Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The liver, like the pancreas, develops embryologically as a glandular outgrowth of the primitive foregut . The major functions of the liver may be summarised as follows:
Oxidising triglycerides to produce energy
Synthesis of plasma lipoproteins
Synthesis of cholesterol and phospholipid
Converting carbohydrates and proteins into fatty acids and triglyceride
Regulation of blood glucose concentration by glycogenesis, glycogenolysis and gluconeogenesis
Synthesis of plasma proteins, including albumin and clotting factors
Synthesis of non-essential amino acids
Detoxification of metabolic waste products (e.g. deamination of amino acids and production of urea)
Storage of glycogen, vitamins, iron
Detoxification of various drugs and toxins (e.g. alcohol)
Synthesis and secretion of bile, which contains many of the products of the above processes
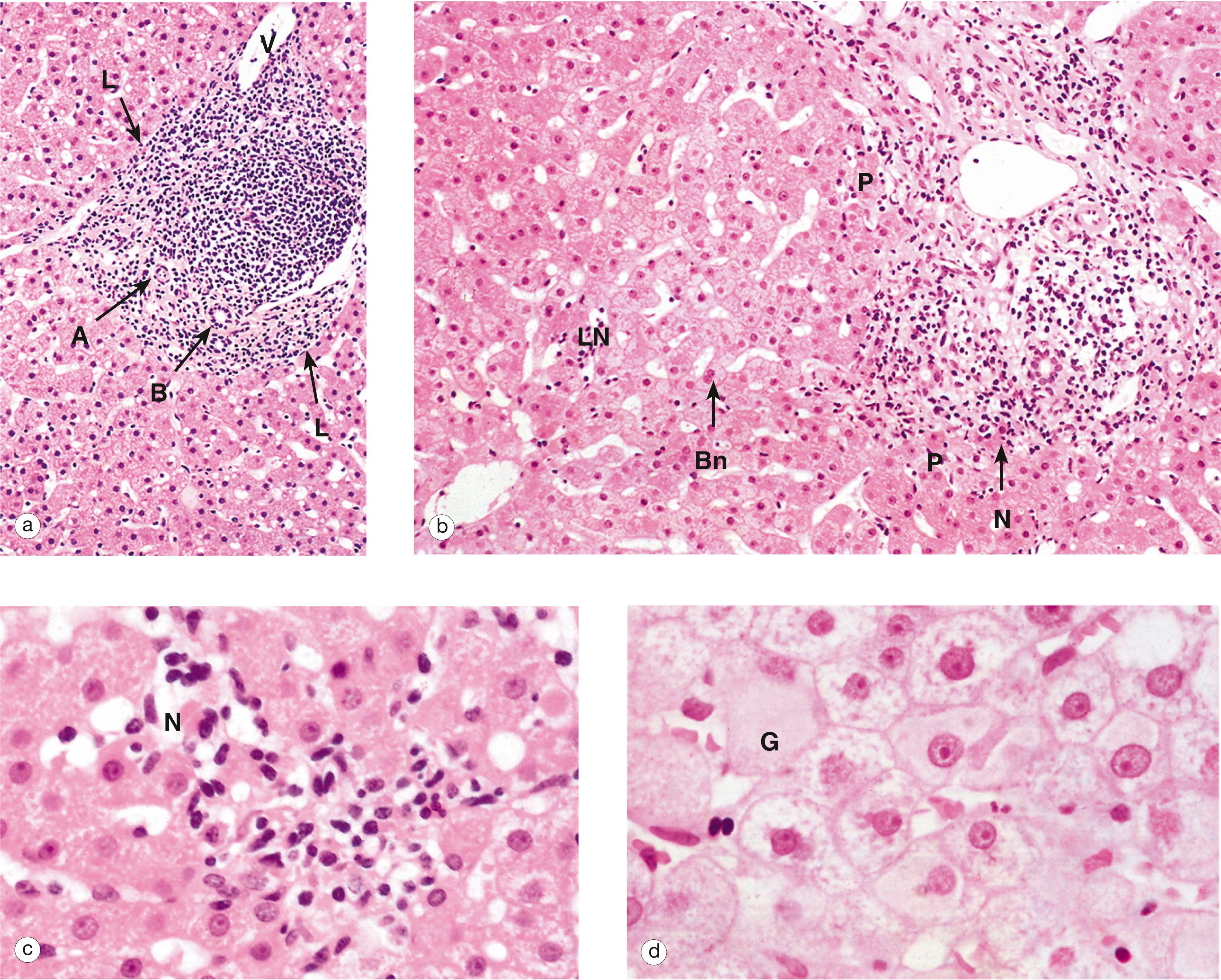
The main functional cell in the liver is a type of epithelial cell called the hepatocyte . These cells are arranged as thin plates separated by fine vascular sinusoids through which blood flows. The close association of liver cells and the circulation allows absorption of nutrients from digestion, as well as secretion of products into the blood.
