Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
|
|
|
|
|
|
|
|
|
|
Indications for cervical surgical fixation include instability secondary to trauma, infection, degenerative spondylosis, osseous metastasis, pseudarthrosis, rheumatoid disease, destruction of bony elements, and extensive laminectomies and other iatrogenic causes. Goals of treatment include preservation of neurologic function, stabilization, maintenance of anatomic alignment, fusion, and early rehabilitation.
Wiring techniques were the first to be developed. Patterns grew complicated, wires evolved into multifilament cables, and rectangular frames were added. However, wires cannot be used when the posterior elements are deficient or after laminoplasty. The degree of stability is poor, and additional external support (e.g., collar, sternal occipital mandibular immobilizer [SOMI brace], halo vest) is often required. Although cervical pedicle screws are biomechanically stronger and provide more rigid fixation than lateral mass screws, the risk of vascular and neurologic injury is higher, the learning curve is steeper, and quite often the pedicle is too small for the screw or does not have a cancellous center.
Since its description in 1972 by Roy-Camille, lateral mass screw–based techniques have become common procedures for posterior stabilization of the subaxial cervical spine. Early designs were simple screw and plate constructs. Because the interfacet distance in the cervical vertebrae is variable, the fixed hole spacing of the plate markedly limits screw positioning. Furthermore, plates are difficult to contour in three dimensions, are not easily extended to the skull or the thorax, and have been known to cause iatrogenic foraminal stenosis through a lag screw effect. Modern system designs are almost all based on polyaxial screws and connected by rods. They allow the surgeon to place screws in the optimal position in the lateral mass while contouring the longitudinal rods to the lateral mass screws. This chapter provides an overview of pertinent factors and describes the technique of placing cervical lateral mass screws.
A thorough understanding of cervical anatomy is essential. Unlike in the lumbar spine, the cervical nerve root is normally positioned at the lower part of the intervertebral foramen, which corresponds to the middle to lower portion of the lateral mass. On a lateral cervical view, the lateral mass projects as a rhomboid; however, lateral mass morphology can vary from patient to patient and even within the same patient. In particular, compared with C3 to C6, the lateral mass of C7 is more elongated from superior to inferior and is thinner from anterior to posterior (increased height-to-thickness ratio). Pait and colleagues noted in 1995 that the variance in measurements from spine to spine and within the same spine was great enough to render averages clinically unreliable. These investigators proposed that the superolateral quadrant, anterior to which no neurovascular structures are present, be considered the “safe quadrant” and suggested aiming posterior screws in that direction.
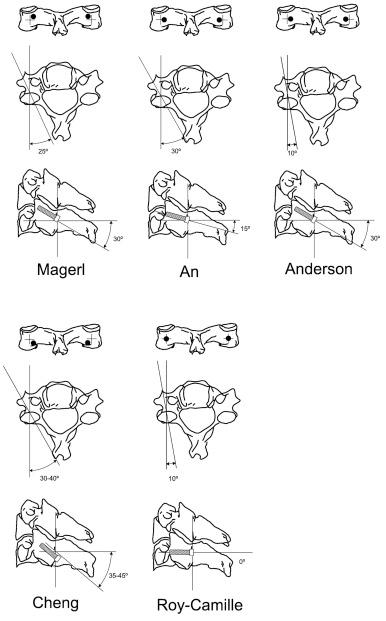
Several different techniques have been described for placement of lateral mass screws. Five trajectories are shown in detail in Figure 43-1 , and this list is by no means complete. All the techniques are compromises that attempt to balance anatomic safety and mechanical competence with ease of placement. Nerve roots, the vertebral artery, facet joints, and, to a lesser extent, the spinal cord are at risk during placement of lateral mass screws. Direct anterior trajectories such as the Roy-Camille are technically straightforward, but the screw length (bite) is shorter and at C6 and C7 has a higher chance of violating the inferior facet joint. Screws that angle cranially (Magerl) have a longer, biomechanically stronger screw tract, but they also have a higher chance of damaging the exiting nerve root and of entering the superior facet joint. A more outward (lateral) trajectory, such as used by the An technique, avoids the vertebral artery but has less bone stock available for the screw to traverse (resulting in shorter screw length) and a higher probability of lateral mass fracture.
Trajectory-based methods rely on the surgeon’s feel of the angle of screw placement, either freehand or by using a mechanical angle guide or C-arm fluoroscopy. Bayley and colleagues proposed aligning the screw trajectory with a constant anatomic reference plane (i.e., parallel to the ipsilateral cervical lamina). The large degree of lateral angulation (up to 50 degrees) provides a reliable safety margin for neurovascular structures, but many patients do not have sufficient lateral mass width for this technique to be performed. Stevens and associates described a technique that is based on the presence of an intact spinous process. The trajectory is aligned parallel to the tip of the spinous process of the vertebra being instrumented and without any lateral angulation. The authors agree with the concept of using anatomic structures for guidance, and their method is by referencing a guidewire placed in the facet joint for the cranial angle, as described in detail later.
Heller and co-workers showed that bicortical purchase provides greater pull-out resistance for lateral mass screws, with a gain of approximately 30%. Stemper and colleagues stated because of superior mechanical stability under single-cycle loading and stiffer response under repeated loading, the use of bicortical lateral mass screws is a superior option for posterior spinal stabilization. The preference at the authors’ institution is for bicortical insertion, although for patients with degenerative disorders without obvious instability, unilateral cortical fixation is usually sufficient.
Using fresh frozen spine segments and in-line pull-out testing, Hostin and associates showed that conversion of a stripped lateral mass screw to an alternate trajectory appears to offer no biomechanical advantage over placement of an increased diameter salvage screw using the same trajectory. Conversion to pedicle screw fixation does provide superior biomechanical fixation, but it is technically challenging, associated with a significant breach rate, and is perhaps best used when lateral mass screw salvage is not feasible (e.g., in cases of fracture). The authors’ protocol is to attempt salvage of a stripped 3.5-mm lateral mass screw by converting it to a 4.0-mm screw in the same path. If the screw is still loose, an attempt is made to convert to pedicle screw fixation if the authors believe that the screw heads connectors can be made to align. As a last resort, that level can be skipped, and the instrumentation can be extended cranially or caudally as necessary.
Several computer-assisted surgical navigation systems are currently available. Although they are theoretically useful, the authors have not found them to make much difference during lateral mass screw placement and do not use them on a routine basis. Malpositioned screws can be identified by stimulation with an electromyography probe and a search for a sustained burst of neurotonic discharge, but again, the authors do not find this necessary on a routine basis.
All the major orthopedic implant manufacturers have their own screw and rod systems. The surgeon should be aware that rods of the same diameter are not necessarily equally rigid, and special connectors, or a transitional rod with varying rod diameters, may be needed to attach a cervical system to a thoracic system (transition rods).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here