Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The differences in skin texture and laxity with age must be considered when choosing a local flap for facial coverage.
The plastic surgeon’s goal is not to cover a facial wound, but instead to reconstruct the characteristics of the missing tissue.
Survival of random flaps depends on perfusion pressure and on intravascular resistance of the region of skin being used and not on set length-to-width ratios.
Local facial flaps design ensures adequate vascularity and places the secondary defects in areas of relative tissue excess or maximum skin extensibility.
Wound tension is minimized so that both the primary and secondary movements in flap transfer do not distort facial landmarks.
Ideally, all incisions lie at the borders of subunits.
Flaps can be classified by the nature of their blood supply, by configuration, by their anatomic location, or by their method of transfer.
The chapter describes established local flap options based on anatomic location and following 10 basic principles for successful design and transfer.
Access video and video lecture content for this chapter online at Elsevier eBooks+ ![]()
![]()
“The delineation and manipulation of skin-flaps constitute the ABC of the plastic surgeon’s métier .” Harold D. Gillies, Plastic Surgery of the Face
There is no substitute for local tissue in facial reconstruction. Skin from outside of the cervicofacial area is a poor aesthetic substitute. The reconstructive surgeon must therefore master judicious use of this finite resource. Many authors have described the use of local flaps to reconstruct defects following excision of the skin malignancies commonly seen in the older Caucasian population. The reader should be reminded, however, that during the birth of modern plastic surgery, amidst the horrors of World War I, local facial flaps were devised for ballistic injuries to the face and only later adapted to various clinical scenarios beyond the traumatized faces of infantrymen. Aside from post-Mohs reconstruction, local flaps have tremendous utility in the revision of the vertically deficient bilateral cleft lip repair; reconstruction after excision of benign lesions such as involuted hemangiomas and nevi; secondary burn reconstruction, and of course traumatic defects, whether produced by knife, gun, animal, or motorized vehicle.
Age and sex are critical components that must be accounted for, specifically in terms of the quality of the patient’s skin. Many flaps and their donor scars that might look good in a 70-year-old, may be aesthetically unacceptable in a child or young woman.
Two key distinctions between older and youthful skin are texture and laxity. The surface of old skin, with its rhytids (both static and dynamic), relative loss of hydration, degenerative solar elastosis, and, in the male, beard growth has a coarse, uneven texture that more easily conceals incisions amongst abundant areas of light, shadow, and facial expression. In addition, deflation and ptosis of fat compartments can exaggerate the convexities and concavities of the face by, for example, deepening the nasolabial folds, marionette lines, and prejowl sulci, thus providing additional hiding places for the placement of incisions and donor scars.
This is, of course, not the case for the younger patient. Placement of incisions at the borders of aesthetic subunits is of even greater importance, relegating certain flaps, such as lip reconstruction using the Karapandzic method, to be used only in aged or coarsened skin. Skin laxity is the other key distinction. Gillies and Millard advised to “Borrow from Peter to pay Paul only when Peter can afford it.” A local flap must borrow from an area of relative excess that is immediately adjacent or regionally adjacent to the defect. Thus, the laxity of tissue seen in older skin allows for more “donor material” as opposed to the taut skin of the young. What may be seen as redundant tissue to be discarded in aesthetic patients can represent precious building material in the individual undergoing reconstruction. Thus, with age, Peter acquires the wealth with which to finance Paul.
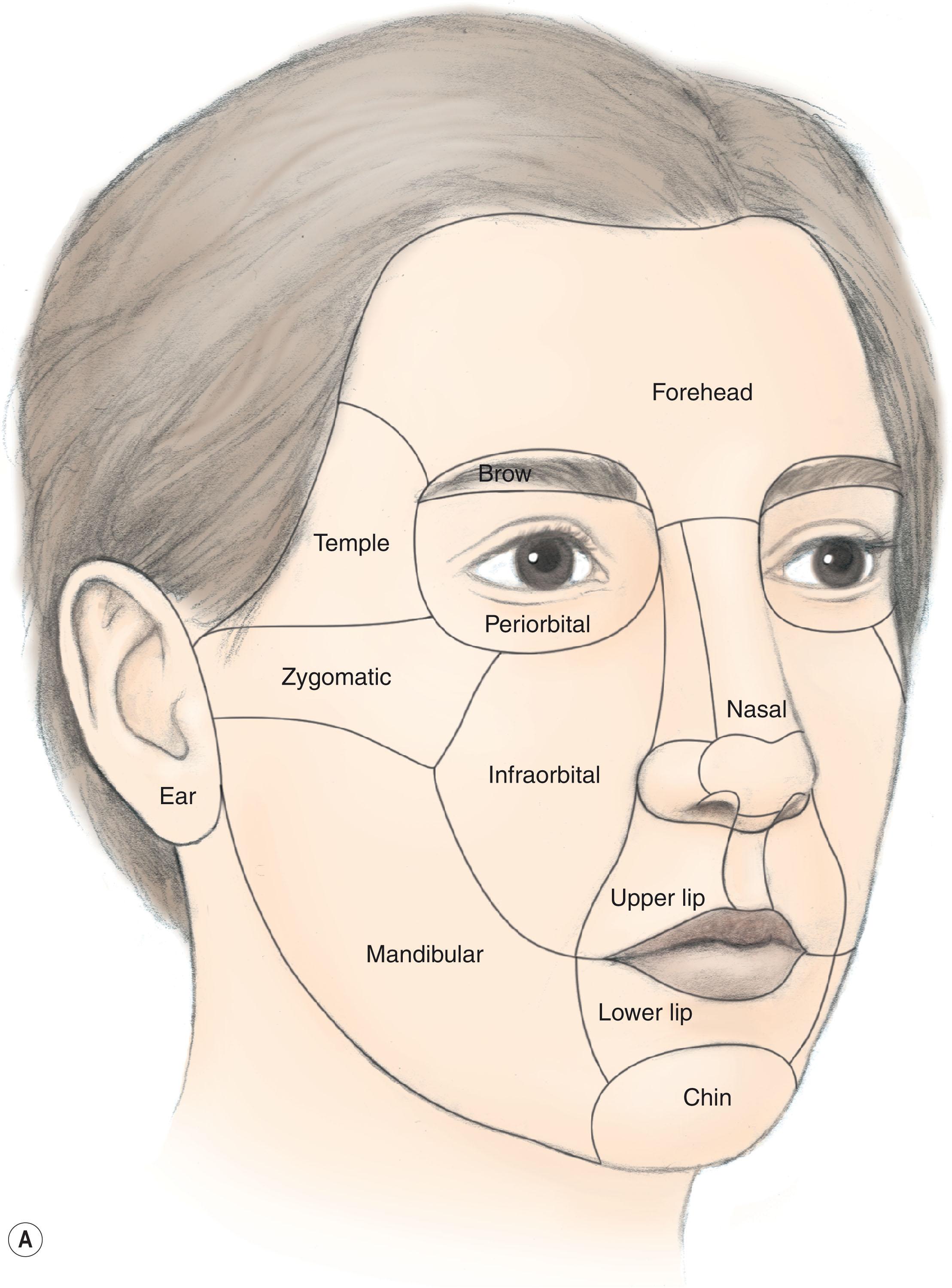
The plastic surgeon must understand that a healed wound on the face is not the primary goal. Wound closure is only a means to a greater end. Plastic surgeons do not simply “fill” defects of the face. Plastic surgeons reconstruct the face. To this end, regardless of patient age, reconstruction must utilize the concept of aesthetic subunits of the face. The subunit borders are naturally occurring demarcations where the human eye expects changes in contour and projection such as the nasolabial fold, the lid cheek junction, the alar crease ( Fig. 10.1 ). It is in these areas where incisions can be best hidden. When reconstructing the primary defect and closing the donor site, the surgeon must also be cognizant to avoid distortion of landmarks . Donor sites must borrow from areas of relative laxity adjacent to the primary defect and potentially away from landmarks. Failing to do so may asymmetrically elevate an eyebrow, transpose a sideburn, cicatrically increase scleral show, or unintentionally peak the white roll of the lip.