Blood flow into the liver sinusoids comes from terminal branches of both the hepatic portal vein and hepatic artery . The liver is therefore unusual in having both arterial and venous blood supplies, as well as separate venous drainage.
With the exception of most lipids, absorbed food products pass directly from the gut to the liver via the hepatic portal vein. This brings blood that is rich in amino acids, simple sugars and other products of digestion but relatively poor in oxygen. The oxygen required to support liver metabolism is supplied via the hepatic artery. After passing through the sinusoids, venous drainage of blood from the liver occurs via the hepatic vein into the vena cava.
The main blood vessels and ducts run through the liver within a branched collagenous framework termed the portal tracts . These tracts also contain the bile ducts that transport bile away from the liver to be secreted into the small bowel.
B bile duct C liver capsule M mesothelial cells P portal tract V hepatic venule
Liver disease is a common problem worldwide and its causes are diverse. Some forms of liver disease are readily diagnosed using a combination of clinical features and blood tests. Such investigations may include standard liver function tests, studies to assess for autoimmune disease, serological testing for viral hepatitis, etc.
Direct examination of tissue biopsies from the liver may be necessary in some cases for a range of reasons, such as to determine the underlying diagnosis, assess disease severity or seek evidence of disease progression.
Special staining methods such as the reticulin preparations shown here are very useful in the pathological assessment of liver biopsies, serving to highlight different aspects of the liver structure. Further details on special stains can be found in Appendix 2 .
