Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A 14-year-old Black American morbidly obese female underwent hemipelvectomy for a pelvis osteosarcoma. She subsequently underwent pelvic reconstruction with a free fibular vascularized bone graft and a reconstruction plate by the orthopedic oncology and hand surgery services. Unfortunately, she developed complex and pending lower back, gluteal, and sacral wounds with potential exposure of the fibular bone graft and hardware. The plastic surgery service was asked to provide better soft tissue wound closure to improve the chance of primary healing of the surgical incision sites ( Fig. 30.1 ).

All incision sites were reopened and all necrotic skin and subcutaneous tissue were debrided. There was a significant amount of hematoma under the skin incisions and the hardware used for reconstruction could potentially be exposed ( Fig. 30.2 ). In this location, there are no local muscle or myocutaneous flaps available for soft tissue reconstruction. Because this patient was quite large with thick subcutaneous tissue even though she was only 14 years old, a large perforator-plus fasciocutaneous rotation/advancement flap was planned. One or two large perforators were identified by a handheld Doppler and should be included within the flap design. With a suprafascial dissection, all identified perforator(s) might be visualized and should be preserved during the flap dissection. The back cut could safely be performed as long as those perforator(s) were preserved. The flap could also be readvanced with even more back cut.
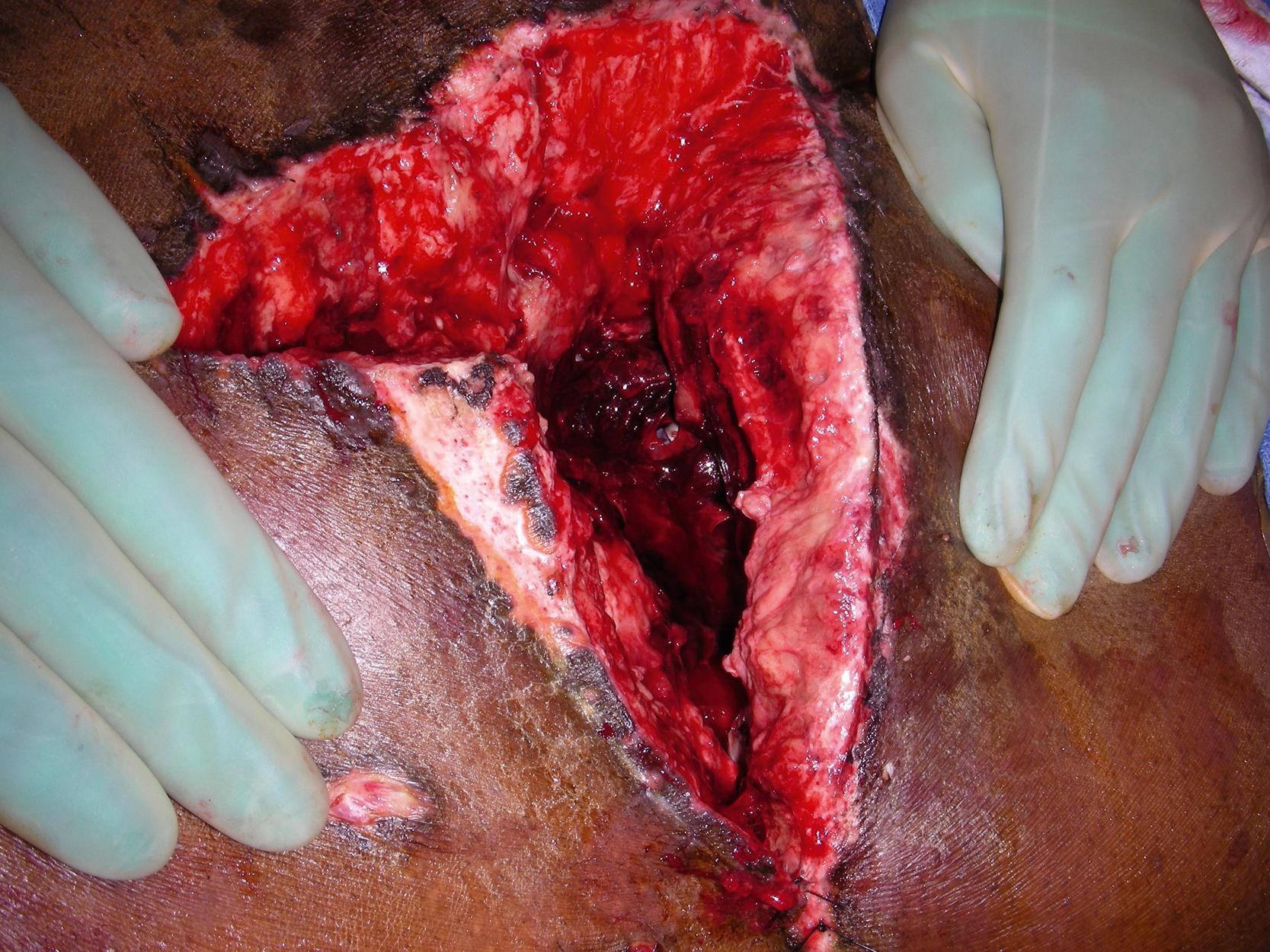
Under general anesthesia with the patient in the prone position, the entire lower back, sacral and gluteal incisions were reopened. There was a fair amount of necrotic skin and subcutaneous tissue along all previous incisions. All necrotic tissues were sharply debrided. Hematoma within the pelvic cavity was removed manually. The wound was then irrigated thoroughly with antibiotic solution.
