Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
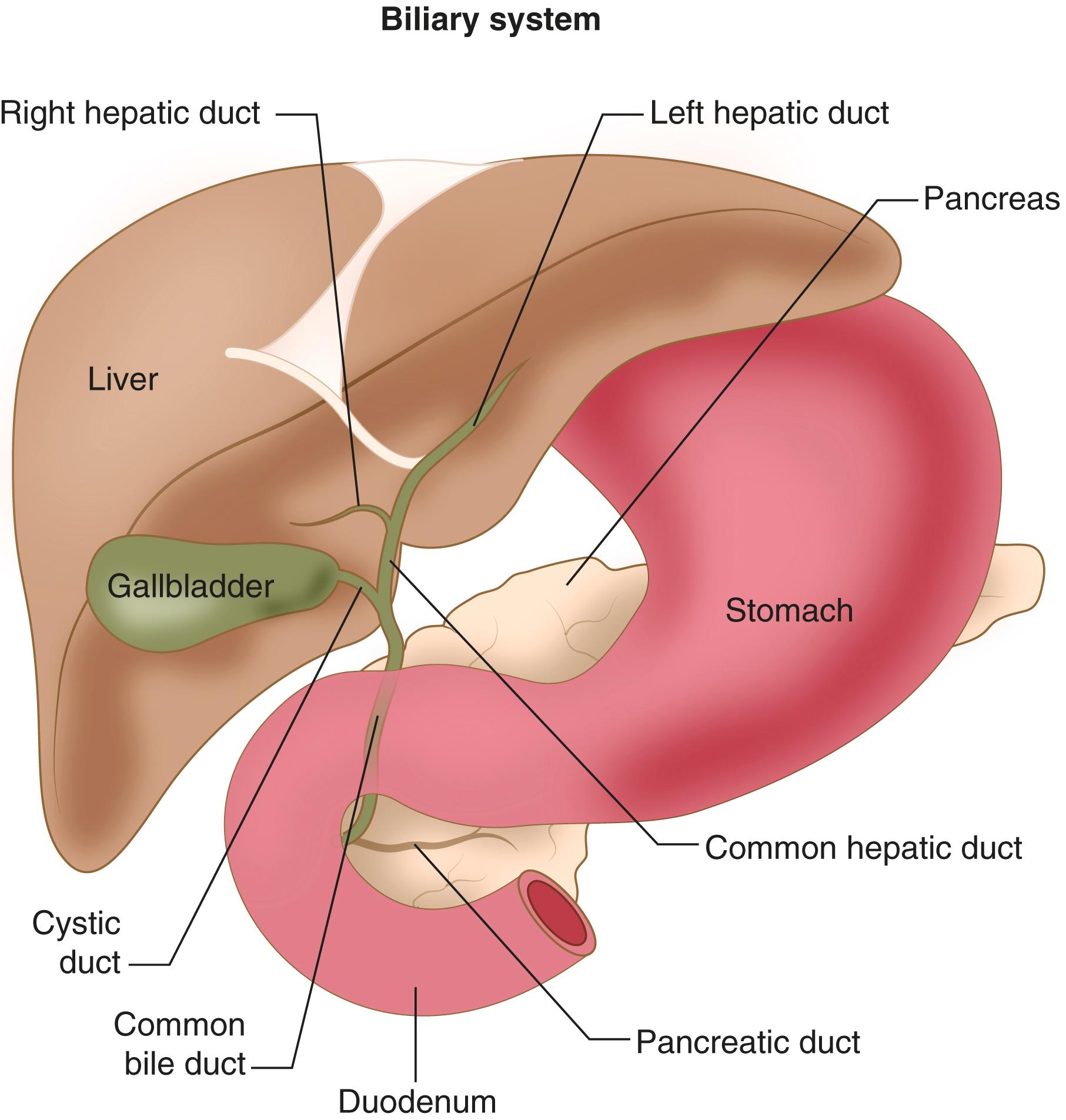
Cancers arising from the liver and biliary tract include hepatocellular carcinoma, cholangiocarcinoma, and gallbladder adenocarcinoma, as well as other less common malignant histologies ( E-Table 181-1 , Fig. 181-1 ). Cholangiocarcinomas are further subclassified by their anatomic location along the biliary tract: intrahepatic (also known as peripheral) or extrahepatic, which includes hilar (also known as Klatskin tumors) and distal locations. These cancers collectively represent the third leading cause of cancer death worldwide and are rising in incidence.
