Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The advancements in laser and light therapies over the past three decades are built upon the foundation of Albert Einstein's The Quantum Theory of Light . In these prescient 1917 writings, he proposed, amongst other concepts, that light consists of quanta of energy, and he hinted at the notion of amplification. In 1958, Townes and Schawlow described Microwave Amplification by Stimulated Emission of Radiation (MASER). This was further refined by Thomas Maiman as Light Amplification by Stimulated Emission of Radiation (LASER) . Early laser devices, however, were functionally limited by their lack of selectivity. Anderson and Parrish developed the concept of selective photothermolysis whereby laser energy could be used for targeted destruction of skin components (see Ch. 136 ). Their 1983 treatise continues to support our understanding of laser–tissue interactions and still drives new therapeutic applications of lasers in dermatology.
This chapter will consider laser and light applications for both medical and aesthetic purposes as related to the skin. Given the multiplicity of lasers available ( Fig. 137.1 ), the laser surgeon must understand the capabilities and limitations of each device so that the appropriate system can be selected and the parameters tailored to treat the intended target. Safe and effective laser therapy is achieved when the operator understands the nature of the target, its location in the skin, and the potential collateral damage. Other energy-based devices, such as those that utilize radiofrequency waves, intense focused ultrasound or microwaves, are also discussed.
The earliest lasers used by dermatologists were applied to vascular lesions and consisted of continuous or quasi-continuous wave lasers, which emitted a constant beam of light. These included argon (488, 514 nm), argon pumped tunable dye (488–638 nm), copper vapor and copper bromide (511 nm, 578 nm), potassium titanyl phosphate (KTP, 532 nm), and krypton (568 nm) lasers. Although these lasers had wavelengths that corresponded to the hemoglobin absorption spectrum, the nature of their continuous beams generally induced nonspecific thermal damage to surrounding structures, leading to scarring and dyschromia. The root of the problem, a mismatch between the laser pulse duration and the thermal relaxation time of the target tissue (see Ch. 136 ), was effectively resolved once it was understood that laser pulse duration should approximately match the thermal relaxation time of the targeted tissue.
The pulsed dye laser (PDL) is considered to be the laser of choice for the treatment of many cutaneous vascular lesions, especially facial telangiectasias, port-wine stains (PWSs), superficial hemangiomas, poikiloderma of Civatte, and erythematotelangiectatic rosacea . Hypertrophic and keloidal scars, psoriasis, and warts are also amenable to treatment with PDL. While the initial PDL systems emitted 577 nm yellow light, slightly longer wavelength PDL devices (585 or 595 nm) were subsequently adopted to allow deeper tissue penetration of up to 1.2 mm.
