Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Local anesthetic agents are important tools used in the everyday practice of emergency medicine. This chapter describes the mechanism of action, the nuances of clinical use, and the adverse reactions to anesthetics that are commonly used in the emergency department (ED). Detailed technical guidance for the performance of topical and infiltrative local anesthesia is provided.
The first local anesthetic was cocaine, an alkaloid in the leaves of the Erythroxylon coca shrub from the Andes Mountains. Early Incan society used cocaine for invasive procedures, including cranial trephination. In 1884, Koller used topical cocaine in the eye and was credited with the introduction of local anesthesia into clinical practice. In the same year, Zenfel used a topical solution of alcohol and cocaine to anesthetize the eardrum, and Hall introduced the drug into dentistry. In 1885 Halsted demonstrated that cocaine blocked nerve transmission, thereby laying the foundation for nerve block anesthesia. The search for alternatives to cocaine led to synthesis of the benzoic acid ester derivatives and the amide anesthetics used today. It was not until the 1960s that detailed understanding of the physiochemical properties, mechanism of action, pharmacokinetics, and toxicity of these agents emerged.
Most useful local anesthetic agents share a basic chemical structure:
Aromatic segment—Intermediate chain—Hydrophilic segment
Subtle variations in this basic structure determine each agent's main physiochemical properties: the negative log of dissociation constant (p K a ), the partition coefficient (a measurement of lipid solubility), and the degree of protein binding. Each of these properties determines the drug's potency, onset, and duration of action. However, physiochemical properties are not the sole determinant of clinical activity; other factors influence the drug's effect. The intermediate chain between the aromatic and the hydrophilic segments is either an amino-ester or an amino-amide; these chemical structures form the basis for the two main classifications of local anesthetics. Common ester-type agents include procaine, chloroprocaine, cocaine, and tetracaine. Common amide-type agents include articaine, lidocaine, mepivacaine, prilocaine, bupivacaine, and etidocaine. Different biochemical pathways metabolize each class. Esters are hydrolyzed by plasma pseudocholinesterase. Cocaine, an ester, is also partly metabolized by N-demethylation and nonenzymatic hydrolysis. Individuals with pseudocholinesterase deficiency may have a greater potential for cocaine toxicity if large doses are used, although this has not been an issue when cocaine is used clinically as an anesthetic. Amides are metabolized in the liver by enzymatic degradation. Local anesthetics are poorly soluble weak bases combined with hydrogen chloride to produce the salt of a weak acid. In solution, the salt exists both as uncharged molecules (nonionized) and as positively charged cations (ionized). The nonionized form is lipid soluble, which enables it to diffuse through tissues and across nerve membranes. The ratio of nonionized to ionized forms depends on the pH of the medium (vial solution or tissue milieu) and on the p K a of the specific agent. The p K a is the pH in which 50% of the solution is in the uncharged form and 50% is in the charged form. When the pH of the solution or tissue is less than the p K a , more of the drug is ionized. When the pH increases, more of the drug is in the nonionized form. Because the nonionized form of drug can diffuse through tissues and nerves, manipulating the pH of the solution can alter a drug's diffusion properties.
Local anesthetics are available in single-dose vials or ampules and in multidose vials, with and without epinephrine. Most solutions have a pH higher than 5. Multidose vials contain methylparaben (MPB), an antibacterial preservative. Local anesthetics premixed with epinephrine also contain an antioxidant (sodium bisulfite or sodium metabisulfite) to prevent deactivation of the vasoconstrictor. These solutions must be adjusted to a more acidic pH, approximately 3.5 to 4.0, to maintain the stability of epinephrine and its antioxidant. These properties as they relate to the amide group are depicted in Table 29.1 .