The liver is also a frequent site of metastasis from other primary cancers. The diagnosis of liver tumors must distinguish metastatic disease from primary liver tumors.
| TUMOR TYPE | APPROXIMATE ANNUAL INCIDENCE |
|---|---|
| Hepatocellular carcinoma | 900,000 cases/yr worldwide ∗ |
| Gallbladder carcinoma | 220,000 cases/yr worldwide |
| Cholangiocarcinoma | 10,000 cases/yr in United States † |
| Mixed hepatocellular-cholangiocarcinoma | Rare |
| Fibrolamellar hepatocellular carcinoma | Rare |
| Cystadenocarcinoma | Rare |
| Hepatic endothelioid hemangioendothelioma | Rare |
| Angiosarcoma and other sarcomas | Rare |
∗ Includes cases of intrahepatic cholangiocarcinoma.
† Includes cases of gallbladder cancer and excludes cases of intrahepatic cholangiocarcinoma.
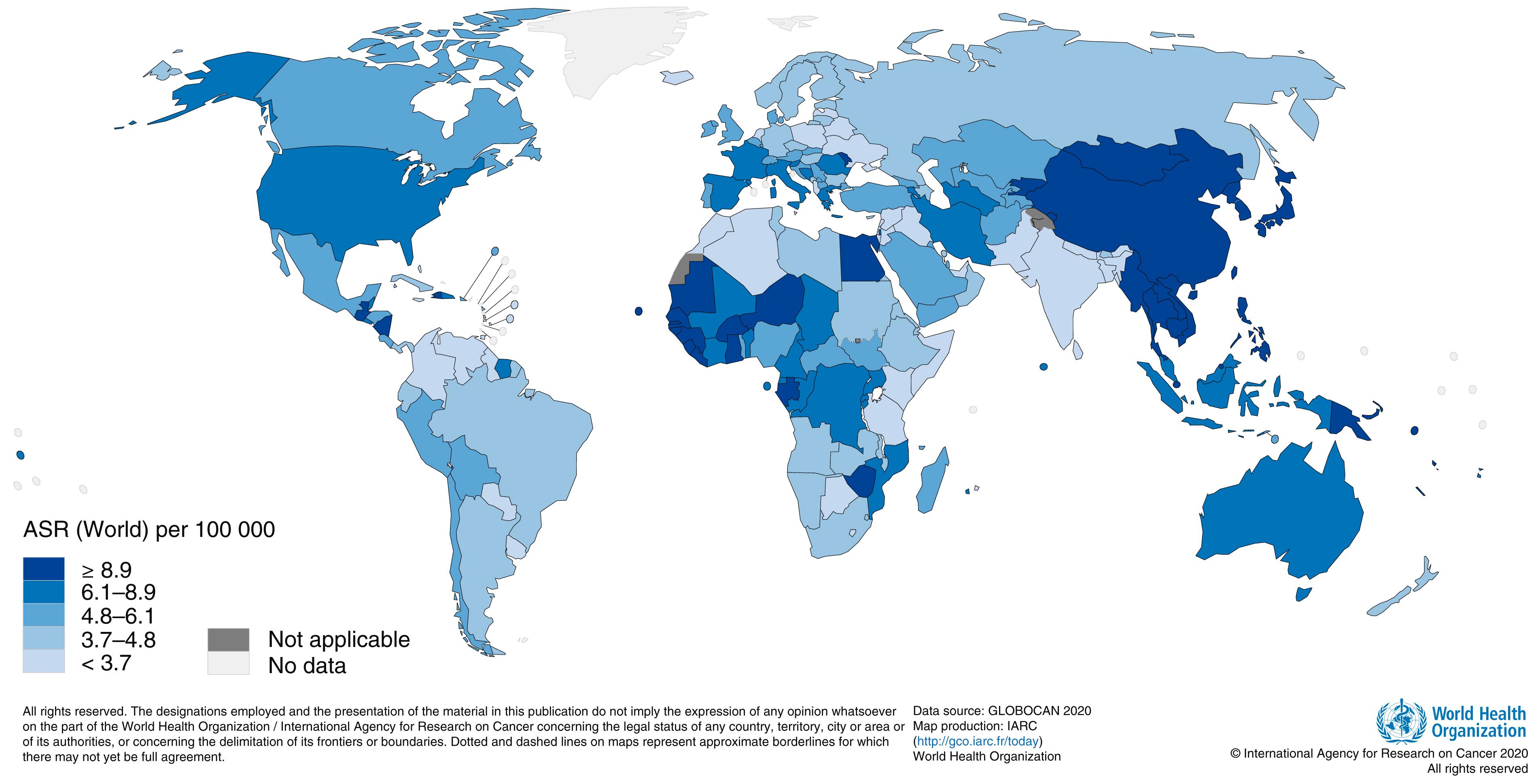
Hepatocellular carcinoma is the most common primary tumor of the liver and the third leading cause of cancer death worldwide. It accounts for approximately 900,000 new cases and 830,000 deaths each year. More than 80% of hepatocellular carcinomas occur in developing countries ( Fig. 181-2 ), owing to an increased prevalence of risk factors, particularly hepatitis B virus and hepatitis C virus ( Chapter 134 ), but rates are also increasing in developed nations ( E-Table 181-2 ). Hepatitis B and hepatitis C viruses together account for more than 80% of all hepatocellular carcinomas worldwide. Alcoholic cirrhosis is another classic predisposing factor. However, nonalcoholic fatty liver disease has surpassed both viral hepatitis and alcoholic cirrhosis as the leading cause of hepatocellular carcinomas in the United States.
