Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since the advent of endoscopic sinonasal surgery, we have continued to see rapid growth and expansion of endoscopic techniques used for a variety of other indications. We first began to see this demonstrated after comparing traditional transcranial approaches versus novel endoscopic approaches for repair of anterior cranial fossa cerebrospinal fluid (CSF) leaks. Certainly, when novel technology and operative techniques for addressing an underlying problem arise, they should, at a minimum, provide equal, if not better, outcomes. Multiple studies have since demonstrated comparable outcomes between open transcranial and endoscopic transnasal approaches. A systematic review from 2013 incorporating 71 studies and 1178 patients demonstrated equivalent success rates in repair of anterior cranial fossa CSF leaks between these two approaches. In addition, endoscopic approaches offered significantly lower complication rates than open approaches, including rates of meningitis (3.9% vs 1.1%), abscess or wound infection (6.8% vs 0.7%), and sepsis (3.8% vs 0%). Other studies have reinforced these findings of successful equivalence while also providing improvement in patient outcomes. That has been shown not only with postoperative complications but also in relation to shorter duration of hospitalization, decrease in cost of health care, and an increase in overall patient satisfaction.
As endoscopic approaches then expanded for other indications, there were notable changes in postoperative CSF leak rates as the size of the resulting skull base defects enlarged. Notable risk factors for postoperative CSF rhinorrhea included the size of the dural defect; intraoperative grade of CSF flow; and in some instances, location of the defect. , In many cases, these factors go hand in hand with each other when referencing repair of defects created during tumor resection. Free mucosal grafting, even when done in multiple layers, was associated with higher rates of failure. Harvey et al. demonstrated this nicely in a recent meta-analysis with 609 patients, showing postoperative CSF leak rates at 15.6% for those patients treated with free grafting.
The advent of the nasoseptal flap (NSF) was a transformative event in skull base reconstruction. Details regarding the history and development of the NSF for use in reconstruction can be found in the previous chapter. For the purposes of this chapter, the NSF cemented the idea that vascularized reconstruction provides ample tissue and improves overall patient outcomes. As discussed with the previously mentioned systematic review and meta-analysis, free grafting of large dural defects yielded postoperative CSF leak rates greater than 15%. The addition of vascularized tissue reduced the rate to 6.7%. High-volume centers have since demonstrated even greater reductions in postoperative CSF leaks with the addition of vascularized reconstruction. This includes large dural defects associated with high-flow leaks or communication with CSF cisterns.
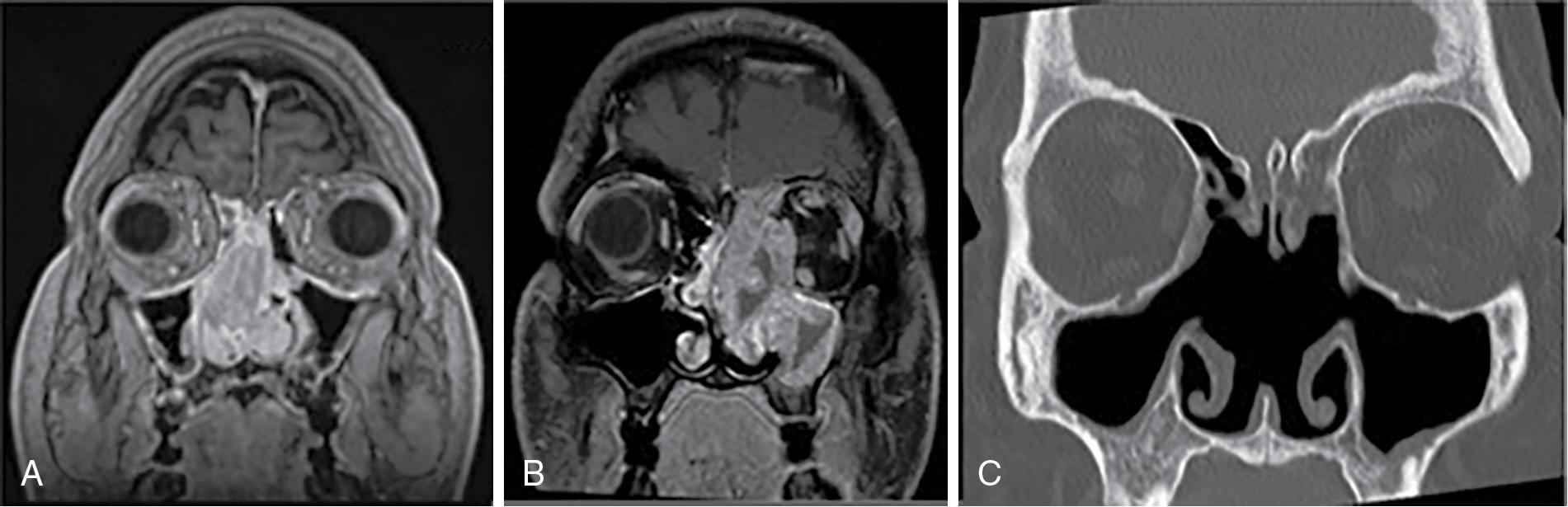
The NSF has repeatedly demonstrated its superiority to free grafting when addressing large defects. However, there remain occasions when the NSF is unavailable for skull base reconstruction ( Fig. 30.1 ). This can be from a variety of reasons, including previous surgery or trauma, tumor involvement, or perhaps the size or location of the defect. When unavailable, secondary vascularized flap options are available to use, both intranasal and extranasal. Vascularized tissue can be particularly important when addressing malignancy or other tumor pathology in which adjuvant radiotherapy may be a consideration. This chapter reviews some of these options for other locoregional vascularized flaps.