| SOLUTION CONTENT | pH (RANGE) | PRESERVATIVE (METHYLPARABEN) | ANTIOXIDANT |
|---|---|---|---|
| Plain, single dose | 4.5–6.5 | − | − |
| Plain, multidose | 4.5–6.5 | + | − |
| Commercial epinephrine, single dose | 3.5–4.0 | − | + |
| Commercial epinephrine, multidose | 3.5–4.0 | + | + |
| Prepared epinephrine, single dose | 4.5–6.5 | − | − |
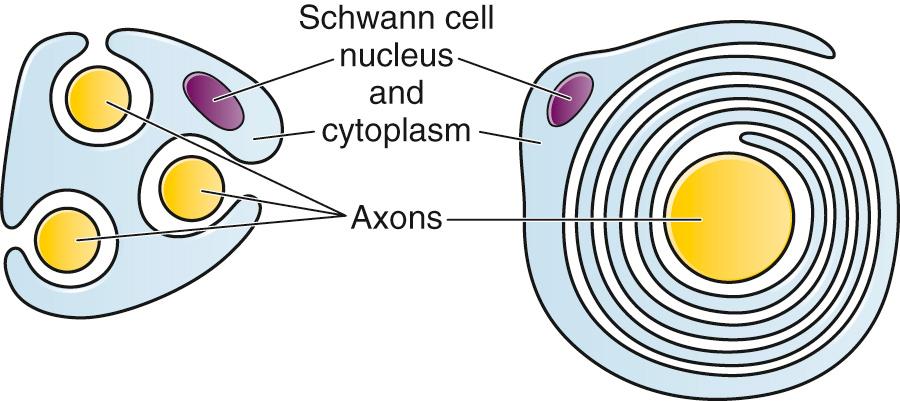
The functional nerve unit includes the nerve axon and its surrounding Schwann cell sheath. The Schwann cell ( Fig. 29.1 ) may surround several unmyelinated axons or a single myelinated nerve fiber and form a myelin sheath. Junctions between sheaths along the axon, called nodes of Ranvier, contain sodium channels necessary for depolarization. As myelin sheath thickness increases from autonomic to sensory to motor fibers, the nodes of Ranvier are spaced farther apart. The most important structure affecting transmission of nerve impulses is the axon membrane ( Fig. 29.2 ). The membrane consists of a double layer of phospholipids into which are embedded protein molecules that serve as channels containing pores for the movement of ions in and out of the cell. Most pores have a filter, or gate, that controls ion-specific movement and a sensory mechanism that opens or closes the gate. Bundles of nerve fibers ( Fig. 29.3 ) are embedded in the endoneurium, which is made of collagen fibrils, and they are surrounded by a cellular layer, the perineurium. The perineurium functions as a diffusion barrier and maintains the composition of extracellular fluid around the nerve fibers. Surrounding the entire structure is the outer layer of a peripheral nerve, the epineurium, which is composed of areolar connective tissue.


The inside of a nerve fiber, or axoplasm, is negative (−70 mV) at rest in comparison to the outside. This resting potential is the net result of the differences in ionic concentration on each side of the axonal membrane and the forces that tend to maintain that difference. Specifically, there is a surplus of sodium extracellularly and potassium intracellularly. The sodium channel is closed, thereby preventing these ions from moving along their concentration gradient (out → in). Although potassium can leave the cell to follow its concentration gradient (in → out), the need to maintain electrical neutrality inside the cell prevents it from completely doing so. Potassium is in equilibrium between the concentration gradient and the electrochemical gradient, thus creating the negative resting potential.
The sodium channel opens when a nerve is stimulated. Sodium ions enter slowly at first until a critical threshold is reached. They then enter the cell rapidly, along the electrochemical and concentration gradients, and cause depolarization. The influx of sodium is halted when the membrane potential reaches +20 mV, but potassium continues to move out of the cell and repolarizes it until the resting potential is reached. When the excitation process has been completed and the nerve cell is electrically quiet, the relative excess of sodium inside the cell and potassium outside the cell is readjusted by the adenosine triphosphate–dependent sodium-potassium pump.
Depolarization of a portion of the nerve causes a current to flow along the adjacent nerve fiber. This current makes the membrane potential less negative and actuates the sensor to open the next sodium channel. The action potential cycle is repeated, thereby propagating the impulse. Nerve conduction is essentially unidirectional because the sodium channel is not only closed but inactivated as well, and delayed closure of specific potassium channels prevents the critical threshold from being reached in the segment just depolarized. Impulses travel continuously down the axon in unmyelinated nerve fibers. In myelinated fibers, current flows from node to node and depolarizes intervening segments at once. This saltatory conduction causes a faster rate of impulse transmission in myelinated fibers.
How local anesthetic agents block nerve conduction depends on the active form of the agent and the specific physiologic and cellular activity.
Anesthetic solutions contain uncharged and charged forms. The concentration of the uncharged form increases in more alkaline milieus. Only this uncharged lipid-soluble form can cross tissue and membrane barriers. Once the uncharged drug is through a barrier, it reequilibrates into uncharged and charged forms in a proportion dependent on the prevailing pH. Because local anesthetics are more effective in alkaline solutions, it was originally thought that the uncharged form was responsible for conduction blockade. Alkaline solutions are currently believed to be more effective because of increased penetration through tissue barriers, but it is the cationic charged form that is responsible for the actual neuronal blockade.
Prevention of sodium influx across the nerve membrane forms the physiologic basis for conduction blockade. Local anesthetics slow sodium influx, thereby decreasing the rate of rise and amplitude of depolarization. If sufficient anesthetic is present and the firing threshold is not reached, the action potential is not formed. With no action potential, no impulse is transmitted and conduction is blocked, which results in local anesthesia.