| RISK FACTOR | INCIDENCE OF HEPATOCELLULAR CARCINOMA ∗ |
|---|---|
| Asian male HBV carriers over age 40 | 0.4-0.6%/yr |
| Asian female HBV carriers over age 50 | 0.3-0.6%/yr |
| HBV carrier with family history of HCC | Higher incidence than without family history |
| African/North American Blacks with HBV | HCC occurs at younger age |
| HBV carriers with cirrhosis | 3-8%/yr |
| HCV cirrhosis | 3-5%/yr |
| Stage 4 primary biliary cirrhosis | 3-5%/yr |
| Hereditary hemochromatosis with cirrhosis | Unknown |
| α 1 -Antitrypsin deficiency with cirrhosis | Unknown |
| Other-cause cirrhosis | Unknown |
∗ Data from Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the study of liver diseases. Hepatology . 2018;68:723-750.
Nonalcoholic fatty liver disease can lead to steatohepatitis, cirrhosis, and hepatocellular carcinoma. When hepatocellular carcinoma develops in patients with nonalcoholic liver disease without preceding cirrhosis, it is more likely to present at an older age, with a larger tumor burden, and with higher rates of recurrent tumor compared with tumors that develop after patients already have cirrhosis.
Hepatitis B virus is endemic in regions such as Asia and sub-Saharan Africa, and it can be vertically transmitted from mother to fetus in utero. Hepatitis C virus, which may be acquired by intravenous drug use or from blood transfusion ( Chapter 134 ), is another important risk factor for hepatocellular carcinoma. In patients who have cirrhosis caused by hepatitis C virus, the estimated annual risk for developing hepatocellular carcinoma is 3 to 5% per year. Other risk factors for hepatocellular carcinoma include hepatitis D virus (which requires coinfection with hepatitis B virus to be pathogenic), hereditary hemochromatosis ( Chapter 196 ), α 1 -antitrypsin deficiency ( Chapter 132 ), primary biliary cirrhosis ( Chapter 141 ), autoimmune hepatitis ( Chapter 135 ), male gender, and dietary exposure to fungal aflatoxins.
Cholangiocarcinoma is the most common primary biliary tract malignancy and the second most common primary cancer of the liver after hepatocellular carcinoma. The incidence of intrahepatic cholangiocarcinoma appears to be increasing. Although most cases are sporadic, the risk for cholangiocarcinoma is increased in patients who have primary sclerosing cholangitis ( Chapter 141 ), inflammatory bowel disease ( Chapter 127 ), viral hepatitis ( Chapter 135 ), congenital choledochal cysts or other structural abnormalities of the biliary tract, chronic pancreatitis ( Chapter 130 ), obesity ( Chapter 201 ), fluke infections ( Chapter 326 ) and other causes of chronic cholangitis, bile duct adenomas, Caroli disease, and diabetes mellitus ( Chapter 210 ).
Gallbladder adenocarcinomas are rare in the United States but account for about 220,000 cases per year worldwide. The incidence varies geographically, with higher incidence rates reported in India and areas of South America and Asia. Risk factors for gallbladder adenocarcinoma include female gender, chronic cholelithiasis, chronic cholecystitis, history of gallbladder polyps, and abnormalities of the common bile duct ( Chapter 141 ). Calcification of the gallbladder (“porcelain gallbladder”) is often considered a risk factor, but it is only weakly associated with the development of cancer.