Gillies stated that “The plastic surgeon must early acquire an instinct for forecasting the viability of the flaps he uses.” Instinct and trial and error have since been supplemented by anatomical science and physiology, particularly with the detailed work on microvascular anatomy by Ian Taylor and colleagues. The blood supply to the skin of the face is arguably the most robust of anywhere in the body. It serves two vital functions: nutritional support and thermoregulation. Primarily because of its thermoregulatory function, the rate of blood flow through the skin is also the most variable in the body. At room temperatures, the volume of blood flowing through the skin (0.25 L/m 2 of body surface area) is approximately 10 times the flow required for nutritional support. In addition, blood flow can increase up to seven times with maximal vasodilatation. These phenomena are made possible by the complex neurovascular architecture of the skin. The same vascular system the body uses to increase blood flow during vasodilatation is harnessed by the plastic surgeon to enhance the perfusion of flaps. The act of flap elevation is an inherently ischemic process to the surgically manipulated skin. Myers commented that “fresh flaps are always both viable and ischemic”. Flaps owe their survival to the difference in the blood flow needed to nourish the skin versus that for thermoregulation. There are, of course, limits to survival when this difference is exceeded.
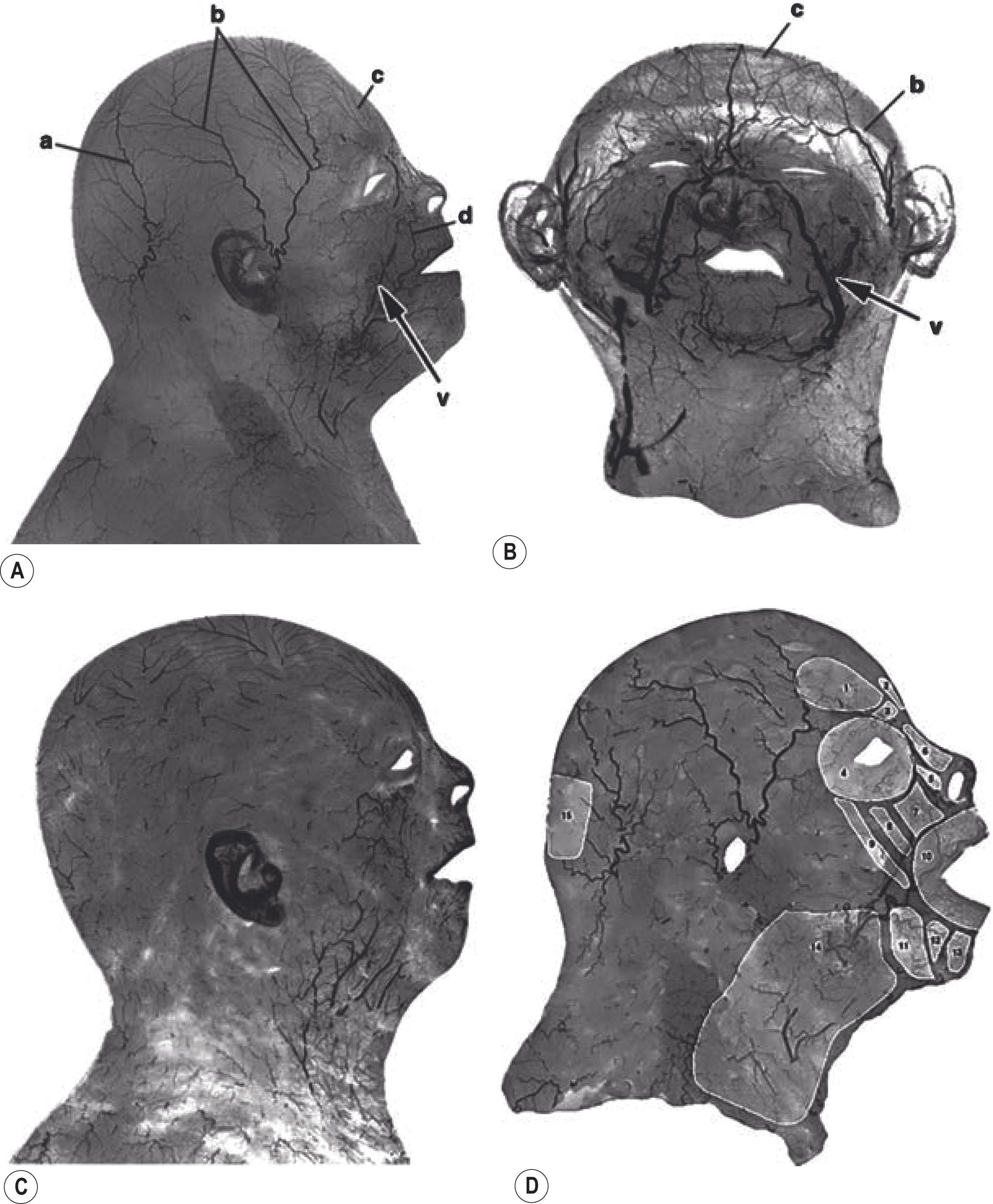
Local flaps for facial reconstruction mostly rely on the subdermal plexus and are thus categorized as “random pattern” flaps. Earlier attempts to raise consistently perfused random pattern flaps in the body posited certain length-to-width ratios. Differing ratios were given for various areas of the body which in turn hinted to regional variation in the blood supply in different areas of the body. Milton subsequently disproved the concept of length:width ratios as viability depended more on the extent of circulation. Survival of random flaps instead depends on perfusion pressure and on intravascular resistance of the region of skin being used for reconstruction. Ian Taylor’s group gave plastic surgery tremendous insight into flap physiology with the anatomical concepts of “choke” vessels and angiosomes. Their anatomical studies indicated the reasons for differences in cutaneous intravascular resistance across the entire body. They were able to explain why the face is indeed a privileged area of arterial perfusion, given the rich anastomotic latticework in the SMAS (superficial muscular aponeurotic system) layer in addition to a dense subdermal anastomotic plexus, particularly in the “blush” area of the cheeks and anterior neck ( Fig. 10.2 ). Prior work on the venous system revealed that face and scalp skin have a paucity of valves, thus explaining the improved venous drainage of facial skin. This insight into venous anatomy is of particular importance as venous occlusion is likely more damaging to flap survival than inadequate arterial supply.
