Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Limb amputation, practiced throughout the centuries, is one of the most effective surgical procedures. With benefits ranging from pain relief to preservation of life, amputation offers a clear path to cure the patient. Despite the importance of a well-executed amputation, the task is often relegated to the least-experienced surgeon on the team. Incorporating deliberation with surgical technique can bring about an outcome that is both pain-free and functional. A small amount of additional time and effort spent in the operating room can potentially save the patient from a life of severe chronic pain and offers the best opportunity for functionality and independence.
Historically, amputation was challenging due to the critical triad of hemorrhage, infection, and pain. In France, Ambroise Pare, a French barber surgeon, introduced vessel ligatures, thus making the application of hot oil obsolete. Tourniquets were used by Morell, another French barber surgeon, in the battle of Besancon in 1674. Prior to the introduction of antisepsis by Joseph Lister in 1867, it is estimated that more than half of all amputees died from infection.
The surgeon must ensure adequate blood supply, sufficient viable soft tissue for coverage, and intact bony architecture ( Box 115.1 ). Other priorities include minimizing surgical trauma by avoiding crushing-type surgical instruments. Although surgical hemostasis is essential to successful amputation, there is a lack of consensus regarding the optimal methods. Beveled skin incisions should generally be avoided, skin should not be separated from underlying tissue, and skin flaps should not be under tension.