Other primary tumors of the liver are much less common, with poorly understood risk factors. Chronic inflammatory conditions, including viral hepatitis, may be associated with the development of combined-histology liver tumors. Exposure to polyvinyl chloride has been implicated in the development of hepatic angiosarcomas. The fibrolamellar variant of hepatocellular carcinoma may occur more commonly in females. Hepatoblastoma tumors occur in infants and children, but almost never in adults.
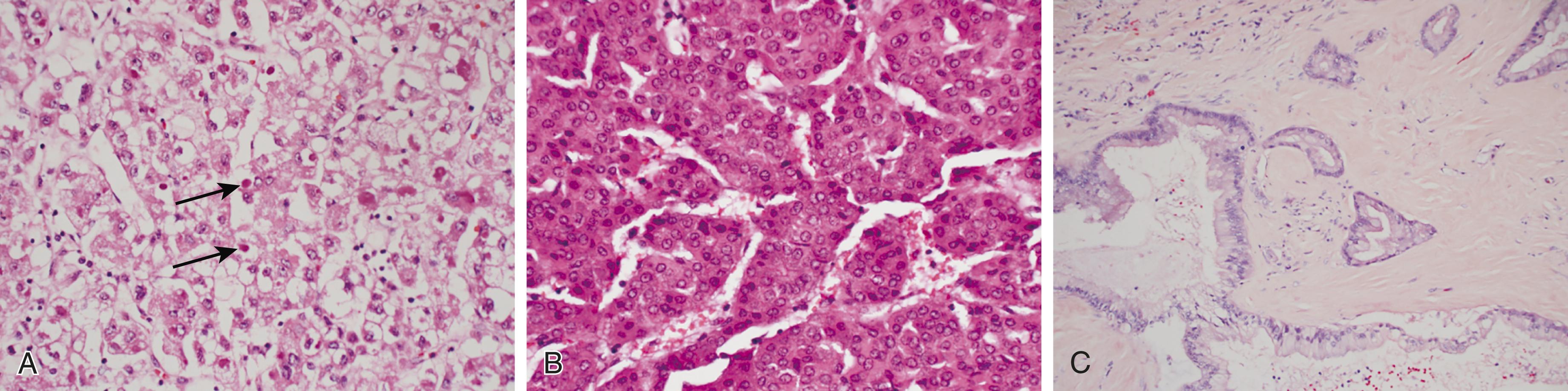
Hepatocellular carcinoma is an epithelial neoplasm that arises from malignant transformation of liver hepatocytes ( Fig. 181-3A and B ). In the majority of cases, the pathogenesis of hepatocellular carcinoma is thought to be a multistep process triggered by underlying liver injury (such as from viral hepatitis, steatohepatitis, alcohol, iron overload, or exposure to aflatoxin). Subsequent inflammation, necrosis, regeneration, cell turnover, and proliferation result in the progressive accumulation of genetic damage and somatic (acquired) mutations. Activation of oncogenes or inactivation of tumor suppressor genes, dysplasia, and subsequently carcinoma can arise. Promoter mutations that result in activation of the TERT gene, which encodes telomerase reverse transcriptase, are seen in approximately 45% of cases, inactivation of the tumor suppressor TP53 is seen in about 30% of cases, and activation of the oncogene β-catenin ( CTNNB1 ) gene is seen in about 25% of cases. Alterations in Wnt , cell cycle, and chromatin-remodeling pathways also have been described.
In hepatitis B-associated hepatocellular carcinoma, a unique mechanism of malignant transformation is direct integration of viral DNA into the host genome. This integration appears to favor specific loci, including activation of the TERT gene promoter.
Cholangiocarcinomas are a histologically diverse group of epithelial cancers that may arise from multiple different liver cell types, including biliary epithelial cells or hepatic progenitor cells, and are often surrounded by a dense stroma with cancer-associated fibroblasts (see Fig. 181-3C ). Cholangiocarcinomas are associated with underlying inflammation and cholestasis, which activate growth factors and a proliferative response. Overexpression of Notch1 and AKT has been implicated in a process by which hepatocytes are converted into the cholangiocytic precursors of intrahepatic cholangiocarcinoma. Molecular and genomic subtypes of biliary tract cancers can also be defined by mutational status and gene expression profiles. For example, isocitrate dehydrogenase-1 ( IDH1 ) gene mutations and fibroblast growth factor receptor-2 ( FGFR2 ) gene fusions each occur in approximately 15% of intrahepatic cholangiocarcinomas.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here