The NSF is based off the posterior septal branch of the sphenopalatine artery. There are other branches of the sphenopalatine artery that provide vascular supply to the structures of the lateral nasal wall. As such, many of these lateral nasal wall structures can be pedicled to their primary branching points distal to the sphenopalatine foramen. This primarily includes the middle turbinate and inferior turbinate flaps. The inferior turbinate flap can be widened to incorporate some of the mucoperiosteum along the frontal process of maxilla or the nasal floor, and this is often referenced as the lateral nasal wall flap or extended inferior turbinate flap.
The middle turbinate flap is a pedicled flap of mucoperiosteum based off the middle turbinate branch of the sphenopalatine artery. Many cadaveric and anatomic models have been reported and described to demonstrate its length and utility in skull base reconstruction. , Primarily, it can be an alternative option for reconstruction of the sella, planum, or posterior ethmoid skull base.
Variation in harvesting technique has been described, but ultimately, this involves a vertical incision within the anterior head of the middle turbinate. A releasing incision is also required along the medial mucosa as it extends posteriorly toward its attachment near the lateral nasal wall. After these incisions have been made, the flap is elevated in a submucoperiosteal fashion, taking care to leave the bony attachments as best as possible. There are sagittal, coronal, and oblique planes to the middle turbinate, and its three-dimensional anatomic configuration can make this portion of the procedure quite demanding technically. With the mucosa elevated, the bone of the middle turbinate is gradually removed all the way back toward the sphenopalatine foramen. The foramen can be dissected out as well toward the pterygopalatine fossa or infratemporal fossa if increasing length is desired.
The advantages of the middle turbinate flap include vascularized tissue in close proximity to the posterior ethmoid skull base, planum, and sella. Its primary arc of rotation is very similar to that of the NSF. In theory, this flap would be used quite often for defects at this location, but there are many drawbacks. Primarily, this flap remains quite challenging to harvest compared with other intranasal flap options. The middle turbinate itself is not particularly rigid, and elevation is fraught with frustration. In addition, the length available from this flap is not robust, and its arc of rotation limits its utility along the cribriform plate and clivus. Anatomic studies have demonstrated the average length is a little over 4 cm, with a surface area of approximately 5 cm 2 . As a comparison, the NSF provides approximately 25 cm 2 of vascularized tissue on average.
Although it should not be dismissed, the middle turbinate flap is often reserved for small sellar and parasellar skull base defects when the NSF is unavailable. It can also be used as a secondary flap to augment free grafts along the middle and posterior cranial fossa to aid in revascularization and epithelialization and improve wound healing.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here