Gillies stated that “Essentially, all flaps are similar and consist of two parts – the part chiefly concerned with the traffic of circulatory fluids, and the part available for plastic use.” A flap is basically a tongue of tissue. The pedicle of a flap is the portion of the flap responsible for providing vascularity to the flap whilst the skin paddle is the portion used to reconstruct the defect. The difficulties encountered in local flap reconstruction, as opposed to free flaps, is that the skin paddle, donor site, and recipient site are all in close proximity to one another and its reach is constricted by its own pedicle.
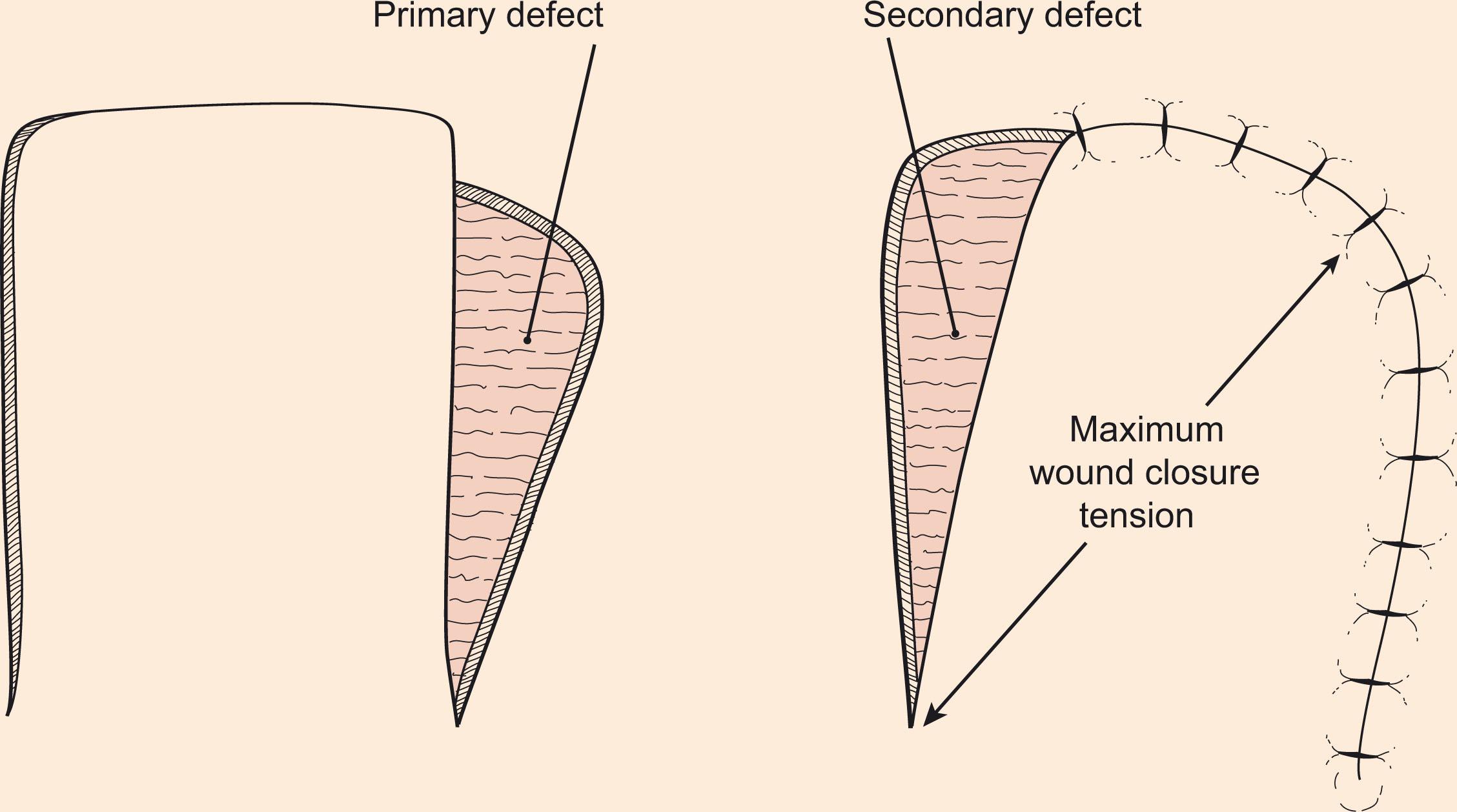
The primary defect is the wound that is to be closed by a local skin flap ( Fig. 10.3 ). The secondary defect is the wound created at the donor site when the local flap is transferred to the primary defect. Therefore, one of the challenges in local facial flap reconstruction is to design a flap that places the secondary defect in the most aesthetically advantageous location. This typically translates into elevating flaps from areas of the face and neck with greater skin laxity and away from fixed facial landmarks.
