Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Major lower extremity amputations continue to be part of all vascular practices despite the general approach of aggressive limb salvage. Although often viewed as a failure of treatment, a major amputation should be considered a reconstructive and definitive treatment option. The convergence of several important factors, including the increased life expectancy of the general population as well as the epidemics of diabetes and peripheral artery disease (PAD), suggest that amputations will remain an important issue facing patients and surgeons for the foreseeable future. The goal of amputation is to remove all infected, gangrenous, or ischemic tissue and provide the patient with the longest functional limb. Avoidance of repeated amputations and uncomplicated healing of operative sites is crucial for the patient’s optimal recovery and best functional rehabilitation or palliation.
In the United States, approximately 60,000 major amputations (amputations above the ankle) are performed annually. Diabetes and PAD remain the major risk factors for lower extremity amputation worldwide. Patients with diabetes have an eight-fold greater risk of amputation than those without diabetes. Studies show that 25% to 90% of all amputations are associated with diabetes. , This association is due to the presence of neuropathy and infection, as well as the increased prevalence of PAD in patients with diabetes.
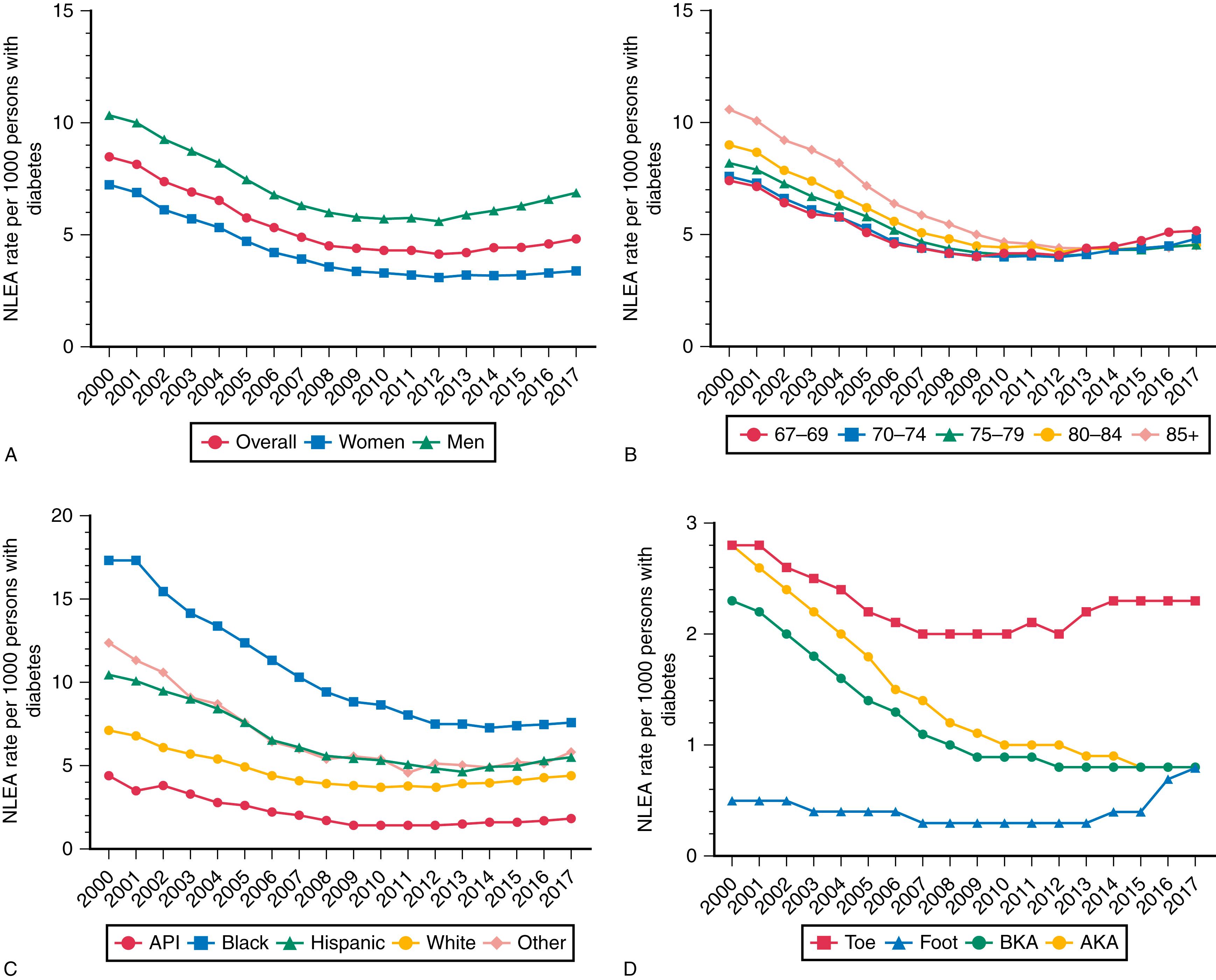
Despite the rising incidence of diabetes, current published data support an overall decrease in major amputation rates. A review of all Medicare claims from the Centers for Medicare and Medicaid Services between 1996 and 2006 showed a 29% decline in amputations. A report from the National Hospital Discharge Survey data on nontraumatic lower extremity major amputations (NLEA) and National Health Interview Survey data on diabetes prevalence showed the age-adjusted NLEA discharge rate per 1000 persons decreased from 11.2 in 1996 to 3.9 in 2008, while rates among persons without diabetes were unchanged. These trends were validated in a Scottish national cohort study from 2004 to 2008 where major amputations rates decreased by 40.7% from 1.87 per 1000 in 2004 to 1.11 per 1000 in 2008. This decrease in amputation rates initially plateaued around 2009 with nontraumatic lower extremity amputation occurring in 4.4 patients per 1000 people with DM, a decrease of nearly 50% compared to 2000. , Since 2009, however, there has even been a slight increase in the rates of NLEA reported on a state and national level among diabetic Medicare patients up to 4.8 per 1000 patients. The most recent study, however, includes foot and toe amputations in their overall calculation of NLEA; looking at subgroups of patients undergoing isolated below-knee and above-knee amputations, these rates actually continue to be stable and even slightly improved when compared to rates in reported in 2009 ( Fig. 114.1 ).