How anesthetic agents prevent sodium influx is still not completely understood. It is believed that the cationic charged form blocks the action potential from inside the membrane; the agent enters the sodium channel from the axoplasmic side and binds to a receptor. This “specific receptor” theory is well accepted and is considered the predominant mechanism in preventing influx of sodium. However, this theory cannot account for the action of benzocaine and other neutral compounds or the uncharged base forms of the common local anesthetics.
In summary, when a local anesthetic (other than benzocaine) surrounds the perineurium, it equilibrates into its uncharged and charged forms based on tissue pH and p K a . In a more alkaline environment, a greater proportion of the uncharged form is present. The uncharged lipid-soluble form penetrates tissue, nerve sheath, and nerve membrane to gain access to the axoplasm and reequilibrates into both charged and uncharged forms. The charged form enters the sodium channel, decreases movement of sodium into the cell, and halts nerve transmission. The uncharged base is also involved in sodium channel blockade, but the exact nature of this mechanism is unknown.
A local anesthetic's onset, potency, duration, and ability to produce a differential blockade in mixed nerves are a function of its physiochemical properties, the physiologic environment, and to some extent, manipulation by the clinician.
The p K a of an anesthetic is the primary physiochemical factor that determines its onset of action. Increased tissue penetration and a shortened onset of action are found in drugs with a lower p K a because more of the lipid-soluble uncharged form is present ( Tables 29.2 and 29.3 ). Although in isolated nerve fibers the onset of action directly parallels p K a , other physiochemical factors also influence drug activity. For example, prilocaine and lidocaine have the same p K a , but lidocaine's onset is faster because of its enhanced ability to penetrate through nonnerve tissue.
| AGENT | ONSET: p K a | POTENCY: LIPID SOLUBILITY | DURATION: PROTEIN BINDING |
|---|---|---|---|
| Tetracaine | Slow | 8 | Long |
| Procaine | Slow | 1 | Short |
| Chloroprocaine | Fast | 1 | Short |
| Lidocaine | Fast | 2 | Moderate |
| Mepivacaine | Fast | 2 | Moderate |
| Prilocaine | Fast | 2 | Moderate |
| Bupivacaine | Moderate | 8 | Long |
| Etidocaine | Fast | 4–6 | Long |
| AGENT | TYPE | SITE OF METABOLISM | p K a | LIPID SOLUBILITY (PARTITION COEFFICIENT) | PROTEIN BINDING (%) |
|---|---|---|---|---|---|
| Tetracaine | Ester | Plasma | 8.5 | High (4.1) | 76 |
| Procaine | Ester | Plasma | 8.9 | Low (0.02) | 6 |
| Chloroprocaine | Ester | Plasma | 8.7 | Low (0.14) | — |
| Lidocaine | Amide | Liver | 7.9 | Medium (2.9) | 64 |
| Mepivacaine | Amide | Liver | 7.6 | Medium (0.8) | 78 |
| Prilocaine | Amide | Liver | 7.9 | Medium (0.9) | 55 |
| Bupivacaine | Amide | Liver | 8.1 | High (27.5) | 95 |
| Etidocaine | Amide | Liver | 7.7 | High (141.0) | 94 |
The site of administration also influences the onset of action. Onset times are prolonged as the amount of interspersed tissue or the size of the nerve sheath increases because of the greater distance that the agent must travel to reach its receptor. The pattern of onset for large nerves is determined by the structural arrangement of its fibers. Peripheral (mantle) fibers are blocked before core fibers. Because mantle fibers innervate more proximal regions, nerve blockade proceeds in a proximal to distal progression.
Adding sodium bicarbonate to raise the pH of the anesthetic solution (a technique that decreases pain on injection) yields a higher concentration of the uncharged lipid-soluble form and decreases onset time. Increasing the total dose by using a higher concentration of the same volume or a greater volume of the same concentration also shortens onset time. For most procedures performed in the ED, the time of onset of most agents is short enough that manipulation to achieve shorter times is unnecessary.
The lipid solubility of an anesthetic is a primary physicochemical factor determining potency. The drug's partition coefficient, not the concentration of the lipid-soluble form determined by the p K a or pH, confers its lipid solubility. Because the nerve membrane is lipid, lipophilic anesthetics pass more easily into the cell and few molecules are needed to block conduction (see Tables 29.2 and 29.3 ).