Assess arterial perfusion and bone architecture.
Handle all tissue with atraumatic technique.
Excise all nonviable and infected tissue.
Apply tourniquet to minimize blood loss.
Eliminate all sharp bone edges and fragments.
Minimize number of cuts across muscle.
Transect nerves sharply and allow retraction.
Minimize use of electrocautery.
Close wounds under no tension.
Perform myodesis or myoplasty to stabilize antagonistic muscle groups.
Use drains to reduce dead space.
Provide prophylaxis for deep venous thrombosis.
Administer prophylactic antibiotics.
Avoid weight bearing until adequate wound healing has occurred.
Use protective soft and rigid dressings.
Avoid excessive cosmetic tailoring of wounds.
Isolate infected or gangrenous tissue with barrier adhesive drapes.
In general, a longer stump is preferred due to improved prosthetic fitting and biomechanics, but not at the cost of leaving poorly perfused or infected tissue. Excessive soft tissue may interfere with prosthetic fitting and should be avoided. Over-attention to minor dog ears and irregularities may satisfy immediate cosmetic goals at the cost of wound healing and flap viability. Antagonistic muscle groups should be stabilized to prevent skeletal misalignment, a complication which is both detrimental functionally and cosmetically. Myoplasty , the suture fixation of antagonistic muscle groups, may help in this regard, in addition to myodesis , the direct suturing of the musculotendinous unit to the bone. Excessive periosteal stripping may devascularize the bone, leading to the formation of ring sequestra.