A hepatic artery branch B bile ductule BC binucleate cell H hepatocyte plate L lymphatic PV terminal portal venule S sinusoid SC sinusoid lining cell T portal tract V terminal hepatic venule
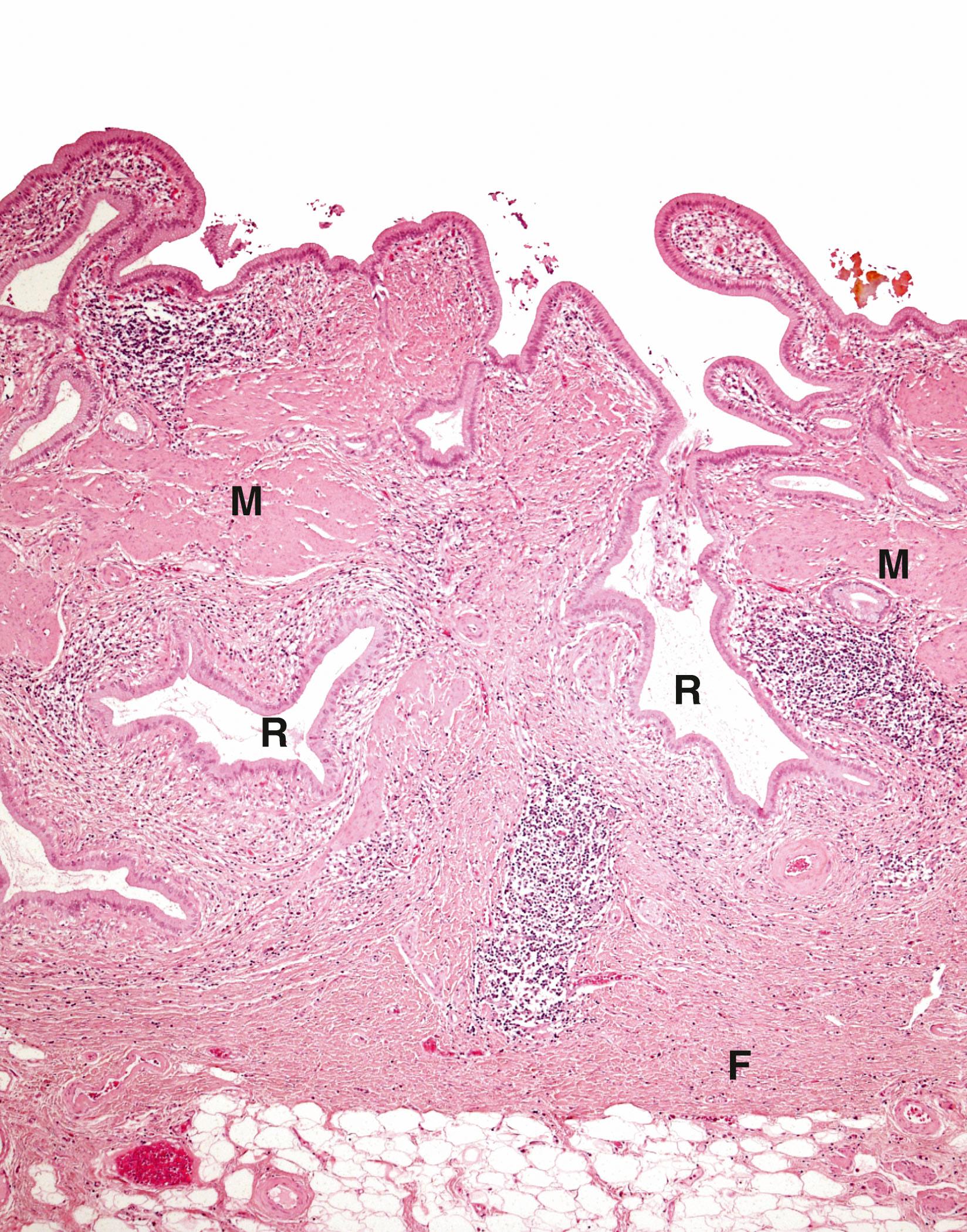
F fibrous septum T portal tract V terminal hepatic venule
In diseases where there is repeated liver cell destruction, the liver responds by cell division to replace dead liver cells ( regeneration ) and by depositing collagenous tissue ( scarring ). The combination of nodules of regenerated liver cells separated by bands of scar tissue is termed cirrhosis .
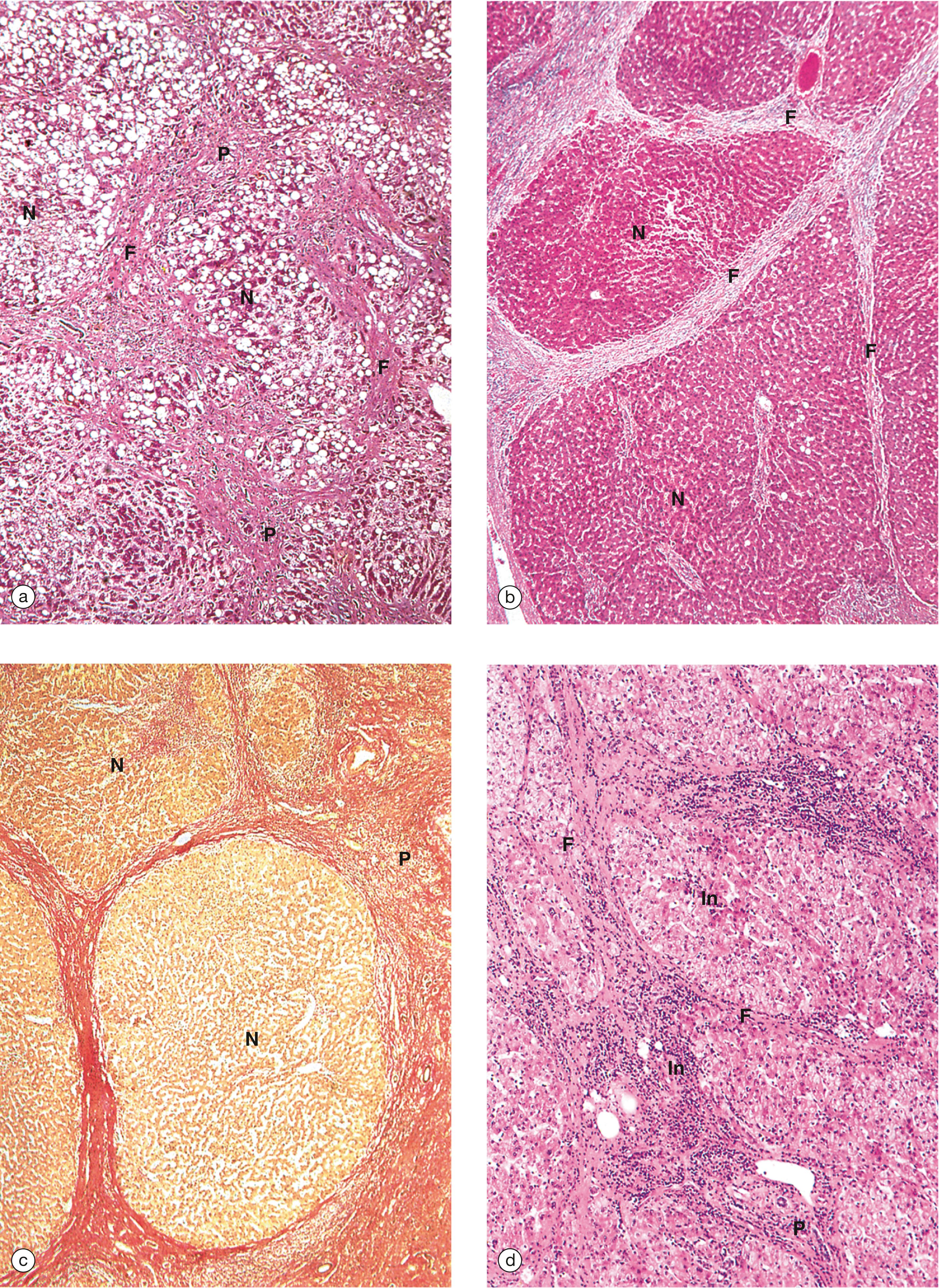
In cirrhosis, the liver cells that are separated from a normal sinusoidal blood flow have reduced function (e.g. reduced synthesis of albumin and reduced secretion of bile). The scarring and interruption of the low-resistance sinusoidal system has important consequences. Blood from the portal vein cannot drain from the liver and portal hypertension develops.
The common causes of cirrhosis are diseases in which there is continued liver cell damage and death. Chronic ethanol abuse is an important cause. Infection with hepatitis viruses B and C often leads to chronic hepatitis and a risk of cirrhosis. Certain autoimmune diseases are also recognised to cause chronic hepatitis and cirrhosis in susceptible patients. Rare causes include excessive storage of iron and copper due to genetic metabolic diseases.
B binucleate hepatocyte C collagenous tissue Ca bile canaliculus E endothelial cell EP erythroid precursors K Küpffer cell M megakaryocyte MP myeloid precursor T portal tract V terminal hepatic venule