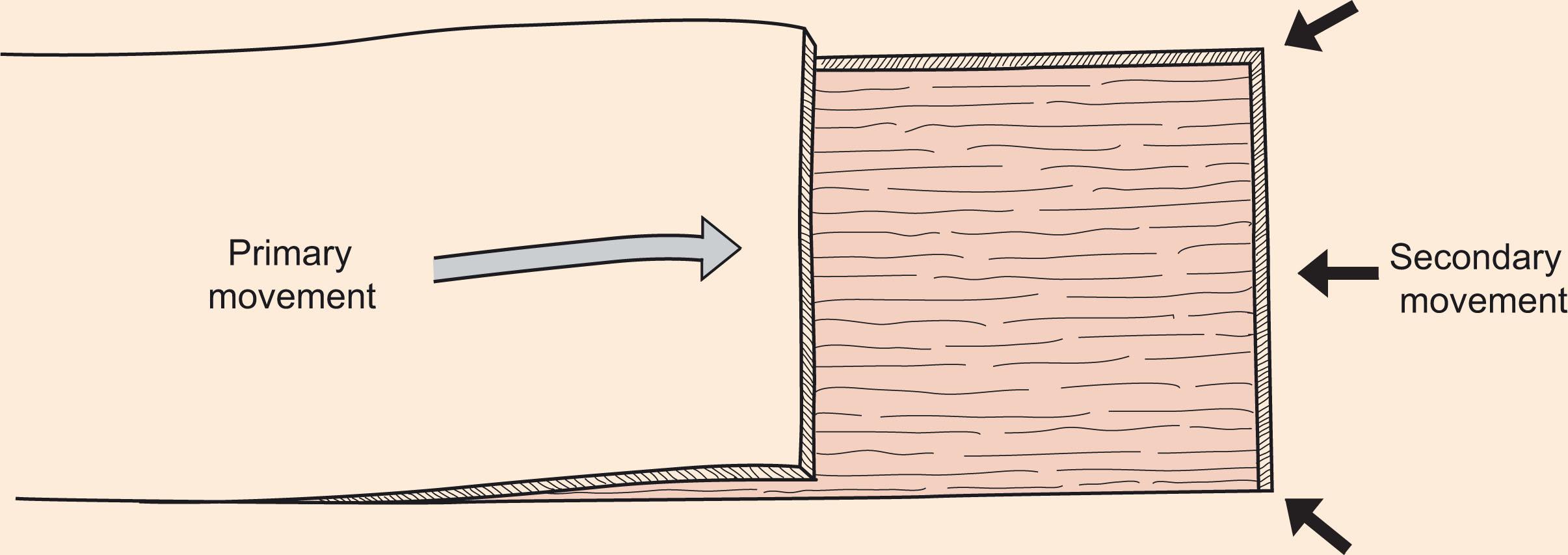
Primary tissue movement is the motion of a local flap when it is transferred to the defect ( Fig. 10.4 ). This is done by either advancing the flap along its length or pivoting it about its pedicle. Secondary tissue movement is the displacement of skin surrounding the primary defect directed towards its center. The vector of secondary tissue movement is usually opposite the vector of primary tissue movement. There is of course additional movement during donor site closure. Thus, a combination of both primary and secondary tissue movements occurs in the successful closure of a wound by a local flap. An additional challenge to local flaps is when the primary defect occurs near a mobile landmark (lower eyelid, ala, eyebrow etc.): the surgeon must design a flap that minimizes distortion of landmarks either by secondary movement or by closure of the donor site.
Wound closure tension is the amount of stress along the suture line of a repaired wound. If the tension is too great, the adjacent structures will become distorted, and the resulting scar unnecessarily widened or prominent. The degree of tension is related to the vectors of primary and secondary movement. Placing the secondary defect in an area of greater laxity can mitigate closure tension. Tension can also affect vascularity of the flap where it is inset into the most distant aspect of the defect. Just as in free flap surgery, the surgeon must assess whether the method of inset is consistent with flap vascularity. The skin can accommodate some degree of acute stretching and this extensibility is referred to as mechanical creep . Mechanical creep results in reduction of wound closure tension over a short period of time (intra-operatively) as tension is reduced when skin is held under a constant strain for several minutes.
Thus, the challenges are to design local facial flaps of adequate vascularity, placing the secondary defects in areas of relative tissue excess or maximum skin extensibility. Wound tension is minimized so that both the primary and secondary movements in flap transfer do not distort facial landmarks. Ideally, all incisions lie at the borders of subunits.
Flaps can be classified by the nature of their blood supply (random vs. axial vs. perforator), by their configuration (rhomboid, bilobe), by their anatomic location (cheek, forehead, lip), or by their method of transfer (free or pedicled). For local facial flaps, classification by method or transfer or movement, remains the most convenient. The two basic categories are pivotal and advancement flaps ( Table 10.1 ). Advancement flaps rely on stretching flap skin in the direction of the primary defect and as such are subject to increased wound closure tension. Pivotal flaps, in contrast, rotate about a point at their base and, in their purest form, need not be stretched and although they are thus not subject to increased wound closure tension, the donor site of the flap may be. In most circumstances, most pivotal flaps attain wound closure via a combination of pivoting in addition to advancement.
| Pivotal | Advancement |
|---|---|
| Rotation | Unipedicle |
| Transposition | Bipedicle |
| Interpolated | V–Y and Y–V |
| Island | Island |
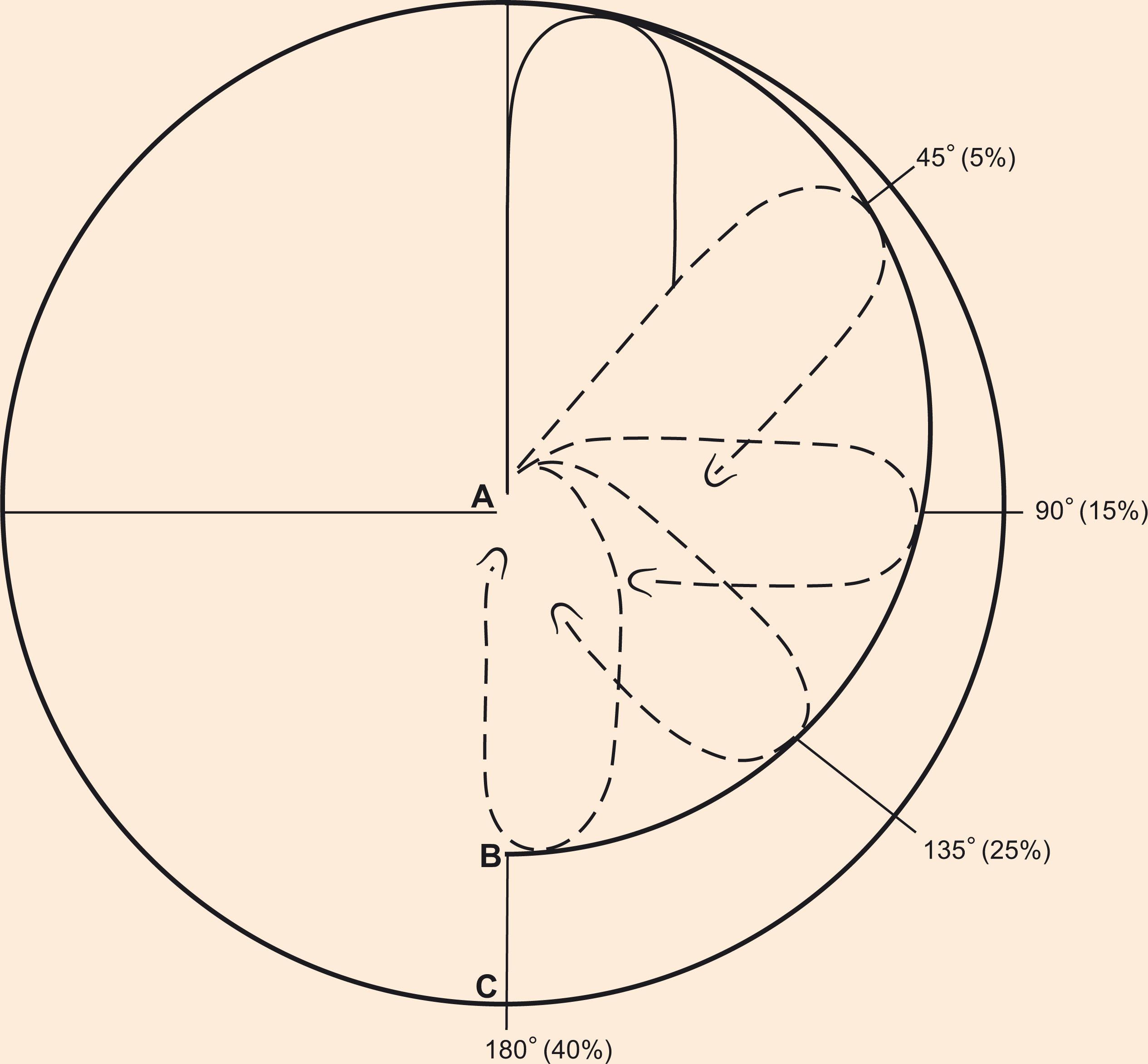
Four types of pivotal flaps exist: rotation , transposition , interpolated , and island . The common trait amongst these flaps is that they reach the defect by pivoting at a fixed point: the pedicle. Critical in designing flap length is the realization that there is an increasing reduction in effective length with greater degrees of pivot ( Fig. 10.5 ). Pivoting a flap 45° results in a 5% loss of length; 90° loses 15%, and 180° loses 40%. It should be noted that the common technique of using gauze or silk tie to determine sufficient length upon pivoting may yield false information since neither of these fabrics bunch up at the pedicle as skin would to thereby restrict length upon rotation. This bunching of the pedicle is a standing cone (dog ear) and the size of the deformity increases in proportion to the degree of pivot. Thus, a flap’s arc of pivot should generally not exceed 90° whenever possible. The exceptions to these limitations would be an island flap, whose pedicle is skeletonized to its feeding vessels, or a narrowly based axial flap such as a paramedian forehead flap.