Infected areas should be isolated with the use of mechanical barriers. Open “drainage” or guillotine amputation is sometimes warranted in the setting of gross infection. A two-stage approach, delaying primary closure until a patient is clinically stable, may preserve limb length. Antibiotic coverage should be narrowed based on Gram stain and culture results, with discontinuation as soon as clinically warranted to prevent opportunistic infection such as Clostridium difficile .
Protection of the amputation site with use of a rigid or soft dressing may prevent injury in the case of falls. Incisions must be well healed prior to weight bearing. Given their limited mobility, patients are at high risk for developing deep venous thrombosis (DVT) and should receive prophylaxis. Perioperative prophylactic antibiotic use is recommended to limit wound infection following amputation.
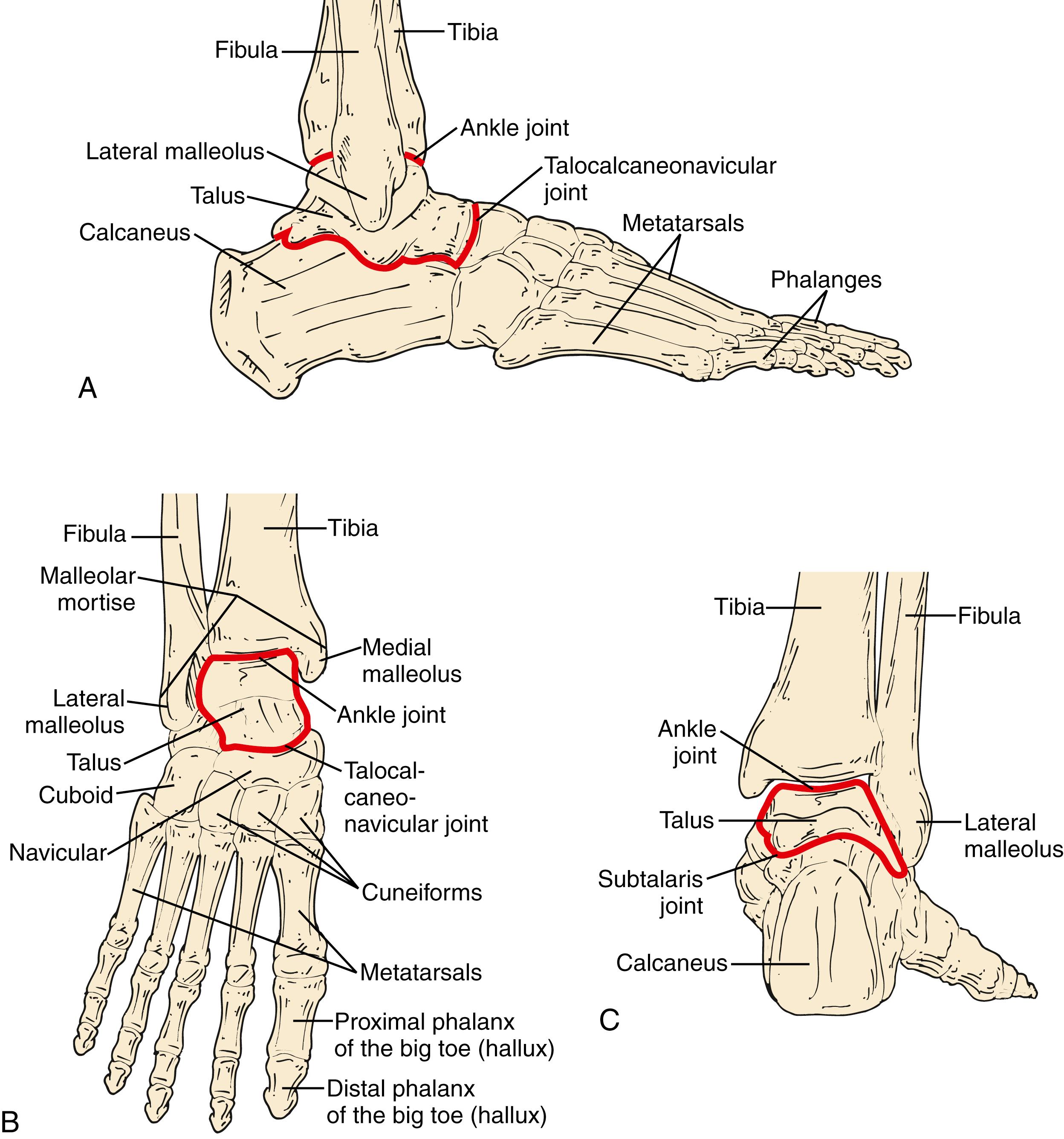
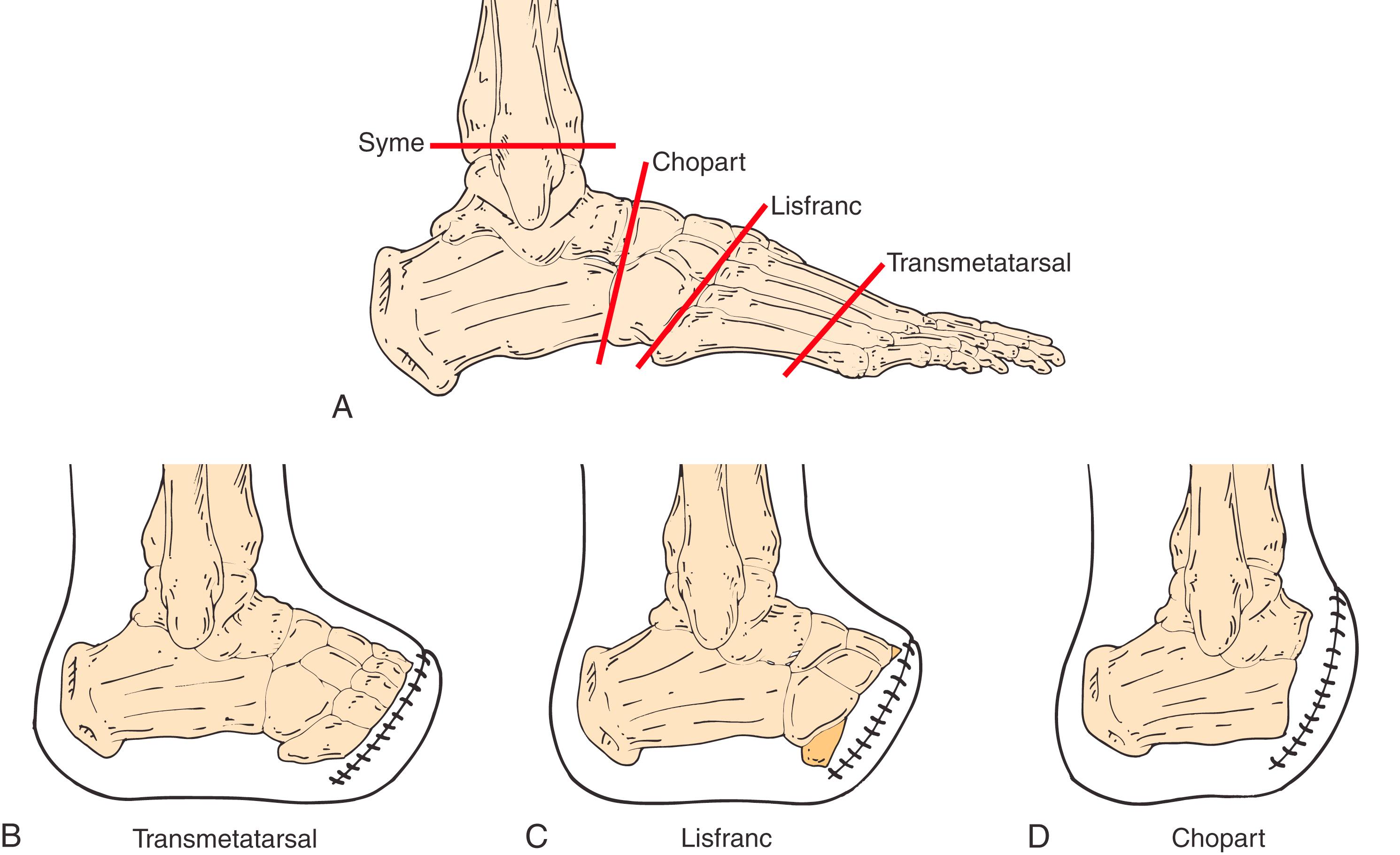
The bony anatomy of the ankle consists of seven tarsal bones and five metatarsals ( Fig. 115.1 ). The great toe has two phalanges, whereas the other toes have three. Medial and lateral sesamoid bones in the flexor tendons of the first toe provide stability. Joint capsules surround the interphalangeal and metatarsophalangeal hinge joints, and ligamentous and tendinous attachments work in concert with the plantar fascia to maintain structural integrity of the foot.
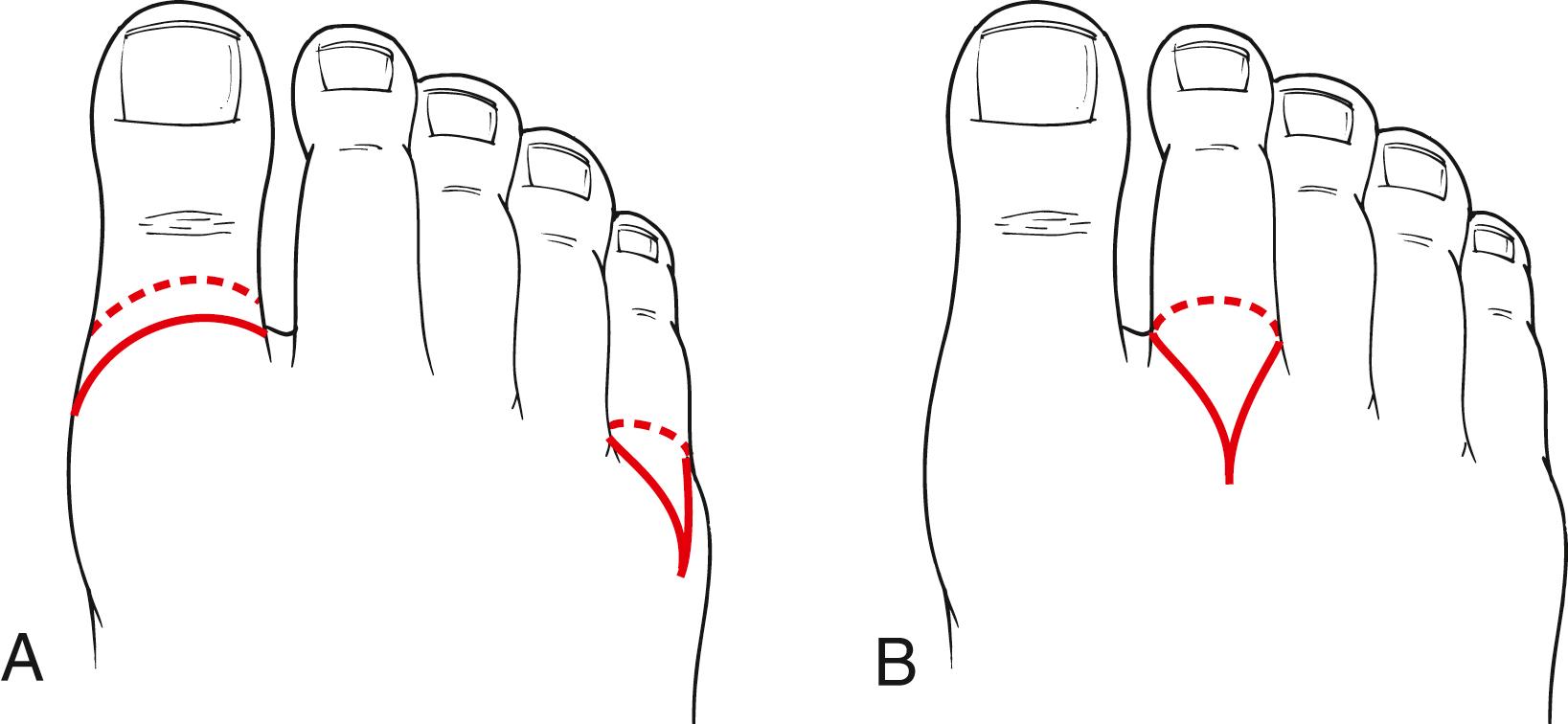
Toe amputation is appropriate for lesions of the middle and distal toe. A racket incision achieves tension-free closure. So-called for its shape like a tennis racket, the “handle” should lie longitudinally along the dorsal surface of the digit, in the midline for the second through fourth toes and away from the midline on the medial lateral surfaces for the first and fifth toes ( Fig. 115.2 ).