There is significant regional variation in the performance of amputation around the world, suggesting that factors other than medical issues may affect amputation rates. , , A United Kingdom study cited significant regional variation in amputation rates and stressed the need for consensus guidelines. The Global Lower Extremity Amputation Study Group reported that Navajo men undergo the highest amputation rate (first major amputation) at 44 per 100,000 population per year; the lowest rate was 2.8 per 100,000 per year in Madrid, Spain. Physician experience plays a key role in the selection of amputation as a treatment. In the treatment of critical limb ischemia, surgeon caseload and hospital volume have been shown to affect amputation rates, with low volumes being associated with higher amputation rates.
A study of a Medicare claims database demonstrated that the supply of vascular specialists influences the rate of amputation. A 0.30 increase in the number of vascular surgeons per 10,000 Medicare beneficiaries was associated with a 1.6% reduction in amputations. The distribution of vascular surgeons and interventional radiologists in the United States is strongly correlated not only with regional medical needs but also with local climate, education, crime, and transportation. This observation suggests that policies to increase the supply of vascular specialists in underserved areas may reduce regional disparities in amputation rates. Patient and healthcare provider education has also been demonstrated to reduce amputation rates. Earlier identification of patients at risk leads to timelier referral, and intervention.
A complex interaction exists between race, ethnicity and amputation rates. In certain groups, such as the Native American Navajo population, amputation rates appear to be related to the high incidence of diabetes. However, Blacks are more likely than Whites to undergo amputation as opposed to revascularization even when controlling for the presence of diabetes. , These differences have been attributed to variations in access to healthcare, treatment of comorbidities, and possible physician and patient factors. Insurance status also has an effect on amputation rates. Patients without insurance coverage have higher rates of amputation than those with access to health insurance. Data from the National Inpatient Sample documented that 34% of the 691,833 patients presenting with lower extremity ischemia from 1998 to 2002 underwent amputation. The primary amputation rates were significantly higher among patients who were non-White, low income, and without commercial insurance. Similar results showed that Black patients were 1.7 times more likely to have both primary and repeat amputations compared to other patients. These findings have also been affected by the recent changes in access to healthcare put forward by the Affordable Care Act (ACA). The Healthcare Cost and Utilization Project State Inpatient Database concluded that admissions for amputations across six states had increased since the enactment of the ACA, indicating enhanced access to medical care in those states. When Massachusetts adopted their expanded insurance coverage in 2006, there was an apparent decrease in preexisting disparities between Whites and non-Whites presenting with PAD. Another promising example of improved outcomes with better access is demonstrated in Arkansas, where patients with private insurance had a lower rate of amputation compared to those without. Whether this can be replicated on a national scale remains to be seen, although more states are noted to have similar trends as recently reported for Alabama and Massachusetts.