Jaundice is a yellow discolouration of the tissues due to increased levels of bilirubin and associated deposition of bile pigments. It is a common consequence of liver and biliary tract disease but its causes are very diverse. Hyperbilirubinaemia (raised blood level of bilirubin) can be classified as prehepatic, hepatic or posthepatic .
Prehepatic jaundice occurs due to increased production of bilirubin, exceeding the liver’s capacity to excrete it in its water-soluble conjugated form. The majority of bilirubin comes from metabolism of haemoglobin and so this form of jaundice is usually associated with conditions in which there is excessive red cell breakdown, such as sickle cell anaemia and other haemoglobinopathies. In this type of jaundice, there is predominantly unconjugated hyperbilirubinaemia .
Hepatic jaundice occurs when there is acute or chronic damage to the liver, reducing its ability to metabolise and excrete bilirubin. In this condition, there is usually a mixture of conjugated and unconjugated hyperbilirubinaemia.
Posthepatic jaundice is also known as obstructive jaundice and reflects some form of mechanical blockage which interrupts the flow of bile into the biliary system. Most commonly, this occurs due to gallstones (see Fig. 15.13 ) blocking the common bile duct or due to tumour arising in the head of the pancreas (see Fig. 15.16 ). In obstructive jaundice, there is predominantly conjugated hyperbilirubinaemia, since there is no intrinsic metabolic problem but, rather, a simple mechanical blockage. Sometimes this type of jaundice is referred to as surgical jaundice because its treatment often requires surgical input.