After incising the skin and soft tissues, the tendinous attachments are divided at the same level as the skin incision and the bone is trimmed back accordingly. If a disarticulation is warranted, a #15 blade is inserted into the joint capsule. Cartilage is excised with a rongeur and the bone edges are filed smooth. Excessive use of electrocautery should be avoided. Interrupted nonabsorbable monofilament sutures are used to close the wound in one layer.
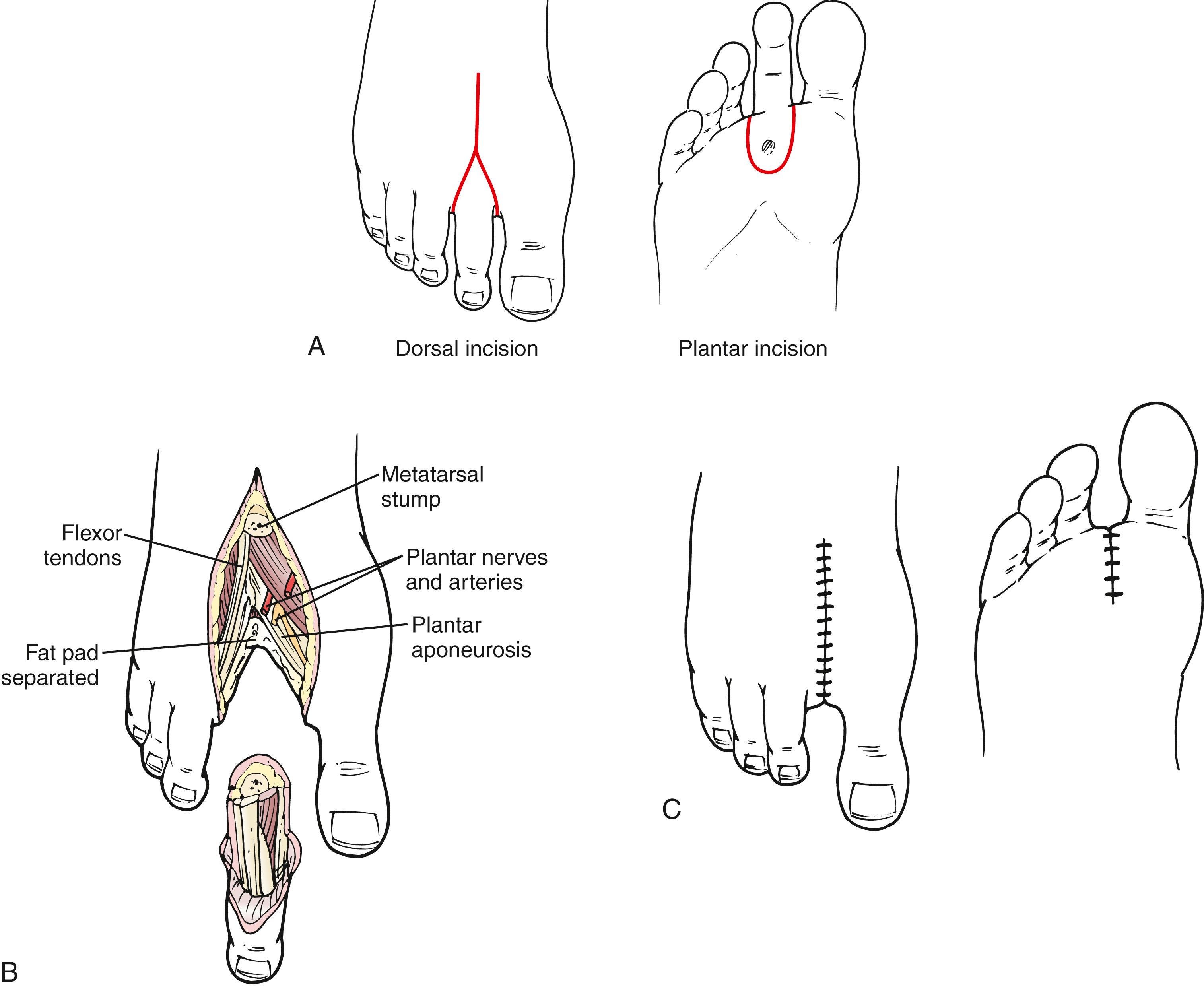
A ray amputation includes resection of the digit and variable length of the associated metatarsal. Ray amputations may be completed with a racket incision, with the “handle” or vertical portion extending proximal to the metatarsal head ( Fig. 115.3 ). The skin and soft tissues are incised, the tendinous attachments are divided and allowed to retract, and the metatarsal is transected before dividing the remaining soft tissues. Typically, the sesamoid bones are excised, associated flexor tendons are placed on tension and transected, and residual tendon is allowed to retract. Care should be taken to avoid injury to adjacent digital arteries and nerves.