The degree of vasodilation produced by the anesthetic also affects potency because vasodilation promotes vascular absorption, thereby reducing the amount of locally available drug. Lidocaine is more lipid soluble than prilocaine or mepivacaine, but it produces more vasodilation. Although lidocaine is twice as potent as prilocaine or mepivacaine in vitro, it is equipotent in vivo. Though not a primary reason for its use, epinephrine increases the depth of anesthesia by producing vasoconstriction and making more molecules available to the nerve. Drugs more readily absorbed by fat have reduced potency. Increased concentration also increases potency. Choosing an anesthetic for its potency is not usually necessary for any given site because the commercially available concentration of an agent may be manipulated to make most drugs equianesthetic. For example, lidocaine, being one fourth as potent as bupivacaine, is usually used at four times the concentration (1% to 2% vs. 0.25% to 0.5%, respectively). For different sites and techniques, different concentrations and volumes of a given agent are needed to produce adequate blockade.
The degree of protein binding of an anesthetic primarily determines its duration of action. Agents that bind more tightly to the protein receptor remain in the sodium channel longer (see Tables 29.2 and 29.3 ). Like potency, the duration of action is reduced by the vasodilation produced by local anesthetics. Prilocaine, which is less protein bound than lidocaine, has a longer duration of action because of its lesser degree of vasodilation. The duration of action also varies with the mode of administration. It is shorter when agents are applied topically.
The duration of action may be prolonged by several methods. Increasing the dose, usually by increasing the concentration, prolongs the duration to limits imposed by toxic effects. Raising the pH of the anesthetic solution has also been shown to prolong duration. The most practical way to increase duration is to use solutions that contain epinephrine. Epinephrine causes vasoconstriction, decreases systemic absorption, and allows more drug to reach the nerve. The effect of epinephrine varies according to the agent. Anesthetics that intrinsically produce more vasodilation (e.g., procaine, lidocaine, mepivacaine) benefit more from epinephrine's vasoconstrictive action. The long-acting, highly lipid-soluble agents (e.g., bupivacaine, etidocaine) are less affected because they are substantially taken up by extradural fat and released slowly. In fact, lidocaine with epinephrine may be effective for as long as bupivacaine without epinephrine. Generally, most ED procedures can be accomplished quickly before the anesthesia wears off regardless of which drug is selected. Choose agents with a long duration of action when the procedure is lengthy or if postoperative analgesia is desired.
Local anesthetic agents may be applied topically to mucous membranes, intact skin, and lacerations. There are sufficient differences among these sites to merit a separate discussion of each one. Topical anesthesia of the eye is discussed in Chapter 62 .
Effective anesthesia of the intact mucous membranes (not intact skin) of the nose, mouth, throat, tracheobronchial tree, esophagus, and genitourinary tract may be provided by several anesthetics ( Box 29.1 ). Tetracaine, lidocaine, and cocaine are the most effective commonly used agents ( Table 29.4 and Box 29.1 ). Benzocaine (14% to 20%) is commonly used for intraoral or pharyngeal anesthesia ( Fig. 29.4 ). The anesthesia produced is superficial and does not relieve pain that originates from submucosal structures. The onset of action may be slow, which limits its usefulness in urgent situations (such as passing a nasogastric tube). Agents applied topically can be absorbed systemically, and concentrated topical agents can cause toxicity.
Benzocaine spray will produce transient anesthesia of the mucous membranes. Rarely, it can precipitate methemoglobinemia in standard doses. Anbesol (Pfizer Inc., New York, NY) is a popular over-the-counter benzocaine anesthetic for dental problems, such as teething. Topical anesthesia of mucous membranes can be obtained by applying a gel mixture of 10% lidocaine, 10% prilocaine and 4% tetracaine (Profound, Steven’s Pharmacy Costa Mesa, CA, www.stevensrx.com ) and is preferred by editors.
EMLA cream (lidocaine and prilocaine) will produce anesthesia of intact skin, but it must be in place for approximately 60 minutes to provide significant benefit.
ELA-Max, now known as LMX4 (Ferndale Laboratories Inc, Ferndale, MI), is another topical lidocaine preparation with a more rapid onset of action.
“Magic mouthwash” contains equal parts of diphenhydramine elixir, Maalox (Novartis, East Hanover, NJ), and 2% viscous lidocaine. Each 5-mL teaspoon contains less than 50 mg of lidocaine. It is swished, held in the mouth for 1 to 2 minutes, and expectorated.
Lidocaine (2%) may be used intraorally, but repeated use may produce systemic toxicity, especially in children. Each 5-mL teaspoon contains 100 mg of lidocaine. It should not be swallowed but, instead, expectorated after holding it in the mouth for a few minutes. Viscous lidocaine is not useful for acute pharyngitis. Systemic narcotics are preferred if the pain is severe.