The interplay between revascularization and amputation is complicated. Over a 10-year period the Mayo Clinic reported a 50% reduction in amputation rates that corresponded to increased rates of lower extremity revascularization by both surgical and endovascular (EV) techniques. A Finnish study also demonstrated that an increased revascularization rate correlated with a decrease in major amputation among elderly patients. A U.S. study of two national (Nationwide Inpatient Sample and National Hospital Discharge Survey) and four state databases demonstrated that both the number of lower extremity revascularizations and the number of major amputations have declined; this has been accompanied by a substantial increase in lower extremity EV interventions. From 1998 to 2003 the volume of major amputations decreased 16% regionally (New York, California, New Jersey, and Florida) and 25% nationally. , However, minor amputations increased 4% regionally and 3% nationally. It has been speculated that the improved limb salvage rates are partially explained by the increase in total revascularization procedures (driven by EV interventions due to the perceived decreased morbidity). Earlier EV interventions in less critical lesions and expanding EV procedures to the patient who is too high-risk for open surgery may contribute to the lower rates of major amputations. Additionally, failed EV procedures may not directly translate into amputations, since not all of these procedures are performed on people with extensive tissue loss or even advanced CLTI. Other possible factors contributing to lower rates of amputation include greater awareness of PAD, clear guidelines for the medical management of PAD risk factors, atherosclerosis, and improved wound care.
High-risk patients treated with EV interventions have superior rates of limb salvage and maintenance of ambulation compared to patients undergoing primary amputation. However, these patients have no better functional benefit than those treated with primary amputation after 1 year. When autologous vein is available, the long-term results of the Bypass versus Angioplasty in Severe Ischemia of the Leg (BASIL) trial indicate that the outcomes of a bypass surgery–first approach is superior to a balloon angioplasty–first strategy in terms of amputation-free survival. The ongoing debate over which patients benefit from EV interventions first over surgery first is the surmountable task undertaken by the Best Endovascular versus Best Surgical Therapy in patients with Critical Limb Ischemia (BEST- CLI) trial investigators, the results of which are greatly anticipated.
The ideal balance of EV and open surgical reconstructions has yet to be determined for lower extremity ischemia. Nationwide Inpatient Sample data suggest that lower extremity revascularizations have reached a plateau of approximately 140,000; similarly, major amputation may have settled near 60,000 annually. , The Trans-Atlantic Inter-Society Consensus (TASC) II Working Group documented that the incidence of major amputations varies from 12 to 50 per 100,000 population per year. The total number of revascularizations, in particular endovascular procedures, may be underestimated because same-day EV procedures (not hospitalized), as well as procedures performed in outpatient-based laboratories (OBL) are not being captured in the Nationwide Inpatient Sample database. This has multiple effects, primarily limiting the capture of these procedures in national databases, as well as limiting the ability to track their outcomes. This trend potentially skews our overall numbers when it comes to procedures performed, immediate technical results, effect of patient ambulation as well as longevity of procedures performed. With an increasingly aging population and their physiologic limitations, our ability to perform traditional open revascularization is limited yet endovascular approaches seem feasible even in the most frail patients and may greatly confound the rates of amputation after revascularization attempts.
Indications for amputation have traditionally been divided into acute ischemia, chronic ischemia, foot infection, severe traumatic injury, and lower extremity skeletal or soft tissue malignancies. Trauma and malignancy are beyond the scope of this chapter and are not discussed. In the presence of acute ischemia, major amputation is undertaken for irreversible ischemia, for severe ischemia with no revascularization options, or following unsuccessful attempts at revascularization. Amputation for chronic ischemia may be performed owing to failure of revascularization, lack of suitable conduit or target arteries, severe patient comorbidities, poor functional status, or extensive gangrene or infection such that foot salvage is not possible. Pedal sepsis without ischemia constitutes another major subgroup of patients undergoing amputation; this presentation is extremely common in patients with diabetes and associated neuropathy. The underlying indications for amputation frequently overlap, making it difficult to evaluate outcomes based on the indications as reported in literature.