Simultaneous amputation of the first and second rays will significantly alter gait. Isolated first ray amputation is prone to recurrent ulceration in up to 60% of patients. Some surgeons advocate a complete transmetatarsal amputation (TMA) of all remaining toes in this setting but there are no conclusive data governing this decision. A patient-specific approach is best.
Proximal to the phalanges are five metatarsals (see Fig. 115.1 ). They are stabilized by the deep transverse metatarsal ligaments and plantar ligaments distally and the plantar metatarsal ligaments proximally. The proximal metatarsals articulate with three cuneiform bones and the cuboid laterally. Collectively the tarsometatarsal (Lisfranc) joint connects the midfoot and forefoot.
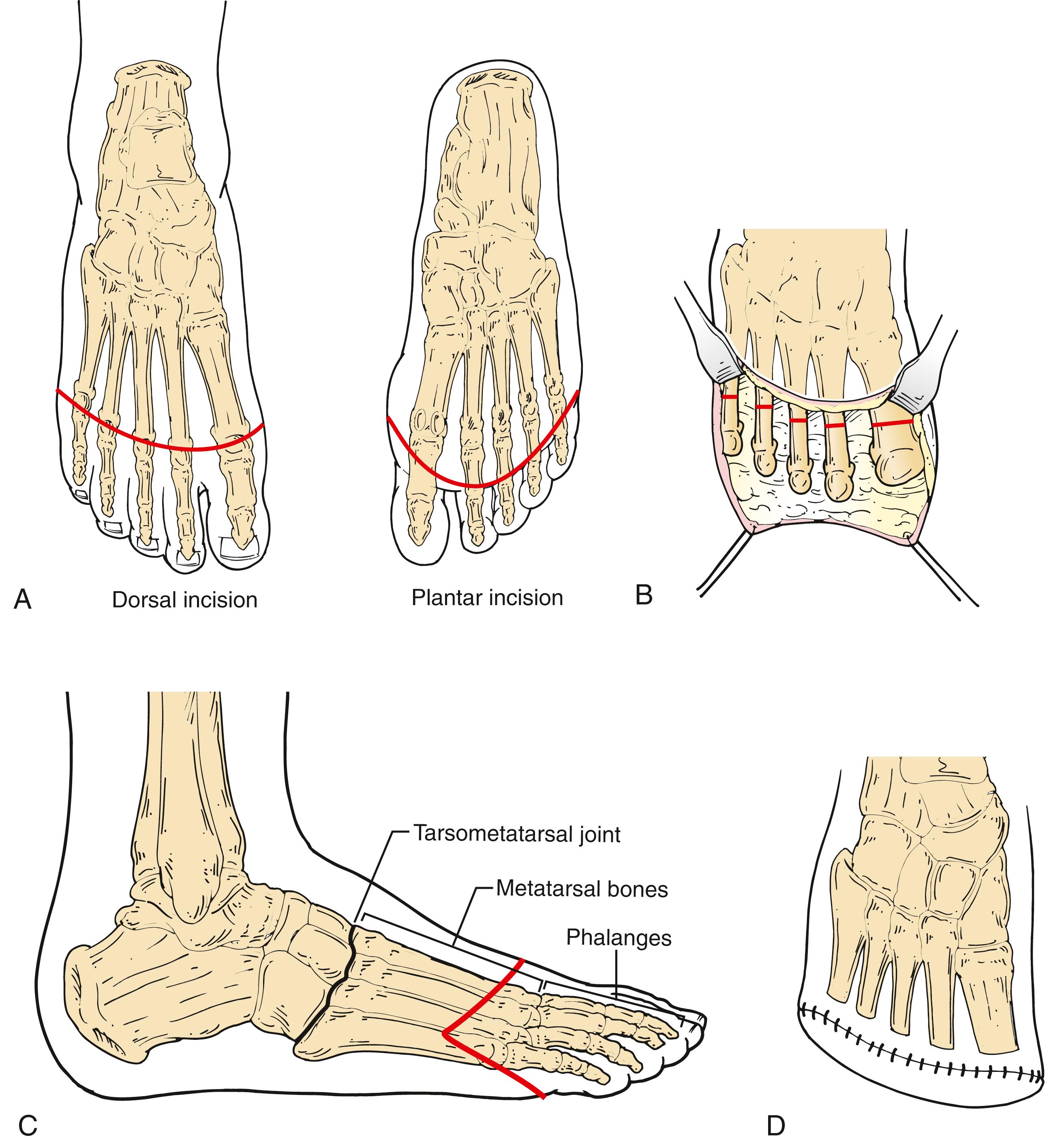
TMA is appropriate for wounds involving the entire forefoot or when multiple ray amputations are considered. TMA offers the ability to wear standard footwear with near-normal ambulation. TMA is contraindicated in cases of severe bony deformity of the midfoot and hindfoot which would lead to structural instability.