ED, Emergency department; EMLA, eutectic mixture of local anesthetics.
| AGENT | USUAL CONCENTRATION (%) | Maximum Dosage a | ONSET (min) | DURATION (min) | |
|---|---|---|---|---|---|
| Adult (mg) | Pediatric (mg/kg) | ||||
| Tetracaine | 0.5 | 50 | 0.75 | 3–8 | 30–60 |
| Lidocaine | 2–10 | 250–300 b | 3–4 b | 2–5 | 15–45 |
| Cocaine c | 4 | 200 | 2–3 b | 2–5 | 30–45 |
a These are conservative figures; see text for explanations.
b The lower dosage should be used for a maximum safe dose when feasible.
c The 10% cocaine solution is best avoided because of minimal additional clinical benefit and the potential for coronary vasoconstriction in patients with coronary artery disease.

Tetracaine solution is an effective and potent topical agent with a relatively long duration of action. It is used in concentrations from 0.25% to 1% with a recommended maximum adult dose of 50 mg. In overdose, it has the disadvantage of severe cardiovascular toxicity without any preceding central nervous system (CNS) stimulatory phase.
Lidocaine is also an effective topical agent that is marketed in a variety of forms (solutions, jellies, and ointments) and concentrations (2% to 10%). The 10% form is most effective, and minimal topical anesthesia is achieved with less potent concentrations. Lidocaine is commonly used as the 2% viscous solution prescribed for inflamed or irritated mucous membranes of the mouth and pharynx. Patient misuse of viscous lidocaine, by repeated self-administration, can lead to serious toxicity. Topical lidocaine provides an adequate duration for most procedures, with the maximum safe dose being 250 to 300 mg.
Cocaine is an effective, but potentially toxic topical agent that is applied to the mucous membranes of the upper respiratory tract. Although it is an ester, hepatic metabolism occurs, as does hydrolysis by plasma pseudocholinesterase. Absorption is enhanced in the presence of inflammation. Cocaine is the only anesthetic that produces vasoconstriction at clinically useful concentrations, hence its popularity for treating epistaxis. This major advantage is offset by its susceptibility to abuse and toxic potential. The toxic effects are due to direct stimulation of the CNS and blockade of norepinephrine reuptake in the peripheral nervous system. Cocaine should not be administered to patients who are sensitive to exogenous catecholamines or who are taking monoamine oxidase (MAO) inhibitor antidepressants. Clinical manifestations of toxicity include CNS excitement, seizures, and hyperthermia. Central and peripheral effects of hypertension, tachycardia, and ventricular arrhythmias may also be seen. Acute myocardial infarction has been reported after topical application. Cocaine is commonly used as a 4% solution with a maximum safe dose of 200 mg (2 to 3 mg/kg). A 10% solution is available, but this concentration adds little to the topical effect while enhancing the potential for toxicity. Coronary vasoconstriction may occur with doses as low as 2 mg/kg applied to the nasal mucosa. Although the clinical effect of this vasoconstriction is usually benign and without electrocardiographic changes, topical cocaine should be used cautiously in patients with known or suspected coronary artery disease. Dyclonine offers advantages over other topical anesthetic agents. It is a ketone derivative without an ester or amide linkage and may be used in patients who are allergic to the common anesthetics. Extensive experience with the topical preparation has shown it to be effective and safe. Dyclonine is marketed in 0.5% and 1% solutions, often in sore throat preparations, with a maximum adult recommended dose of 300 mg.
Benzocaine is an ester that is marketed in its neutral form in 14% to 20% preparations (Cetacaine [Cetylite Industries, Inc., Pennsauken, NJ], Americaine [Celltech Pharmaceuticals, Rochester NY], Hurricaine) (see Fig. 29.4 ). Its low water solubility prevents significant penetration of the mucous membranes, thus reducing systemic toxicity if applied to intact mucosa. However, it is not a potent anesthetic and has a brief duration of action. It is more allergenic than other topical agents. Benzocaine is usually dispensed in an admixture with other therapeutic ingredients and is clinically effective only at relatively high (>14%) concentrations. Benzocaine is available as a nonprescription gel and liquid (6.3% to 20% Anbesol [Pfizer Inc., New York, NY], for example) and is used for a variety of maladies, including ear pain, mouth pain, and teething. It is commonly used by dentists to produce mucosal anesthesia before intraoral nerve blocks (see Chapter 30 ). Adriani and Zepernick recommended this agent for lubricating catheters, airways, endotracheal tubes, and laryngoscopes and reported only one adverse reaction (methemoglobinemia) in their experience with approximately 150,000 patients. Methemoglobinemia occurs rarely after mucosal absorption of benzocaine used repeatedly for teething infants and after standard doses of benzocaine sprays used in endoscopic procedures.
An excellent topical preparation is a combination of lidocaine, prilocaine, and tetracaine, especially useful for dental mucosa anesthesia. Topical gel mixtures of 2.5% lidocaine and 2.5% prilocaine (eutectic mixture of local anesthetics [EMLA]) are commonly used on intact skin but have also been used on mucous membranes. EMLA is more effective than 20% benzocaine when applied to the oral mucosa before needle injection for dental anesthesia. One study demonstrated that pain was reduced more quickly with EMLA than with benzocaine when applied to the buccal mucosa.