Malone reported the indications for amputation as follows: complications of diabetes (60%–80%), infection without diabetes (15%–25%), ischemia without infection (5%–10%), chronic osteomyelitis (3%–5%), trauma (2%–5%), and miscellaneous (5%–10%). These classifications have a certain degree of overlap and mask the interaction between ischemia and diabetes. This simplistic breakdown does not provide clear insight into the true influence of ischemia or the full potential of revascularization to reduce amputation rates. In addition, because no revascularization is universally successful, amputation may ultimately follow revascularization.
The presence of diabetes, either alone or in combination with PAD, contributes to the majority of major nontraumatic lower extremity amputations. The overall incidence of diabetes in patients undergoing amputation is reported as approximately 60% (ranges from 25%–90%). , This information is based on hospital discharge diagnoses and thus may not be all encompassing and completely accurate; however, it is perhaps the most inclusive data we have. Although many general classifications overemphasize the role of diabetes and understate the role of concomitant ischemia, it is clear that diabetes alone confers a higher risk (as high as an eight-fold increase) of amputation.
Attempts have been made to categorize the indications for major amputation to explain why amputations continue to be performed despite aggressive revascularization programs. When identifying the indications for amputation, it must be recognized that with chronic ischemia, limb loss may ultimately occur despite revascularization. In addition, the index presentation may be someone with an acutely or chronically ischemic limb that is beyond any hope of salvage. The influence of gangrene and pedal sepsis must also be considered because they have a significant impact on the options for limb salvage. Lastly, patient comorbidities and ambulatory status influence the decision for amputation.
The TASC II Working Group reported that the rate of primary amputation in chronic critical leg ischemia is approximately 25%. Non-reconstructable vascular disease is the most common indication for secondary amputations, which accounts for nearly 60% of patients. In an article further assessing the indications for amputation, a series of 131 consecutive major lower extremity amputations were reviewed and the indications for amputation were classified ( Table 114.1 ). In this academic vascular setting, more than 50% of patients who underwent amputation did so following a prior attempt at limb salvage via revascularization or had no anatomically feasible revascularization options. This group of patients had exhausted the armamentarium of the vascular surgeon. Seventeen percent of patients were not considered candidates for aggressive attempts at limb salvage owing to preexisting medical issues including nonambulatory status (8%), or having excessive surgical risk (9%). In addition, 32% of patients had nonsalvageable limbs at presentation due to extensive pedal gangrene, pedal sepsis, or a nonviable foot that mandated primary amputation.
| Indication for Major Amputation | Percentage of Cases ( n = 131) |
|---|---|
| Critical limb ischemia with failed revascularization | 39 |
| Extensive pedal gangrene | 15 |
| Unreconstructable arterial anatomy | 11 |
| Overwhelming pedal sepsis | 9 |
| Excessive surgical risk | 9 |
| Nonviable, acutely ischemic foot | 8 |
| Nonambulatory status | 8 |
Similar findings were reported in another series of 172 major amputations. The indication for amputation was critical ischemia in 87%, and complications of diabetic neuropathy without significant ischemia in 13%. Forty-six patients (30%) had prior bypass failures or amputations despite patent reconstructions, and 10 (6%) had no revascularization options; therefore, 36% had exhausted the resources of revascularization. Eighty-five patients (55%) underwent primary amputation because of severe comorbidities, poor functional status, extensive necrosis, or a combination of these factors. Together the previous studies highlight the central role of both ischemia and tissue loss in the determination of the need for major amputation.
The Society for Vascular Surgery’s Wound, Ischemia and foot Infection (WIfI) classification system helps define the factors influencing limb salvage. This system includes the grading of key elements of the wound (W), degree of ischemia (I), and severity of foot infection (fI). The composite WIfI stage then gives greater detail regarding the risk of amputation and benefit of revascularization. Early validation studies demonstrated that worsening WIfI stages are associated with major amputation in patients undergoing revascularization for chronic limb-threatening ischemia (CLTI). However, among patients with diabetic foot ulcers, while the WIfI score predicted wound healing, it was not predictive of amputation in patients without peripheral arterial disease.
The significant role that delay in patient presentation plays in limb salvage cannot be overstated. The mean time to vascular surgery consultation was 73 days for pedal tissue loss and 27 days for ischemic rest pain in the report by Nehler and colleagues. This delay likely accounts for the large percentage of primary amputations in their series and underscores the need for patient and referring physician education. In a report by Bailey and coworkers, only 24% of patients with critical limb ischemia were perceived as needing “urgent” vascular consultation, with a mean 8-week duration of symptoms before vascular evaluation. This suggests that delayed patient presentation involves patient factors, referring physician issues, as well as issues with access to specialist care.