BC bile canaliculus D space of Disse E erythocytes H hepatocyte J junctional complex L lipid droplet Ly lysosome M mitochondrion Mv microvilli rER rough endoplasmic reticulum S sinusoid lining cells sER smooth endoplasmic reticulum
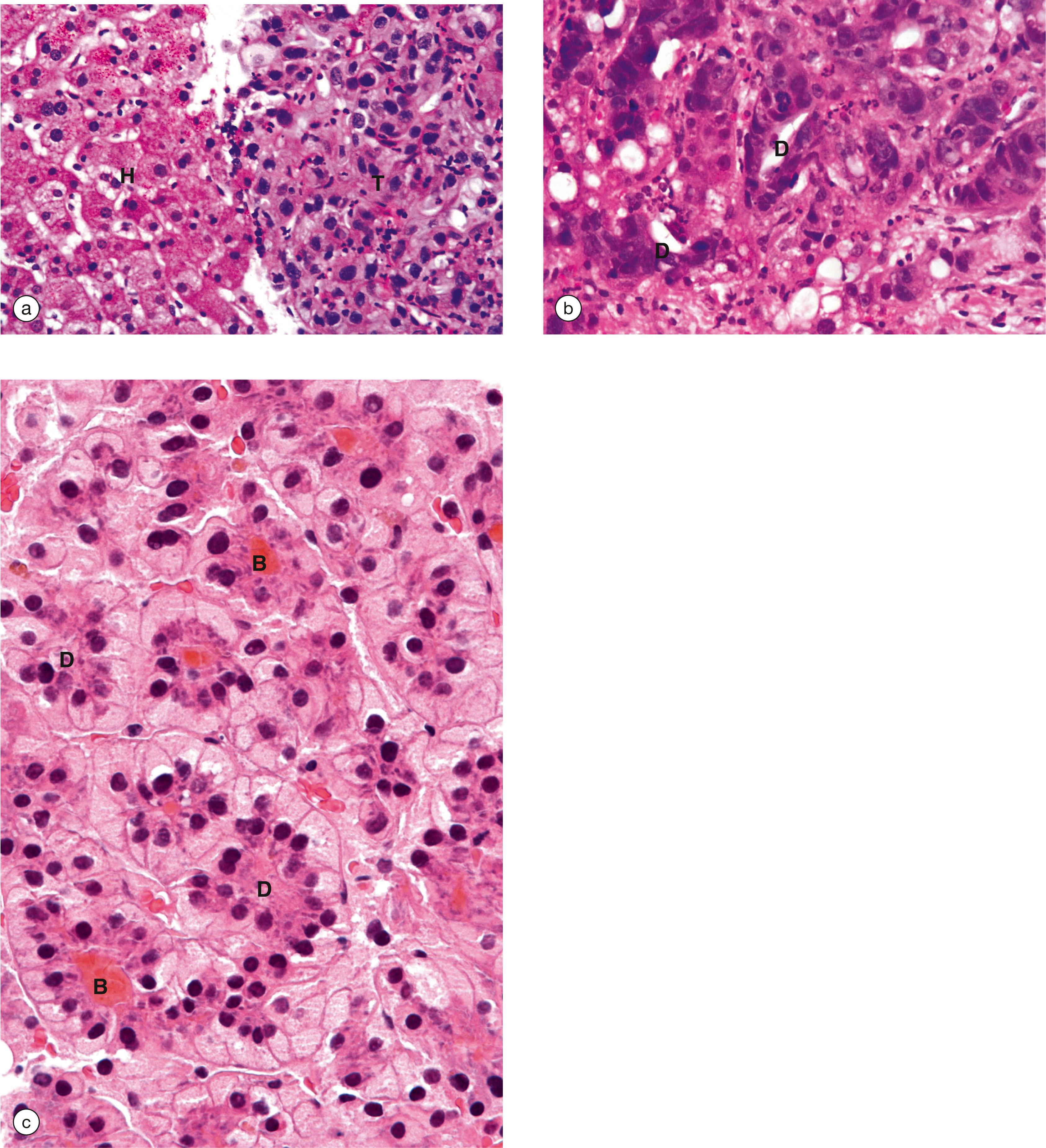
Any cause of cirrhosis of the liver predisposes to HCC which is a primary liver carcinoma . Tumours can present as one large tumour nodule or multiple nodules. Histologically, the tumour cells resemble hepatocytes unless very poorly differentiated. Alpha-fetoprotein is often secreted by these tumours and therefore can be used as a tumour marker.