As with infiltrated anesthesia, toxic reactions to topically applied anesthetics correlate with the peak blood levels achieved and not necessarily with the dose administered. Systemic absorption of a topical agent is more rapid, with a higher level being achieved than with the same dose given by infiltration. The total dose of a topical anesthetic should be considerably less than that used for infiltration at a given site. Fractionating the total dose into three portions administered over a period of several minutes effectively reduces peak blood levels. Inadvertent suppression of the gag reflex, combined with difficulty swallowing, may lead to aspiration, an important potential adverse reaction to topical anesthesia of the nose, mouth, and pharynx. Infections from drug solutions in multidose vials for topical anesthesia of the larynx and trachea have not been substantiated.
A commonly used “magic mouthwash” for the topical treatment of painful gingivostomatitis in children is often prescribed by emergency clinicians and pediatricians. There has been little scientific study of the preparation and it is not available commercially, but it has been used safely for decades. It consists of equal parts viscous lidocaine (2%), Maalox as a binder, and diphenhydramine elixir. Corticosteroids or nystatin is often added when the mixture is used to treat chemotherapy-induced mucositis. However, a 2004 review found no evidence that magic mouthwash is effective in treating this condition. The creamy mixture is swished around the mouth and expectorated, or painted on specific lesions with a cotton swab. Packing an area with a cotton ball soaked with this mixture is another option. Repeated doses or swallowing of the elixir can produce systemic toxicity, so careful instruction should be given to limit use of the solution to every few hours. This combination would be theoretically less toxic than simply using topical lidocaine.
Emergency clinicians often prescribe 2% viscous lidocaine (20 mg/mL) for patients with pharyngitis, stomatitis, dental pain, or other inflammatory or irritative lesions in the oropharynx. Although this intervention is widely used and generally safe, the common misconception that topical anesthesia is totally innocuous may result in poor patient instructions and serious consequences. Topical lidocaine is helpful for painful mouth lesions, but is of little practical value for acute pharyngitis, for which systemic analgesics are usually a better option. Seizures and death from topical lidocaine have been reported when excessive repeated doses have been administered. Toxic blood levels may occur because the anesthetic effect of viscous lidocaine lasts for only 30 to 60 minutes and patients with recurrent pain may either ignore or be ignorant of the safe dosing interval of 3 hours and medicate themselves more frequently. Patients tend to increase each dose to obtain greater relief, and inflammation may increase systemic absorption. In addition, painful oral lesions may last for several days.
Children are at higher risk for the rare toxicity of oral lidocaine. When compared with adults, children may exhibit increased lidocaine absorption, decreased clearance, and a longer half-life. Continued medication use allows lidocaine and its major metabolites monoethylglycinexylidide (MEGX) and glycinexylidide (GX) to accumulate. Both MEGX and GX are produced from the hepatic metabolism of lidocaine and are excreted in urine. They possess anesthetic and antiarrhythmic activity and have the potential for CNS toxicity. Although these metabolites are less potent than lidocaine, their elimination half-lives are considerably longer. Several investigators regard MEGX and GX to be the cause of CNS toxicity with prolonged topical use of lidocaine. The length of time that viscous lidocaine is retained in the mouth and whether the excess is expectorated or swallowed also affect the blood level produced. Expectorating the medication after swishing it in the mouth produces much lower blood levels than when it is swallowed. It seems logical that the most hazardous mode of administration would be to retain the solution in the mouth “until absorbed.”
Clearly explain the proper way to use viscous lidocaine and inform patients not to dose themselves ad libitum . Note that a 2% solution contains 20 mg/mL, or 100 mg per standard teaspoon (5 mL). The recommended maximum adult dose is 300 mg (15 mL of a 2% solution) no more frequently than every 3 hours. When possible, instruct the patient to decrease the dose by using direct cotton swab application. When gargled or swished in the mouth, limit application time to 1 to 2 minutes, and instruct the patient to expectorate excess solution. Limit use to 2 or 3 days, especially if swallowing the solution is necessary to obtain relief. Prescribe lower doses for patients at risk for decreased clearance (see later section on Systemic Toxic Reactions ). Doses for children are prescribed at 3 mg/kg. Because infants cannot expectorate well, do not use viscous lidocaine for minor oral irritation and teething. Recommend that no food be eaten for 1 hour after application because anesthesia of the oropharynx can interfere with swallowing and cause aspiration. Special note should be made of the over-the-counter availability of benzocaine, commonly used for toothaches and teething. A gel or liquid (Anbesol, Pfizer) is available in 6.3% to 20% formulations. When used repeatedly in the oral cavity on irritated tissue, systemic toxicity, including methemoglobinemia, may occur.