The most important decision in treating CLTI is the initial determination of whether to attempt limb salvage or proceed with primary major amputation. Despite widespread discussion of great triumphs in revascularization, there is a growing awareness that primary amputation may be the best approach in specific patient subsets. As stated earlier, more than 140,000 lower extremity revascularizations are performed annually in the United States. In recent years, open revascularizations have been partially replaced by EV procedures, yet nearly 60,000 major amputations are still being performed each year. , This implies that the ratio of amputation to revascularization may be close to 1:2 nationally. Many specialty centers may have a much lower ratio, owing to the filtering effect of referring physicians. Many patients perceived as not being candidates for revascularization are treated locally with amputation and are never referred to these high-volume centers specializing in revascularization.
The ratio of major primary amputation to revascularization differs among facilities and may vary because of surgeon experience and practice protocols. One prospective study demonstrated that 43% of the 224 patients presenting with limb-threatening ischemia were treated by primary amputation, and 57% were treated with revascularization. Diabetes mellitus, end-stage renal disease, tissue loss, and poor functional status were all predictors of treatment with amputation as opposed to revascularization.
A reasoned approach to patients presenting with CLTI is necessary. A thoughtful strategy considering the patient’s comorbidities, the status of the foot, and the complexity of the required revascularization has been outlined by Nehler and colleagues. In a good-risk patient with minimal pedal tissue loss, an aggressive attempt at revascularization should be undertaken with appropriate EV or open bypass techniques including the consideration of alternative vein conduits. However, when the patient’s overall health status is poor or the foot lesions are extensive, primary amputation must be considered. Additionally, patients presenting with poor baseline functional status, extreme frailty or overall poor physiologic state should be considered for primary amputation. An aggressive use of revascularization, particularly EV interventions, likely has resulted in limb salvage attempts in higher-risk patients which may have contributed to the reduction of overall major amputations. , Despite this, secondary amputations are not an uncommon occurrence. In a study of 358 patients (412 limbs), patients with limb loss despite patent EV interventions were compared with the rest of the EV-treated group and with those who underwent amputations with patent bypasses (APBs). Amputations occurring despite a patent, revascularized segment constituted 38% of limb loss in open and 80% in EV-treated patients ( P = 0.001). Most amputations in the EV group were performed within 3 months and the indications were extensive tissue loss or limb dysfunction after radical debridement of infection or gangrene (37%), recurrent infection (42%), and failure to reverse ischemia (21%).
The perceived improved outcomes following revascularization compared with amputation have driven the belief that revascularization is always the better option. However, an examination of the data demonstrates that functional outcomes following amputation may not be markedly different from those following revascularization for specific patient subgroups. Taylor and associates analyzed 553 patients who underwent 627 primary major limb amputations. In patients younger than 60 years, functional outcomes following BKA were similar to those of patients undergoing successful revascularization. Such information lends credence to the observation that primary amputation should be considered not a failure of therapy but a valuable, and often rehabilitative treatment option. , ,
The advances in percutaneous revascularization have raised the question of how best to treat the patient considered “unfit” for open revascularization. Taylor and colleagues reported an analysis of 314 patients treated for critical limb ischemia who were unsuitable for open revascularization owing to medical, functional, or mental comorbidities. Patients were treated with either percutaneous transluminal angioplasty (PTA) or major amputation. The 131 patients treated with PTA had higher rates of maintenance of ambulation and independent living compared with the 183 patients treated with amputation. However, the PTA group had a higher mortality rate, and the advantages in ambulation and independent living lasted only 12 months and 3 months, respectively. In the “unfit” patient, EV treatment may indeed be no better than primary amputation.
In patients with extensive foot lesions, severe comorbidities, or unfavorable anatomy, primary amputation is often the best treatment option. , , In addition to unfit physiology and anatomy, the patient frailty (overall functional status measured by a variety of methods) should be immediately considered prior to deciding on a course of treatment. Because of delayed referral, many patients ultimately undergoing amputation present to the vascular surgeon with extensive pedal necrosis, making limb salvage unlikely, regardless of arterial targets for revascularization. End-stage renal disease presents a particularly difficult challenge, and the presence of advanced heel gangrene in this group of patients may also best be treated with primary amputation. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here