A good gluteal perforator was mapped with a handheld Doppler. A 30 × 15 cm large skin rotation flap was designed based on the location of the perforator and soft tissue defect ( Fig. 30.3 ). The proposed incision of the flap was infiltrated with 1% lidocaine with 1:100,000 epinephrine.

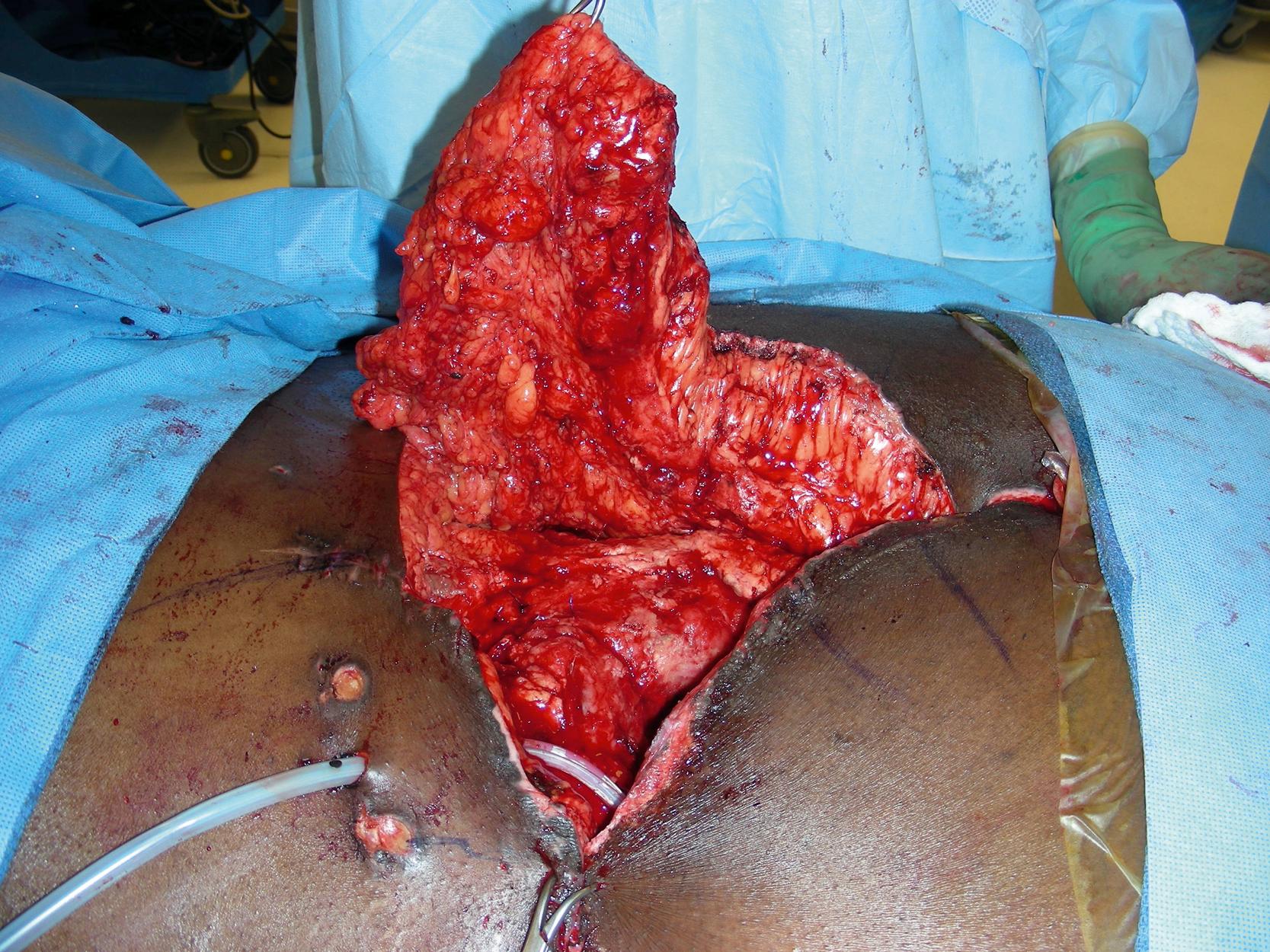
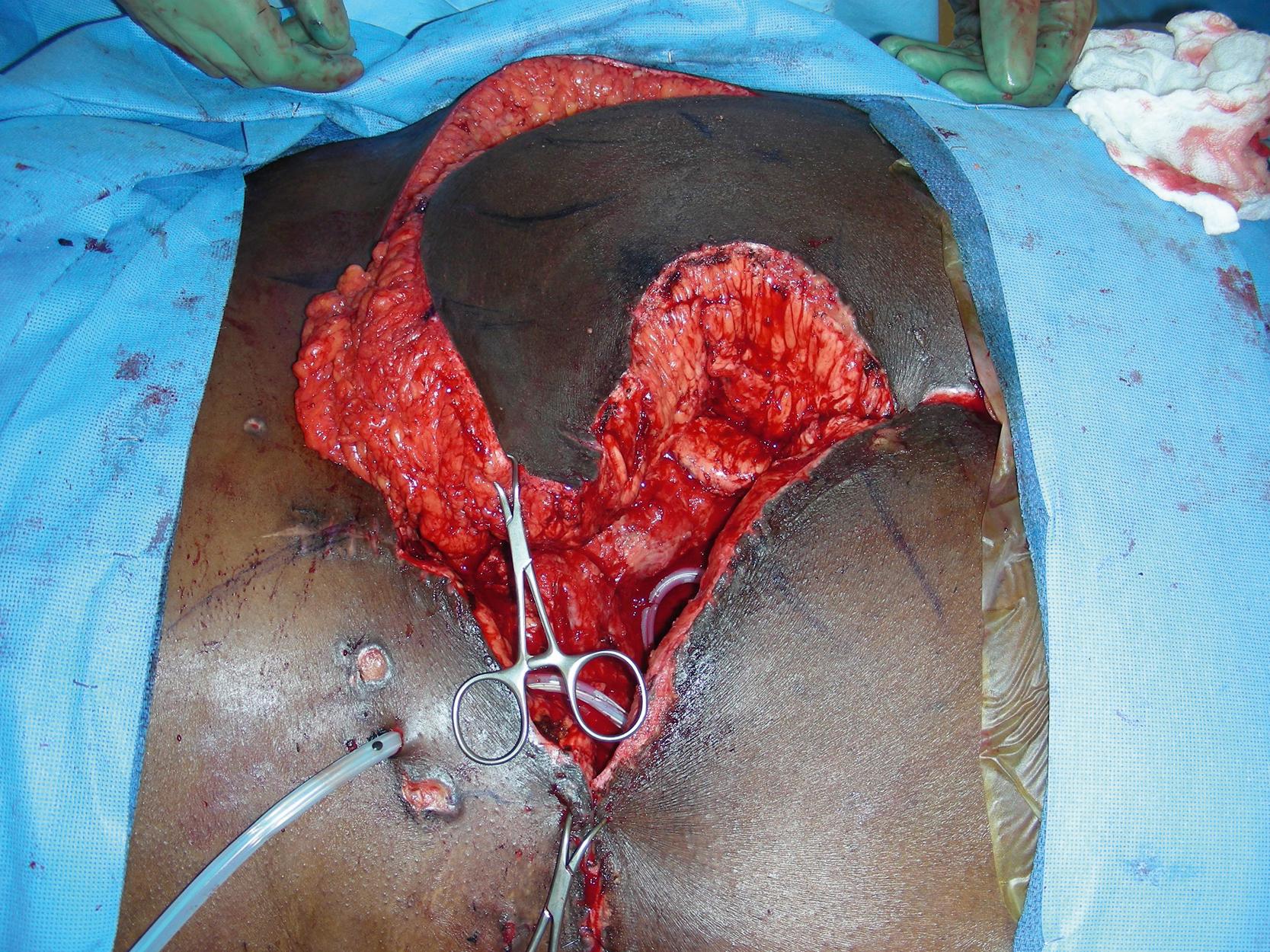
The flap elevation was started by making an incision through the skin, subcutaneous tissue, down to the subfascial plane. The subfascial dissection was performed to raise the flap ( Fig. 30.4 ). During the dissection, the perforator was identified and the flap elevation was performed based on this single large perforator. The flap was easily rotated and advanced into the defect ( Fig. 30.5 ). The flap donor site, measuring 30 × 10 cm, was