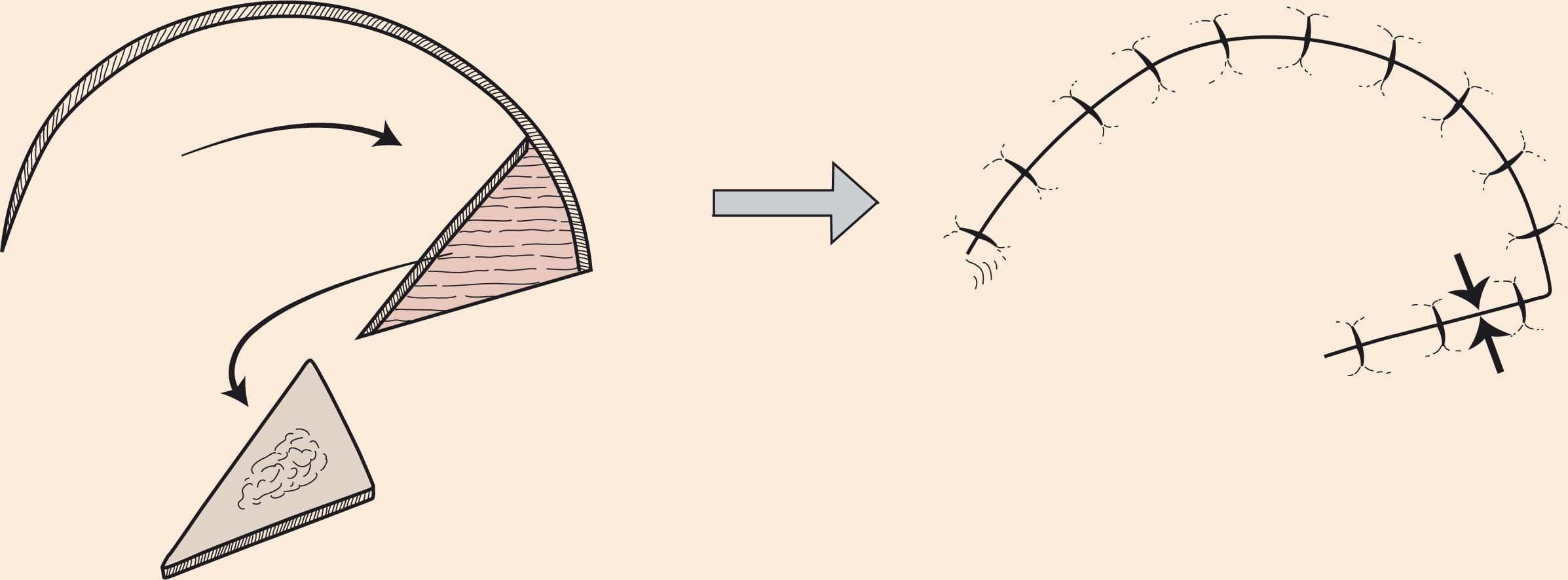
When designing a rotation flap , the surgeon should triangulate the defect making the shortest dimension the base of a triangle ( Fig. 10.6 ). This base then forms part of the circumference of a circle. The flap is designed in an arc so that the leading tip will rotate around the circumference on which the triangular defect lies. The radius from the apex of the triangle to the end of the arc constitutes the pedicle. As a rule, in flap design, the length of the arc should be 4–7 times the defect width. Modifying the defect to a triangle with a height-to-width ratio of 2:1 avoids a standing cone. The height of the defect should be 50–100% the radius of the flap curvature. The area of greatest wound tension is usually along a line from the leading tip of the flap to the most distal point of the arc, which acts as the point of rotation. A back cut reduces this tension by moving the point of rotation closer to the defect.