Lidocaine 4% solution can be atomized with a standard nebulizer device commonly used for delivering asthma medications and inhaled by the patient before insertion of a nasogastric tube. This method effectively anesthetizes the nasopharyngeal and oropharyngeal tissues, thereby easing the pain of tube insertion. Lidocaine (4%) and cocaine (4%) atomized by a single-use mucosal atomizer, compared with lidocaine gel (4%), demonstrated equal reductions in nasal pain scores during the insertion of a nasogastric tube in healthy study participants, although they indicated that overall discomfort was less with lidocaine gel injected into the nose.
The stratum corneum provides a cutaneous barrier that prevents the commonly marketed aqueous solutions (acid salts) from producing anesthesia, but saturated solutions of the bases of local anesthetics are effective on intact skin. When applied topically to abraded skin, most anesthetic agents produce peak blood levels similar to those resulting from infiltration in 6 to 10 minutes.
In 1974, Lubens and coworkers used 30% lidocaine cream, saturated on a gauze pad and adherent to an elastic patch, for a myriad of procedures including minor operative procedures (e.g., excision of lesions, incision and drainage of abscesses), lumbar puncture, venipuncture, and allergy testing. Today, lidocaine is available in a 5% patch, and remains one of the most commonly used topical compounds. Recent literature regarding its effectiveness, however, has been mixed. In a study by Cheng, a lidocaine patch applied at the site of rib fractures in patients taking oral pain medication decreased pain scores when compared to a placebo patch. In contrast, a meta-analysis of 251 patients in 5 trials compared lidocaine patches to placebo patches for acute or postoperative pain, but failed to conclusively demonstrate that a lidocaine patch decreases pain intensity, reduces opioid consumption, or reduces hospital length of stay.
Various topical anesthetics have been suggested to decrease the pain of venipuncture or injections and to provide topical anesthesia for painful skin abrasions and lesions. These agents have been studied extensively and are safe, but they are not practical in many ED settings because of their slow onset of action and inadequate efficacy. However, their activity profiles make them more applicable than 30% lidocaine cream to emergency medicine. Tetracaine base is available as a solution, a gel, and a patch preparation. It is effective in crossing the lipid-rich barrier of the stratum corneum because it is highly lipophilic. EMLA was approved in the United States in 1992. It contains 2.5% lidocaine and 2.5% prilocaine in a unique oil-and-water emulsion, yielding 5% EMLA. The mild lipophilic and hydrophilic properties of the component drugs are greatly increased when mixed together, thereby allowing absorption through intact skin. ELA-Max and ELA-Max5, now known as LMX 4 and LMX 5 respectively (Ferndale Laboratories Inc, Ferndale, MI), are topical lidocaine anesthetic creams with a more rapid onset of action than EMLA cream. ELA-Max is a 4% concentration, and 5% ELA-Max is marketed as an anorectal cream that may benefit patients undergoing painful rectal procedures. Neither product has prilocaine, as is found in EMLA cream, and neither has US Food and Drug Administration approval for pain relief before painful injections or intravenous (IV) insertion, but both have such potential.
Tetracaine base seems to offer the advantage of being able to achieve effective anesthesia with a shorter application time and a longer duration. For tetracaine and EMLA preparations, onset, depth of anesthesia, duration, and blood levels vary directly with application time, use on thinner or inflamed skin, and larger doses. These preparations exhibit a reservoir effect. The drug is deposited in the stratum corneum and continues to diffuse along its concentration gradient, even after it is removed from the skin.
Tetracaine base, lidocaine cream, and EMLA can be useful in the ED for providing anesthesia for many procedures: venous cannulation, venipuncture, or any needle insertion, including preinfiltration anesthesia and lumbar puncture; a variety of minor surgical procedures; and anesthetizing the tympanic membrane and external auditory canal. EMLA has also been used effectively for débridement of ulcers. EMLA cream applied to wound edges prior to local wound infiltration with 1% lidocaine decreased the pain of laceration repair compared with infiltrative anesthesia alone.
EMLA and 5% lidocaine cream are equally effective in reducing the pain of IV insertion. Luhmann and colleagues demonstrated that 5% lidocaine cream applied for 30 minutes under an occlusive dressing was as effective as infiltrated buffered lidocaine before IV catheter insertion in children. Obviously, infiltrative administration of buffered lidocaine requires skin puncture, but its onset of anesthesia is almost immediate. When time is not an issue, topical creams may be an acceptable alternative to infiltrated anesthesia or no anesthesia at all. Approximately a 60-minute interval after application is required for these preparations to provide optimal topical analgesia to the intact skin for such procedures as venipuncture. Early cutaneous placement of these agents (e.g., over common IV sites while the patient is being triaged) is important for practical ED use.