approximated after the skin advancement from the nonflap side. A drain was inserted into the left pelvic cavity. Another drain was inserted under the flap. Six retention sutures were used to insure the wound approximation without too much tension. The entire flap closure was performed with interrupted 2-0 PDS sutures for the deep tissue closure and the subcutaneous tissue was closed with several interrupted 3-0 Monocryl sutures. The skin was closed with skin staples ( Fig. 30.6 ).

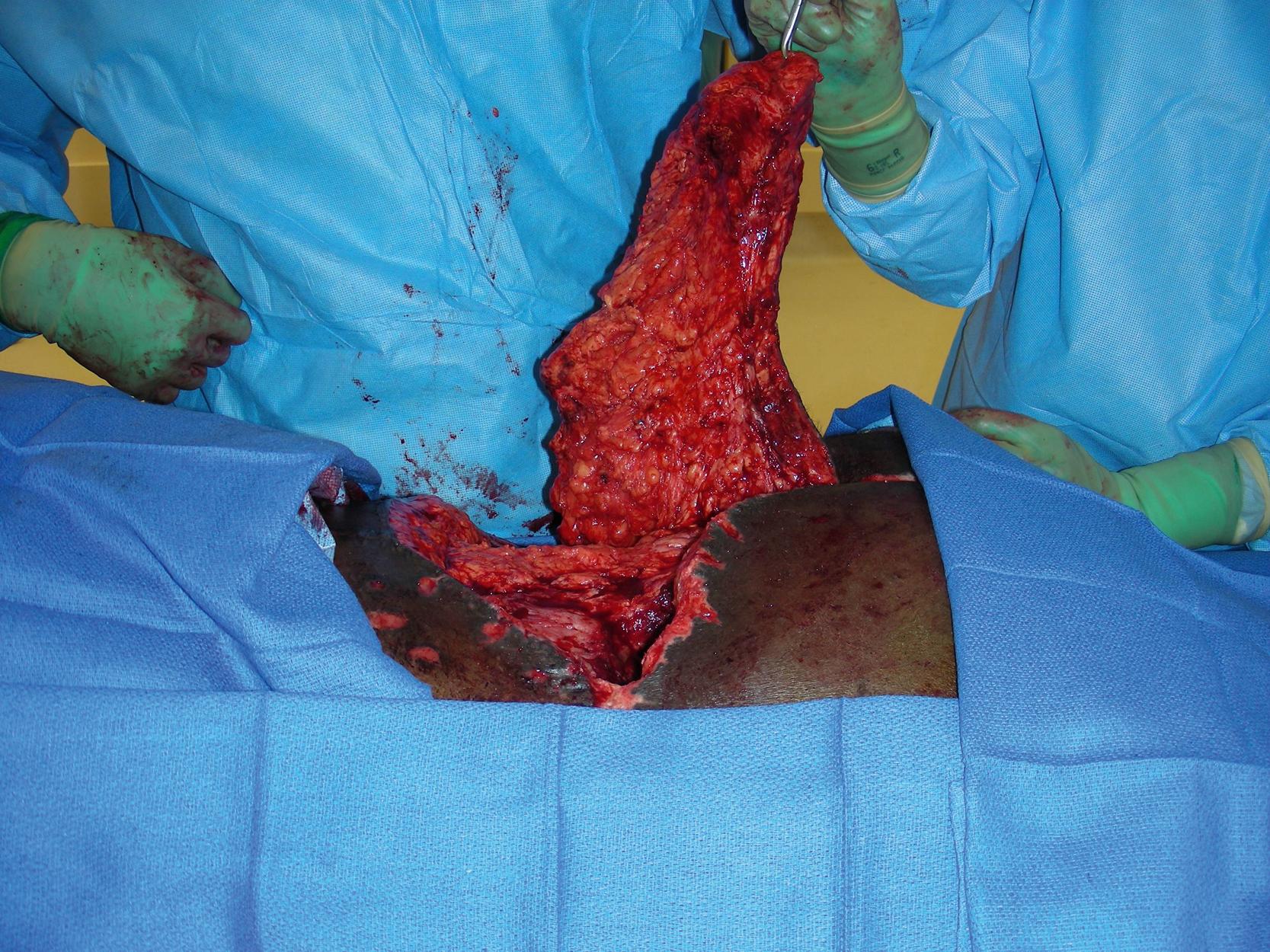
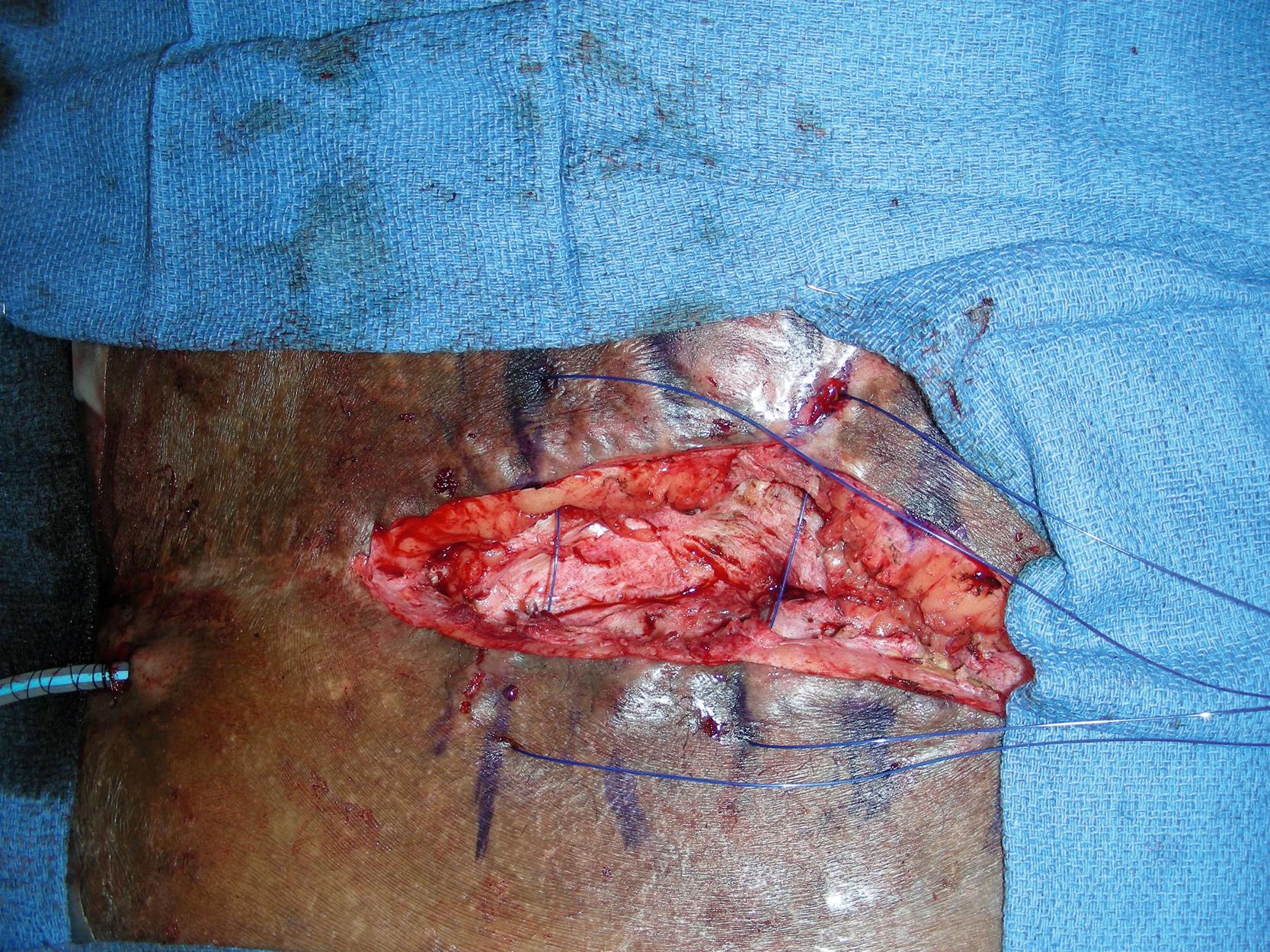
The patient developed partial wound dehiscence with potentially exposed hardware at postoperative 3 weeks ( Fig. 30.7 ). She was taken back to the operating room and all necrotic tissues were debrided ( Fig. 30.8 ). The large skin flap was re-elevated ( Fig. 30.9 ) and rotated and advanced into the defect without any difficulties ( Fig. 30.10 ). The flap site was closed again with the same sutures as the previous flap closure and retention sutures were again used ( Fig. 30.11 ).