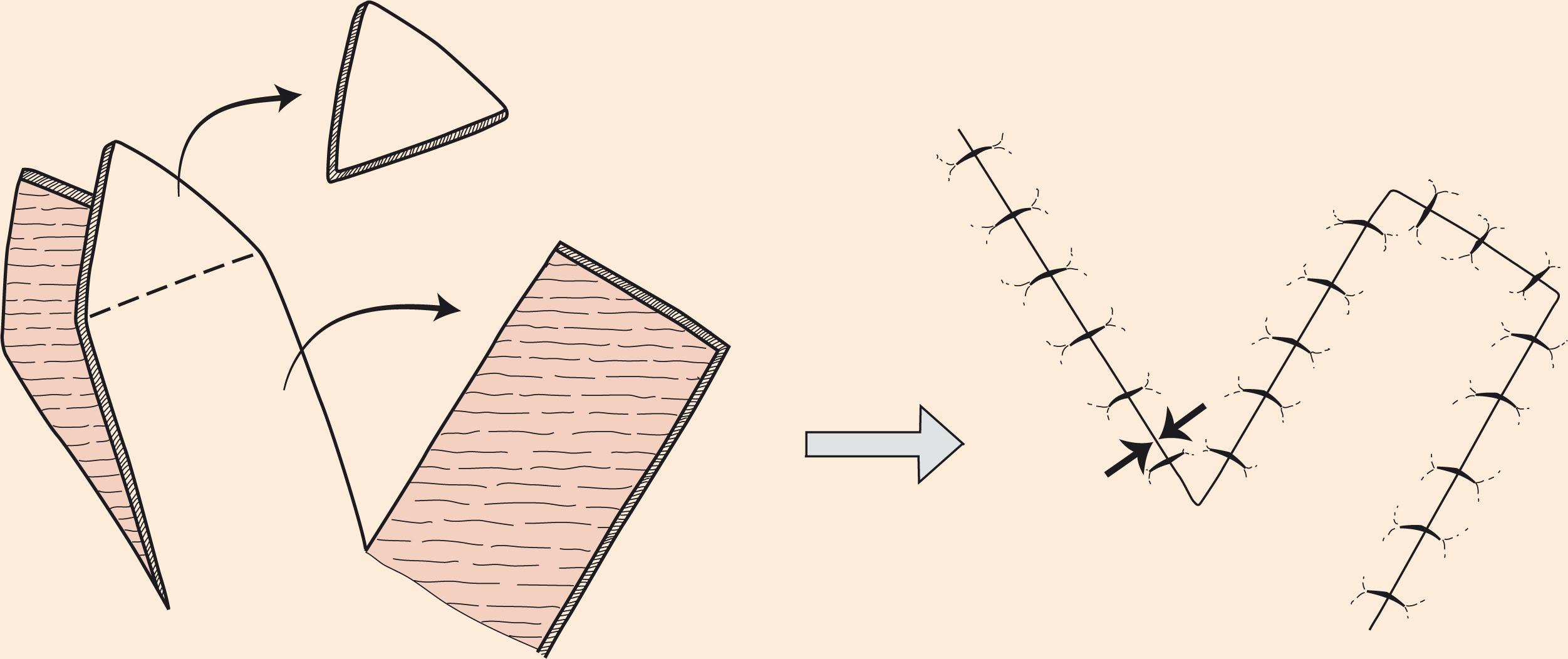
Transposition flaps are designed with a more linear configuration than rotation flaps and can also have a reduction in effective length due to the standing cone that forms as they pivot at their base ( Fig. 10.7 ). While they may be immediately adjacent to their defect, they may also only have the base contiguous with the defect requiring the flap to travel over intact skin. This allows the harvest of the flap some distance from the defect in an area of more skin laxity/redundancy. In addition, the ability to recruit skin at some variable distance may allow placement of donor site incisions within aesthetic boundaries. Transposition flaps are the most common local flaps for head and neck cutaneous defects. Rhomboid and bilobed flaps are key examples.
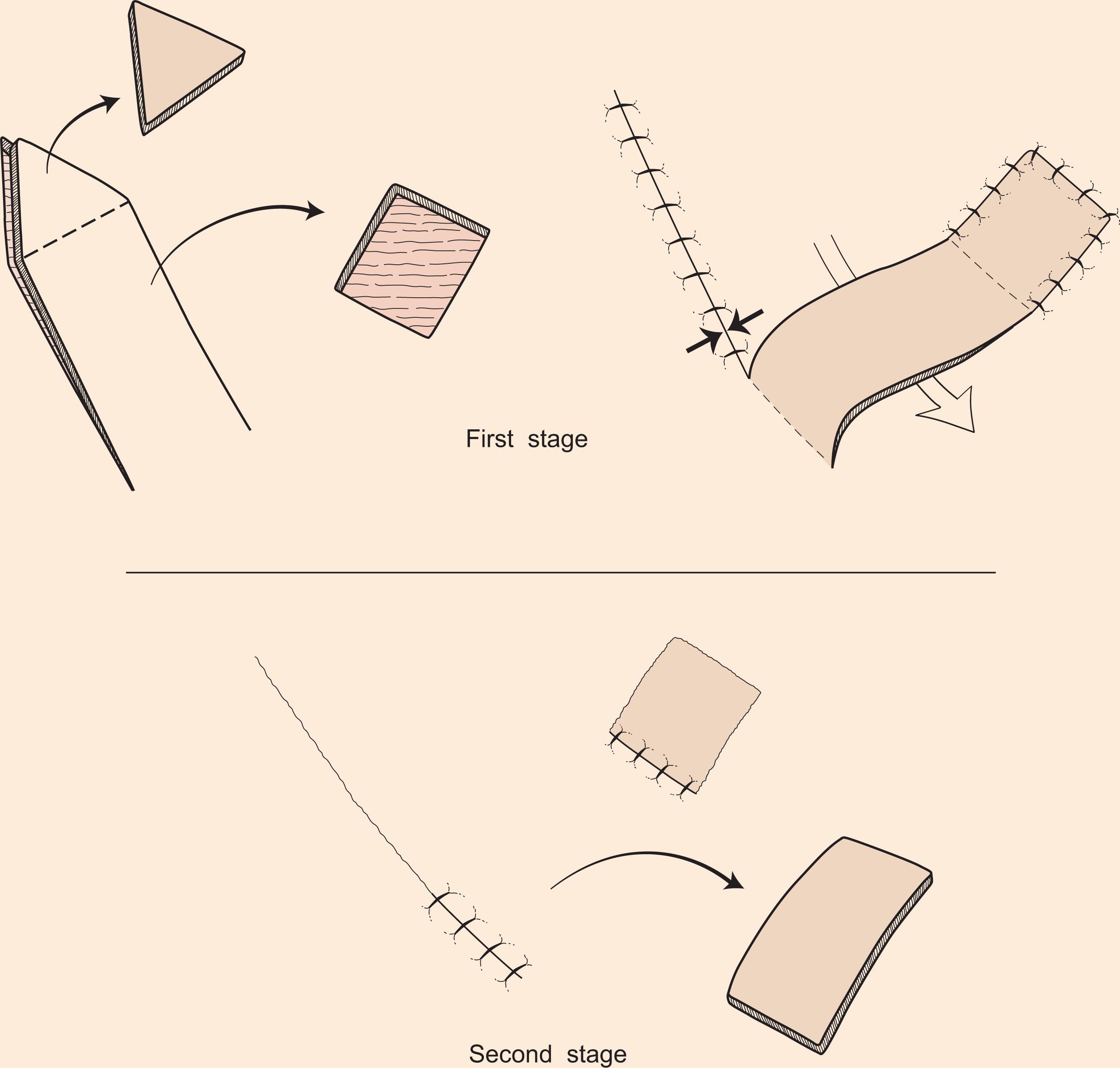
Interpolated flaps differ from transposition flaps in that their donor is not contiguous with the defect at all, neither by the skin paddle nor the pedicle ( Fig. 10.8 ). The pedicle may need to pass over intervening tissue and if so must be divided in a second surgical procedure. While the necessity of a second stage may be seen by some as a disadvantage, this may allow thinning of the flap and sculpting tissue at the recipient site as in a three-stage forehead flap for a nasal defect. The advantages of a distant donor site seen with transposition flaps are even more so with interpolated flaps. The paramedian forehead flap and the nasolabial flap are the most common interpolated flaps used in the face.
Island flaps are so named as they are incised on all borders and thus bear no cutaneous attachments between the flap skin and the donor site. The pedicle is from the subcutaneous tissue or perforating vessels. As such, island flaps can be both pivoted or advanced. Pivoting island flaps are most frequently designed off perforators found at the nasolabial fold.