These topical agents are often used for limited skin incisions (e.g., drainage of small abscesses), trigger point injections, joint aspiration, or injection of bursitis or tendinitis. These agents evaporate quickly from the skin and cool it to the point of freezing. Anesthesia is effective and immediate, but drawbacks include its short duration (only up to 1 minute), potential pain on thawing, and possibly lowered resistance to infection and delayed healing. Highly volatile ethyl chloride spray is flammable. Ethyl chloride has been studied in children to reduce the pain of venipuncture, but the results are mixed. Given their short duration of action and the time needed to perform pediatric venipuncture, these preparations have limited use for this purpose.
This 30% cream is saturated on a gauze pad that is adherent to an elastic patch and placed over the area to be injected or incised. The high concentration of anesthetic and an occlusive patch are needed to achieve effective skin penetration. The duration of action varies with the application time. A 45-minute application time is needed for most procedures. To achieve a topical anesthetic duration of 30 minutes, a 2-hour application is necessary.
Because both agents demonstrate a reservoir effect, anesthesia may increase or begin many minutes after removal of the drug. A precise description of application times and duration is not possible. Tetracaine base requires a minimum of 20 to 30 minutes of application time to produce several hours of anesthesia. EMLA requires an application time of 1 to 2 hours for a reported duration of 30 minutes to several hours. Occlusive dressings seem to increase penetration of EMLA whenever the cream is used. Patches are more convenient and cause no loss of effectiveness.
EMLA dosing is based on the amount of cream applied, not on the amount of anesthetic. Each gram of EMLA cream contains 25 mg of lidocaine and 25 mg of prilocaine. Dosages are given in grams of cream, not milligrams of anesthetic. In general, apply EMLA as a thick layer over intact skin under an occlusive dressing for approximately 1 hour before a procedure. Application of a thick layer approximates to 1 to 2 g/10 cm 2 . For minor procedures such as needle insertions, apply 2.5 g of EMLA over 20 to 25 cm 2 for at least 1 hour. For more painful procedures, apply approximately 2 g of cream per 10 cm 2 for at least 2 hours. The maximum application area (MAA) determines the appropriate total dose applied. Base the MAA on the patient's weight as follows: up to 10 kg, MAA = 100 cm 2 ; 10 to 20 kg, MAA = 600 cm 2 ; more than 20 kg, MAA = 2000 cm 2 .
Collect all the equipment required and make all preparations needed to immediately perform the desired procedure. Invert the bottle 25 cm from the skin and spray a stream along the proposed incision site until the area turns white and hard. Make the incision or local anesthetic injection immediately or during actual spraying of the agent for optimal results because the effect is fleeting. Some clinicians use these vapocoolant sprays to decrease the pain of injection of a more traditional local anesthetic such as lidocaine.
Anesthetic agents may be drawn into the skin without needles by electrical current applied through electrodes in a process called iontophoresis . Lidocaine with epinephrine administered via iontophoresis provides adequate anesthesia before venipuncture in pediatric patients and is superior to EMLA in providing cutaneous anesthesia. Iontophoresis is not widely used in emergency medicine but may be another alternative to applied anesthetic agents.
Recently developed technology known as microneedle pretreatment may improve the efficacy of cutaneously applied topical anesthetics. A functional microarray of fine needles painlessly perforates the stratum corneum to facilitate the penetration of applied medications without using traditional needle injections. A 2010 study demonstrated that perforation of the skin of healthy volunteers with a microneedle to which dyclonine was applied resulted in decreased time to anesthesia and a greater degree of pain reduction than did application of dyclonine to nonperforated skin. Microneedling followed by the application of EMLA prior to facial laser resurfacing, and lidocaine 2.5%/prilocaine 2.5% prior to full face fractional microneedling for atrophic acne scars was superior than either topical anesthetic applied alone. This emerging technology may improve the practical application of anesthetics to intact skin in the ED.
Jet injection of anesthetic through intact skin may overcome some of the limitations imposed by the cutaneous application of anesthetics without needle infiltration. A jet injector is a device containing carbon dioxide gas that rapidly forces a plunger to expel the drug through a small orifice applied over intact skin. Medication penetrates the epidermis to a depth of 5 to 8 mm in 0.2 second and causes the drug to be rapidly dispersed through the skin. Safety is improved because no needles are used to penetrate the skin. Several studies have demonstrated that jet injection of anesthetics provides more rapid anesthesia than topical application of anesthetic agents and is preferred by patients over no anesthesia at all for painful procedures such as laceration repair, lumbar puncture, IV insertion, and arterial blood gas sampling.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here