She unfortunately developed additional skin edge necrosis during the following month and was taken back to the operating room for more debridement ( Fig. 30.12 ). The open wound was reclosed after some undermining and tissue rearrangement and retention sutures were again used ( Fig. 30.13 ).

Several days later, she developed more skin edge necrosis probably from a direct compression ( Fig. 30.14 ). She underwent another wound debridement and wound closure was performed again in the operating room ( Fig. 30.15 ).


After all surgeries and more than 2 months in-patient care, the lower back, pelvis, and gluteal wounds finally healed. The primary service was able to discharge her home. Unfortunately, she had a residual infection of the hardware and was taken back by the orthopedic oncology service for hardware removal and replacement ( Fig. 30.16 ). The plastic surgery service was asked to reopen the previous flap site and to re-elevate the flap for access to the left pelvis ( Fig. 30.17 ). During this procedure, the hardware inside the left pelvis was replaced. Some scar tissue over the previous flap site was excised and the open wound was closed again with the flap advancement and placement of retention sutures ( Fig. 30.18 ).



After multiple operative procedures including the flap re-elevation for new hardware replacement, the lower back, pelvic, and sacral wounds finally healed ( Fig. 30.19 ). During the subsequent follow-up visits, there was no evidence of recurrent infection and the flap reconstruction site healed well with minimal scarring and good contour ( Fig. 30.20 ). The patient has resumed her normal activities and been followed by the primary service for routine follow-up.


Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here