As opposed to pivoting, all advancement flaps “slide” towards the defect and thus must also be immediately adjacent to it. Tissue transfer involves stretching of the skin flap and its pedicle along a single vector. Given their movement, these flaps are best used in areas of greater skin elasticity. The most rudimentary advancement flap is actually a simple layered closure where either side of the skin is undermined. Advancement flaps may be categorized as unipedicle , bipedicle , V–Y , Y–V , and island . Except for V–Y and island flaps, all advancement flaps (even layered closure) will result in two cutaneous standing cones on either side of their base. Removal of these “Burow’s triangles” facilitates even advancement of the flap. In contrast, pivotal flaps result in only one standing cone.
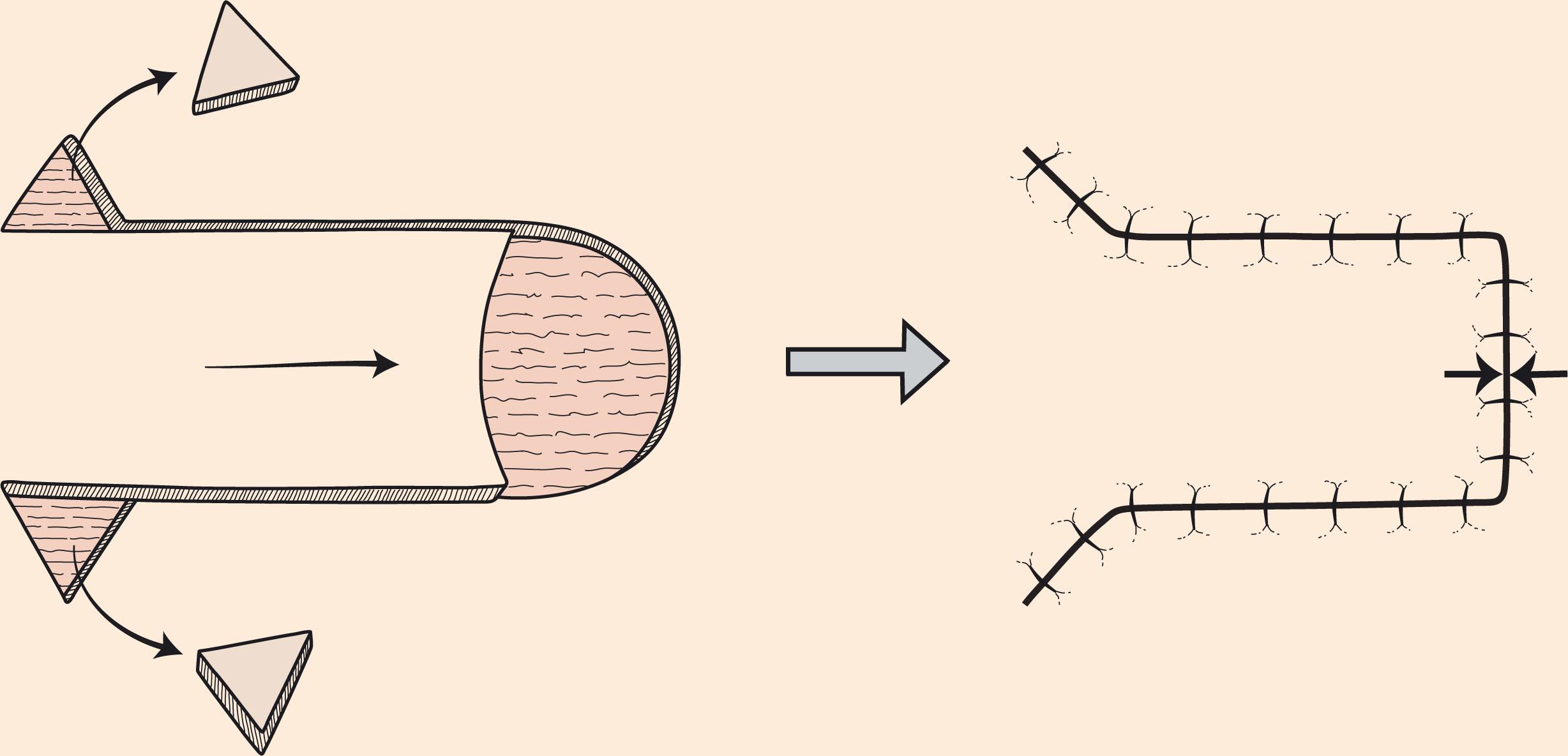
Unipedicle flaps are formed with the leading edge of the flap immediately adjacent to the defect and then flanked by parallel incisions to allow direct advancement into the defect ( Fig. 10.9 ). The repair involves both primary and secondary tissue movement and thus undermining not only the skin paddle but the surrounding skin is necessary to facilitate transfer. The move results in two standing cones at the base that can either be excised or the redundancy of the surrounding skin can be worked out with sutures. Both unipedicle flaps and rotation flaps see a discrepancy between the length of the flap and the edge of the wound within which it moves. In both flaps, Burow’s triangles can be planned to “shorten” the length of the wound. When bilateral unipedicled flaps are used, an “H” or “T” repair will result, commonly referred to as “H-plasty” or “T-plasty”. Unipedicled flaps have great utility for defects of the medial cheek, above the hair-bearing brow, and of the helical rim.
Bipedicled flaps are designed adjacent to the defect with the flap’s long axis perpendicular to the direction of advancement. This results in a secondary defect that may require a skin graft, thus limiting its use in the face. It does have utility, however, in limb reconstruction.