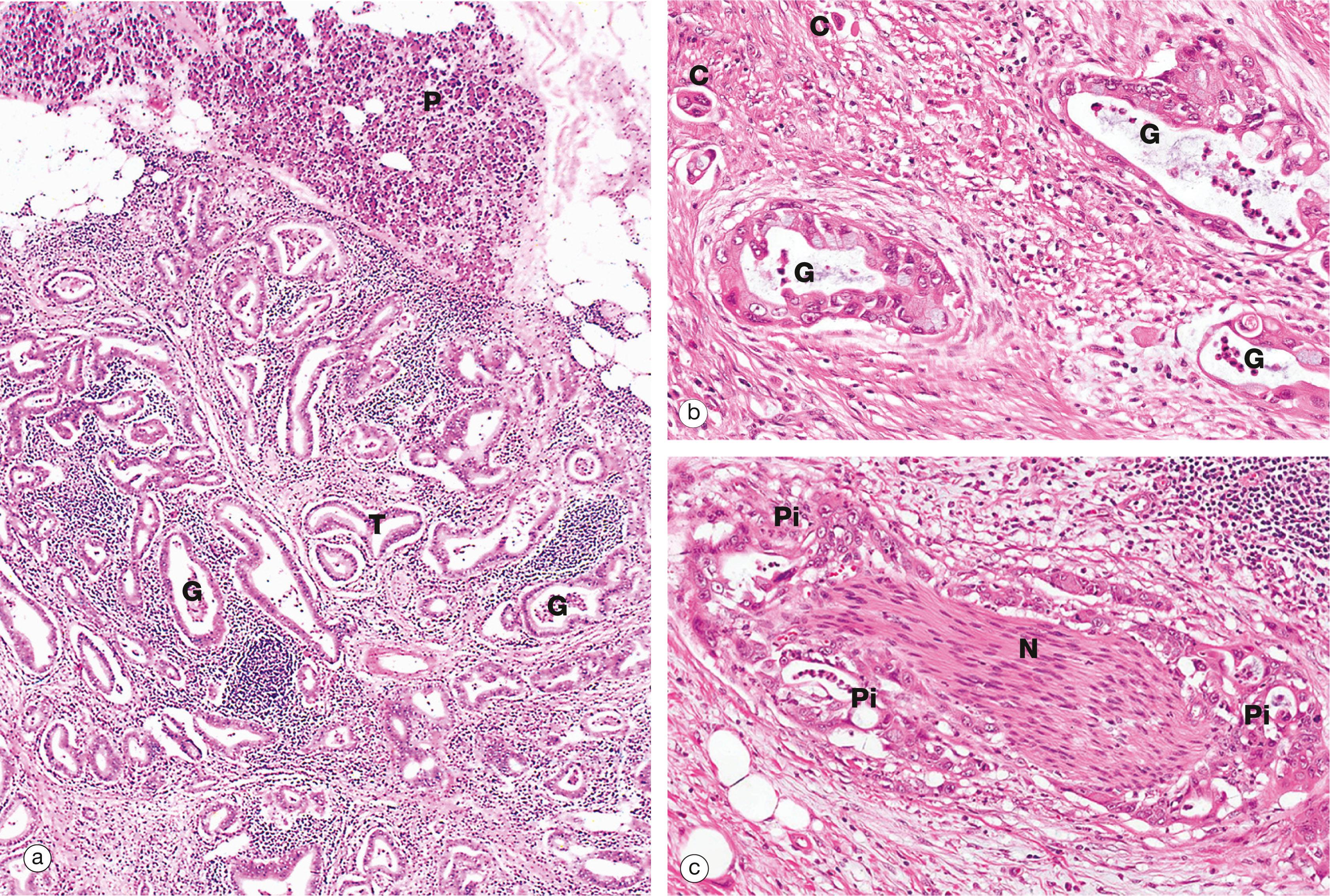
Abnormal concentration and precipitation of the constituents of bile may form stones ( calculi or gallstones ) within the gallbladder or the extrahepatic biliary system. A stone may become impacted in a duct, leading to blockage. Complete blockage of the common bile duct by a stone leads to failure of bile secretion and clinical jaundice (see textbox ‘Jaundice’ ). If the gallbladder is affected by stones, then it may become inflamed, leading to pain ( chronic cholecystitis ). The term cholelithiasis is used to refer to the presence of stones within the biliary system.
Gallstones are formed from the constituents of bile and so they may be composed of cholesterol, bile pigments or a mixture of these. In broad terms, they occur due to an imbalance in the ratio of these normal bile constituents. This is well illustrated by the frequent occurrence of pigment stones in patients with chronic haemolytic anaemias . Excess breakdown of erythrocytes results in increased excretion of the haem breakdown products bilirubin and biliverdin in bile. These then precipitate to form dark, crystalline gallstones which may cause biliary obstruction.
| The normal liver has very diverse functions (see text). As a result, liver disease can produce a wide range of symptoms and signs affecting multiple body systems, some of which are detailed below. | ||
| Sign/symptom | Clinical feature | Mechanism |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here