An incision extends transversely over the dorsum of the foot at the level of the distal metatarsals, coming to corners medially at the first metatarsal head and laterally at the fifth metatarsal head. Next, an incision extends from these corners onto the plantar surface across the base of the toes ( Fig. 115.4 ). The extensor tendons are divided at the skin level, the periosteum is incised, and the metatarsals are divided with a bone saw, each approximately 3–4 mm shorter than the last, moving laterally. A gentle 30- to 45-degree plantar bevel may facilitate liftoff with ambulation and reduce the risk of future ulceration. After dividing the bones, the plantar myofascial attachments to the metatarsal heads are divided. Care should be taken to stay close to the bones during the formation of the flap to avoid “button-holes”. The poorly vascularized tendons and sheaths in the plantar flap should be excised. To reduce the risk of recurrent ulceration due to equinus deformity, some surgeons recommend Achilles tendon lengthening (ATL) or transection.
Three proximal foot amputations are occasionally appropriate: Lisfranc tarsometatarsal disarticulation, Chopart midfoot amputation, and Syme amputation ( Fig. 115.5 ). , Two rarely performed hindfoot amputations are the Boyd and Pirogoff amputations. , Hindfoot amputations are performed primarily in children to preserve length and growth centers.
Many surgeons recommend transtibial (below-knee) amputation if TMA cannot be performed or has failed. Others suggest that increased limb salvage rates can be achieved with the use of unconventional foot amputations. ,
The tibia and the fibula articulate with the talus via the talocrural joint. The ligaments that join these bones are the deltoid, anterior and posterior talofibular, and calcaneofibular ligaments. The talus articulates with the calcaneus at the subtalar joint. The medial and lateral talocalcaneal ligaments and the cervical ligament support this joint. The talocalcaneonavicular joint is a multiaxial joint supported by the talonavicular and plantar calcaneonavicular ligaments. Supination (inversion) at this joint is produced by the tibialis anterior and posterior. Pronation (eversion) is produced by the peroneus longus and brevis. A heavy fibrofatty heel pad firmly adheres to the calcaneus and skin and provides protection during heel strike (see Fig. 115.1 ).
Because the strong ankle extensor attachments are divided in the performance of midfoot and hindfoot amputation, the Achilles tendon exerts unopposed plantar flexor forces on the residual foot. The Achilles tendon may require division or lengthening to prevent the development of an equinus deformity.
Lisfranc first described this amputation in 1815. The incision results in a long plantar flap (see Fig. 115.5 ). Tendons and synovial sheaths are divided at the level of the skin incision. The first, third, fourth, and fifth tarsometatarsal joints are disarticulated. The second metatarsal is divided 1 to 2 cm distal to the medial cuneiform. To reduce the risk of development of equinovarus deformity, Sanders recommended a modification of the Lisfranc amputation that preserves the base of the fifth metatarsal and the insertion of the peroneus brevis. The Achilles tendon is released by either transection or Z-plasty. , The plantar fascia on the flap is approximated to the dorsal periosteum with absorbable sutures. The skin is approximated with interrupted monofilament sutures or staples.
Described by Chopart in 1814, this amputation involves a long plantar flap similar to that used in the Lisfranc amputation (see Fig. 115.5 ) and is performed through the talocalcaneonavicular joint and the calcaneocuboid joint. An Achilles tenectomy is recommended. The extensor hallucis longus and the tibialis anterior tendons may be reattached to the talar neck. The extensor digitorum longus may be reattached to the calcaneus.
Because the Lisfranc and Chopart amputations result in a dramatic alteration in normal foot biomechanics, their durability may be limited. A short-leg plaster cast is applied over the sterile dressings on the operating room table. The cast must be molded to ensure that the talus is slightly dorsiflexed in relation to the tibia and that the calcaneal tuberosity is parallel to the long axis of the tibia. The cast is changed weekly to check wound healing. Weight bearing is allowed after 4–6 weeks. Patients with a Lisfranc amputation need little more than a toe filler with an ankle lace-up shoe. Patients with a Chopart amputation need a custom-fitted ankle-foot orthosis with a filler to hold the shoe adequately.
Syme first described this amputation in 1843. The anterior incision extends across the ankle just distal to the tip of each malleolus, while the posterior incision extends from the malleoli vertically down and across the sole of the foot (see Fig. 115.6 ). The extensor tendons are divided at the level of the skin incision. Next, the dorsalis pedis artery is ligated and divided. The ankle joint capsule is incised while plantar flexing the foot before dividing the medial and lateral ankle ligaments. The tendons of the posterior tibialis and flexor hallucis longus are transected, taking care to avoid injury to the posterior tibial artery. Next, the heel fat pad is carefully dissected by staying close to the calcaneus to avoid buttonholing. Finally, the ankle joint is disarticulated, and the specimen is passed off the table. In a one-stage amputation the malleoli are divided with a saw at the level of the articular surface of the tibia, and the width is reduced by vertical bone excision. Holes are drilled in the medial, anterior, and lateral parts of the distal tibia and fibula to secure the heel pad directly under the tibia. In a two-stage Syme amputation the wound is closed by suturing the heel flap to the dorsal fascia. Six weeks later the malleoli are removed through separate vertical incisions (see Hulnick et al. and Richardson for a detailed description of midfoot amputations).