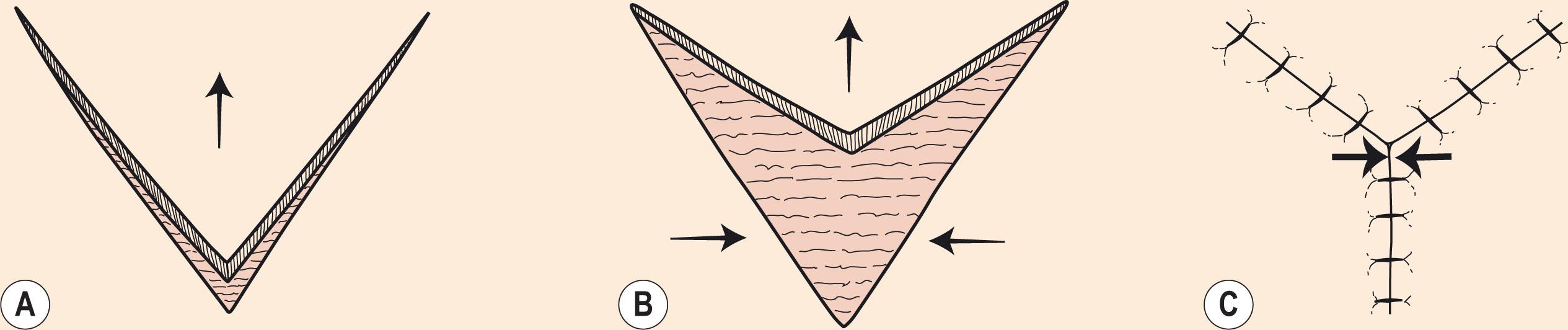
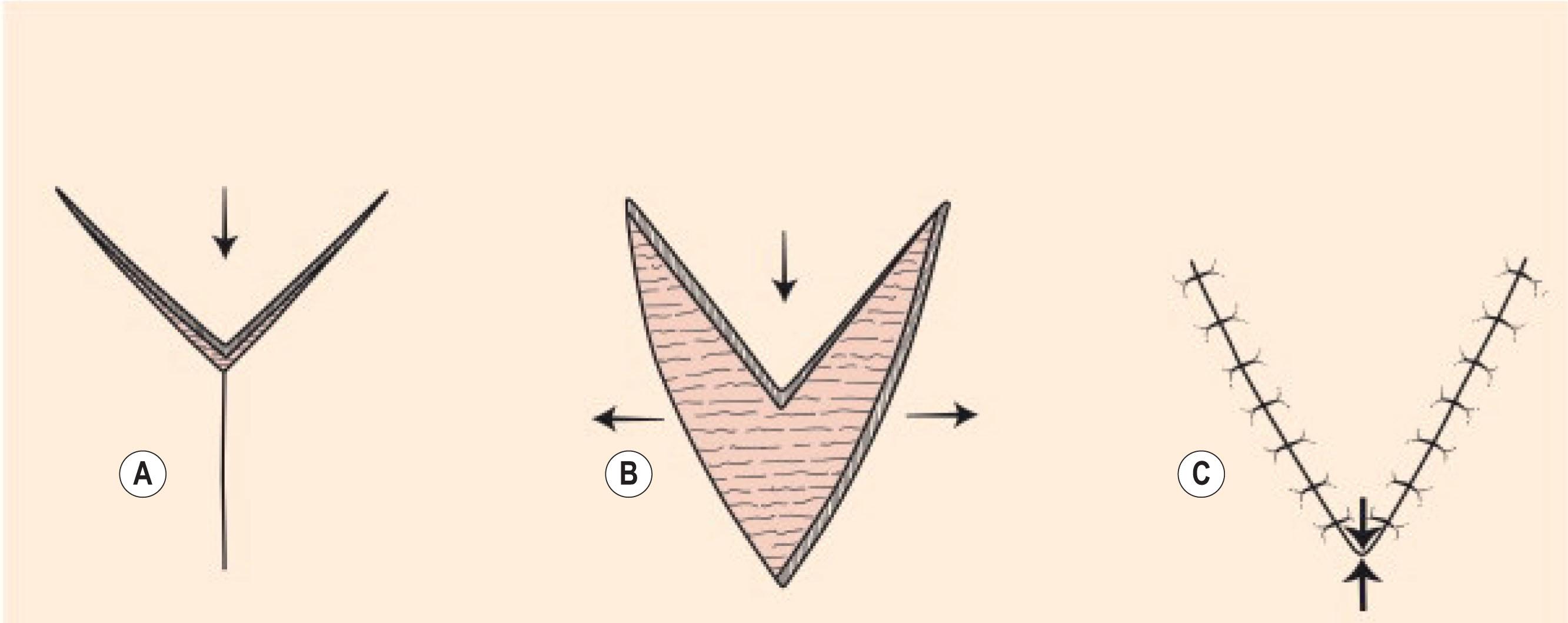
Both V–Y and Y–V flaps see their greatest utility in corrections of distorted landmarks of central facial features (eyelids, nose, lips) from scar contracture. With the V–Y advancement flap, the fork of the V is pushed forward by way of closing its donor site behind it, thus converting the apex of the V to a Y ( Fig. 10.10 ). This movement is therefore nearly tension-free. In contrast, the Y–V flap pulls the crotch of the Y segment into its central limb with the resulting closure forming a V ( Fig. 10.11 ). Consequently, there is tension seen at the apex of the V closure. An example would be medializing the lateralized ala on the cleft side in a unilateral incomplete microform cleft lip. Both flaps are best designed within creases or aesthetic borders.
The following description of local flaps for facial cover is not meant to be encyclopedic – many flaps will be excluded – but it will provide a working template for the reconstruction of such defects with the most suitable and well-established options in modern plastic surgery.
This chapter is organized according to anatomical region but there are 10 common principles that apply to most facial flaps:
Skin elasticity and mobility should be assessed by pinching it between index and forefinger to assess the availability of local tissue. With severe solar damage and following radiation, these qualities are reduced, making adjacent tissue transfer difficult at best.
The thickness of a local flap (or a construct involving a local flap) should match the thickness of the defect.
When raising local flaps, the subdermal plexus should be maintained.
Local flaps should not span anatomical boundaries. In cases where anatomical boundaries have been transgressed by the excision, reconstruction should be performed using two flaps, which meet at the boundary and help re-define it.
Deep sutures are often unnecessary, particularly on the nose where they frequently spit out. However, they should be used judiciously to close large dead spaces when they occur.
It is advisable to use a blue-colored suture in the skin such as 5-0 or 6-0 polypropylene: very few people have blue scabs or blood clots and the blue color makes them easier to remove. However, silk should be used around the eye to minimize irritation.
Generally, the debulking stage of a staged transfer should be performed before the stage where the pedicle is divided. In this way a more accurate and even debulking may be achieved.
Dog ears may be excised primarily by excising tissue away from the base of the flap.
On no account should a patient undergoing a local facial flap be allowed to smoke. All first and secondhand smoking should be discontinued 2 (preferably 4) weeks before surgery and for 2 weeks afterward.
If a local flap appears congested or ischemic on elevation, it should be returned to its bed as a “delay” and then re-elevated a couple of weeks later.
Although it is generally accepted that well-controlled anticoagulant therapy can be safely maintained during the perioperative period, aspirin taken purely for primary prevention of myocardial ischemia may be stopped 7 days preop without risk.
The provision of cover for scalp defects is commonly performed following the excision of skin malignancies such as basal cell carcinoma, squamous cell carcinoma, and malignant melanoma. Closure using skin grafts is feasible if pericranium is preserved, but closure by adjacent scalp tissue is preferred. When pericranium has been sacrificed, flap coverage is mandatory. Basically, there are three types of flap coverage in the scalp: rotation flaps, transposition flaps, and multiple rhomboid flaps.
When designing flaps in the scalp, it is useful to completely shave the head so that previous scars can be seen, and the planned flap sketched out on the remaining skin. That being said, the position of the anterior hairline should be marked to minimize the chance of causing a stairstep in the hairline or a visible scar on the forehead. It is important to identify the major sources of blood supply, namely the supratrochlear, the suprarbital, the superficial temporal, and the occipital arteries. At least one of these should be included in the base of the flap, with no intervening scar, in order to maintain viability. In the case of radiated scalps and in those patients who are smokers, the viability is always questionable, and more vessels should be included if possible.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here