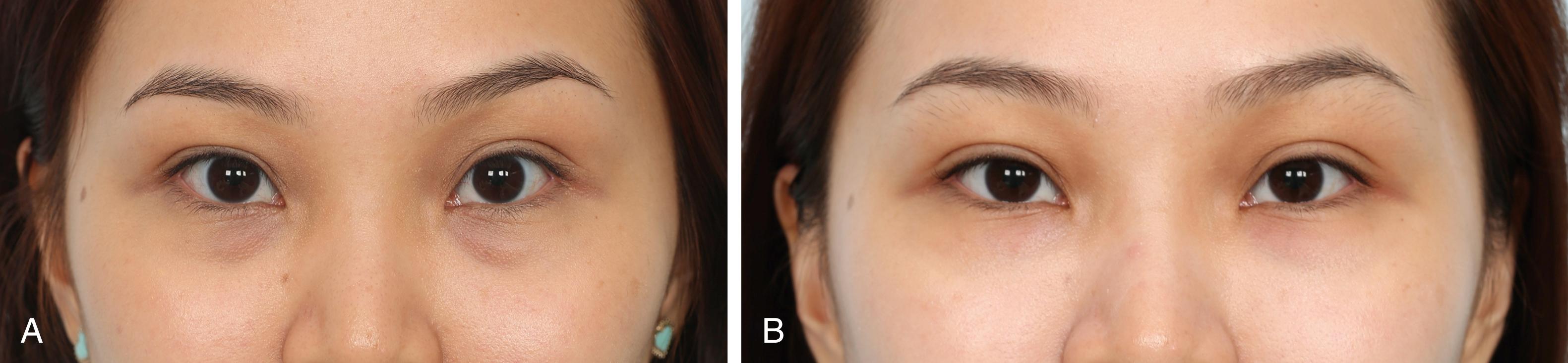
As discussed, aging is a multifactorial process, involving retrusion of the midcheek skeleton and laxity/sagging of the tissues. Fillers work by providing volume/support that to a certain degree compensates for the retrusion of the facial skeleton thus providing a subtle rejuvenating effect. Used in combination, fillers and neurotoxins soften the tear trough (TT) deformity in appropriately selected patients, in general, patients with early aging changes looking to have a little freshening up. Fig. 65.4 illustrates patient classification for treatment with injectables. This degree of “softening” is usually sufficient and may even be very satisfying for grades 1 and 2 TT deformity. As the tear trough ligament cannot be released or divided with nonsurgical techniques, the correction achievable in more advanced tear trough deformities (grades 3 and 4 TT) is generally insufficient and a surgical approach is needed.
Filler for the correction of the tear trough deformity and camouflaging mild eye bags may be placed deep and/or superficial. Deep placement of the filler should be placed caudal to the tear trough ligament on the anterior maxilla ( Fig. 65.5 ). Fillers here function to correct the skeletal/maxillary retrusion (which may be congenital in some patients or as a result of anterior maxillary resorption with aging in older patients) as well as the deflation that occurs with aging. This correction restores the soft tissue support inferior to the tear trough ligament and prevents the soft tissues from “dragging” on the tear trough ligament. The tethering effect is thus reduced and in some patients eliminated, resulting in a smoother lid–cheek junction. As the placement is deep and for the purpose of skeletal augmentation, the volume of filler material needed is relatively large; depending on the degree of maxillary retrusion, generally 0.1–0.5 mL per side over the anterior maxilla. Either blunt cannulas or needles may be used for deep injections. As for the type of product, a softer product should be used due to the very thin soft tissues in this area ( Fig. 65.6 ). Fillers should not be placed above the tear trough ligament as placement here will worsen the tear trough deformity, similar to the effect eye bags have on the tear trough deformity. Superficial placement, in contrast, is for a different purpose. It is to correct the superficial wrinkling that is seen in some patients. As the skin is very thin and delicate at the tear trough, the amount of filler material needed (or can be injected) is very little, no more than 0.05–0.2 mL per side. As for the type of product, only very thin or fluid material should be used.
Neurotoxins complement the use of fillers in the correction of the tear trough deformity, by relaxing the orbicularis oculi located above the tear trough ligament. The microbotox technique is preferred in the tear trough (about 2–4 units in 0.3 mL of saline) injected in a very superficial level raising blebs above and below the tear trough ligament to give a more even relaxation of the muscles.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here