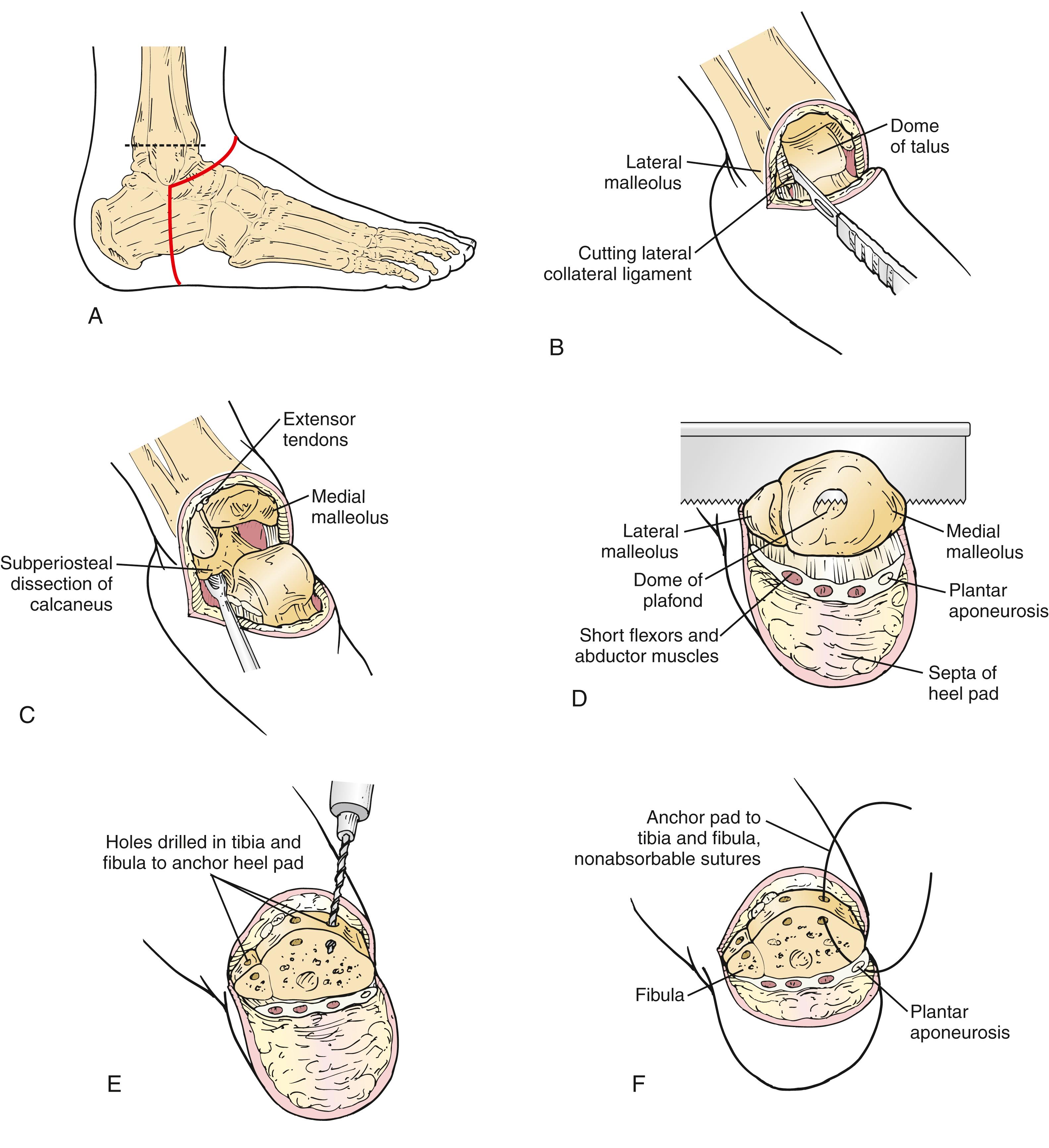
The chief advantage of the Syme amputation is the preservation of limb length, which may obviate the need for a prosthesis during brief periods of weight bearing, such as during transfer from a bed to a wheelchair. The disadvantages include the slight leg-length discrepancy, which may lead to biomechanical side effects in more proximal or contralateral joints. Furthermore, the prosthesis is typically bulky at the ankle and less cosmetically appealing than a conventional below-knee prosthesis.
Probably no surgical procedure is more prone to individual surgeon preference/bias than below-knee amputation (BKA). The choice of incision, length of bone, use of electrocautery, addition of myodesis or myoplasty, management of major nerves, skin closure techniques and postoperative dressings vary widely among even experienced surgeons owing largely to the absence of objective, randomized data.
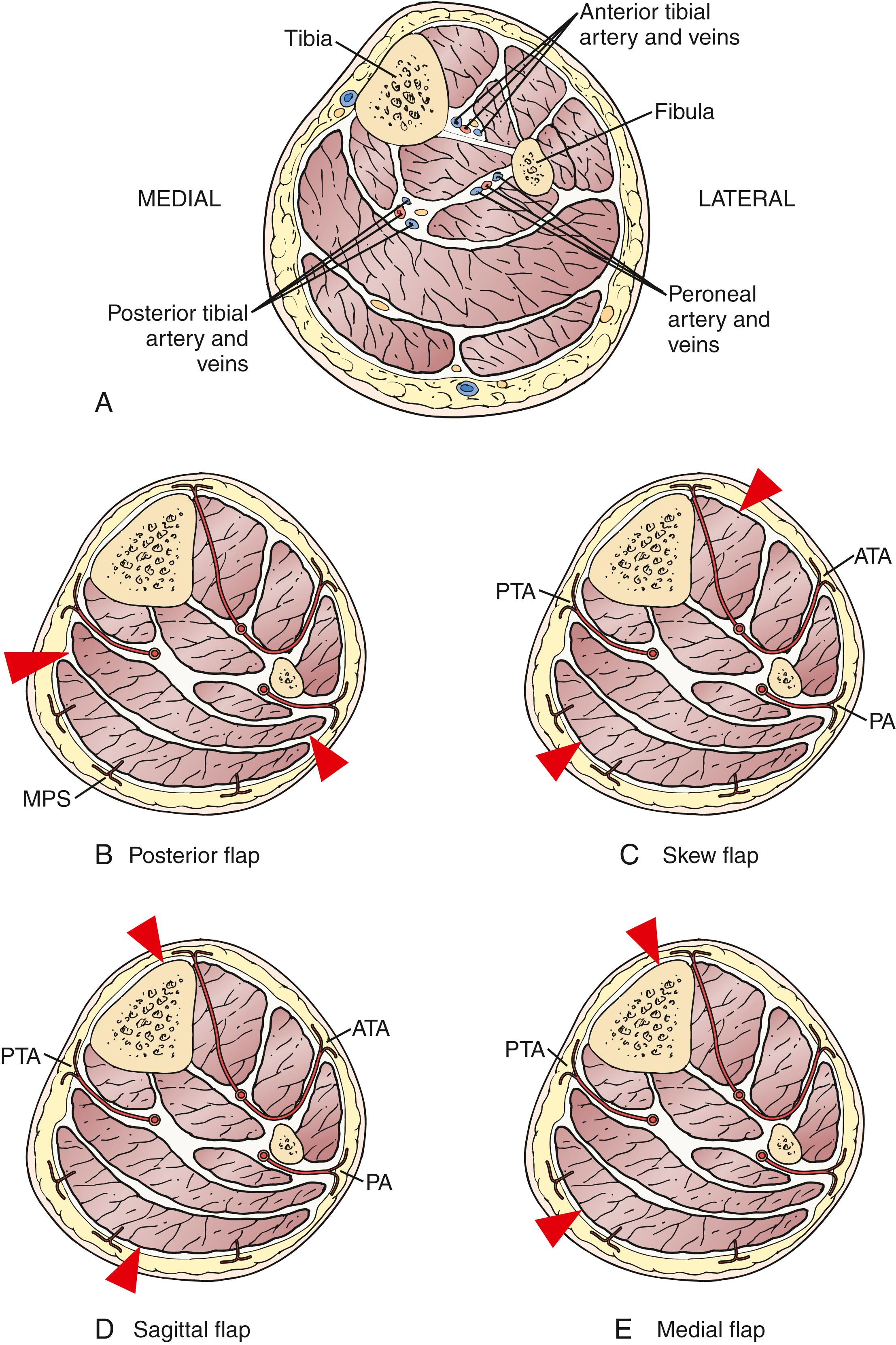
The leg contains four muscle compartments. The anterior compartment contains the tibialis anterior, extensor hallucis longus, and extensor digitorum longus muscles, as well as the anterior tibial artery and vein and deep peroneal nerve. The lateral compartment contains two muscles: the peroneus longus and brevis, as well as the superficial peroneal nerve. The superficial posterior compartment contains the soleus, gastrocnemius, and plantaris muscles. Last, the deep posterior compartment contains the flexor digitorum longus, tibialis posterior, flexor hallucis longus, and popliteus muscles, the posterior tibial artery and veins, peroneal artery and veins, and tibial nerve. The tibial nerve courses adjacent to the posterior tibial artery and veins ( Fig. 115.7 ). Posterior flaps, skew flaps, sagittal flaps, and medial flaps are based on corresponding musculocutaneous perforators; thus it is important to avoid separating the skin and soft tissue from its underlying muscle.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here