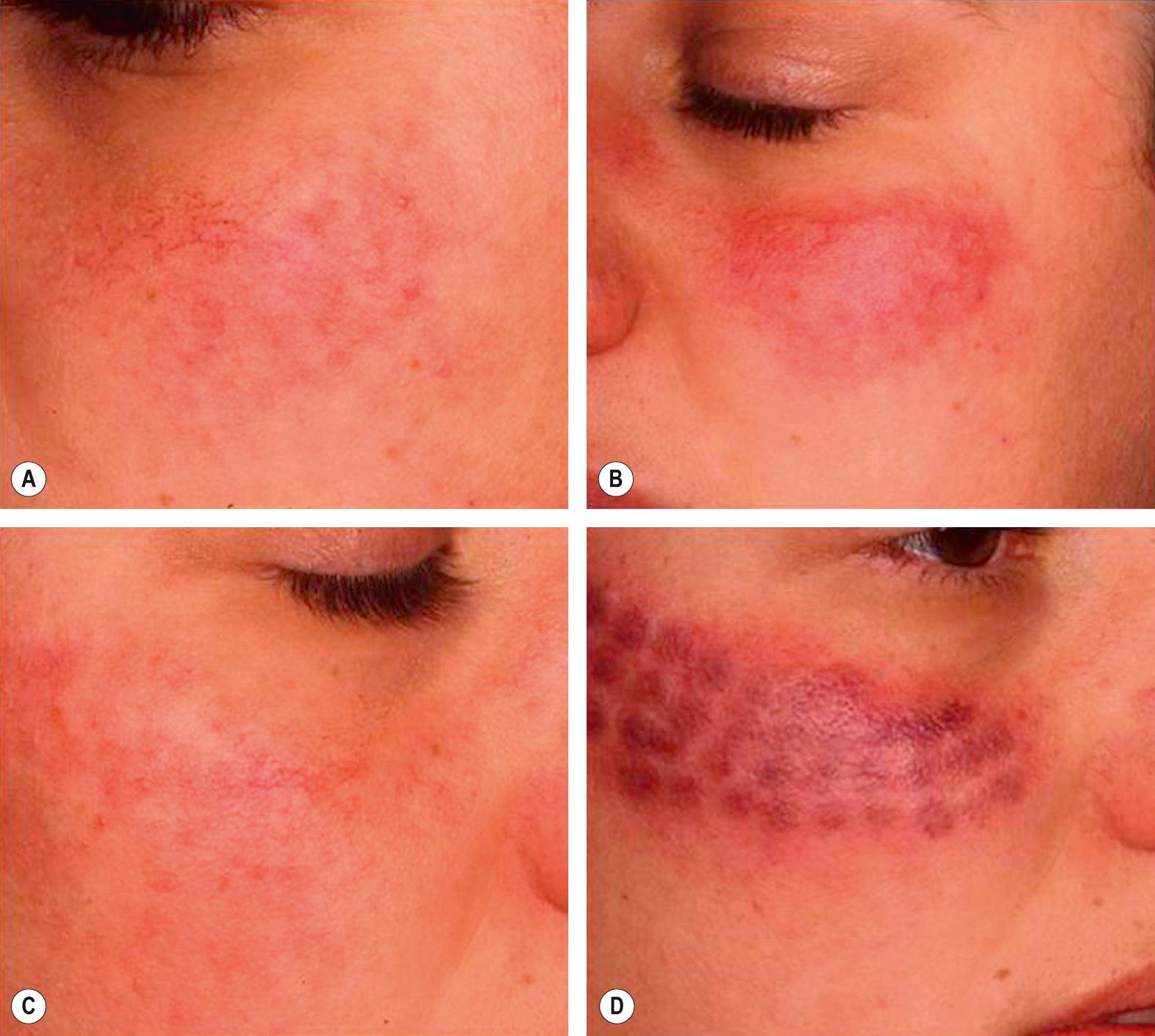
The choice of appropriate PDL parameters affects tissue response, in terms of both efficacy and appearance. Short pulse durations (0.45–3 millisecond [ms]) cause a purpuric reaction related to intravascular coagulation or vessel leakage ( Fig. 137.2 ). While very effective for telangiectasias, the bruised appearance is not cosmetically acceptable to many patients. Although slightly less effective, longer pulse durations (6–10 ms) with multiple passes or “pulse stacking”, consisting of application of a rapid succession of pulses to a particular location with cooling to achieve “purpura-free” treatments, is quite effective and less noticeable. The latest generations of PDL modulate this approach by dividing each pulse into eight micro-pulses. This is said to be more selective, to provide uniform vascular heating with a reduction in purpura, and to be more comfortable.
Epidermal protection during laser treatments, including those with PDL, is critical. Cooling helps to reduce blistering, crusting, and subsequent dyspigmentation, i.e. hypo- and hyperpigmentation. The most common cooling strategies are contact cooling, forced cold air, and cryogen spray. The Syneron-Candela PDL systems incorporate cryogen spray cooling (Dynamic Cooling Device™) which is deployed immediately before the light pulse, while Cynosure systems use forced cold air. In addition to protecting the epidermis from non-selective thermal damage, cooling allows for the use of higher fluences, with improved efficacy.
KTP 532 nm laser light is produced by passing 1064 nm light from an Nd:YAG (neodymium-yttrium-aluminum-garnet) laser through a potassium titanyl phosphate (KTP) crystal, which effectively halves the wavelength and doubles the frequency. Since this wavelength closely corresponds to the first absorption peak of hemoglobin at 542 nm, the KTP laser can be used to effectively treat some vascular lesions (e.g. telangiectasias) in a purpura-free manner (see Fig. 137.2 ). In addition, this laser is a popular device for the removal of lentigines and other epidermal pigmented lesions. While this laser is best employed in patients with skin phototypes I–III, it can used in darker skin types (IV–VI) for unique applications, such as dermatosis papulosa nigra.
The deeply penetrating Nd:YAG 1064 nm laser has significantly less hemoglobin absorption than the wavelengths of the PDL or KTP lasers. However, its absorption by melanin is also very limited. The latter property theoretically enhances the safety profile of the 1064 nm laser in patients with darker phototypes. This laser can be used to treat deeper vascular lesions and spider veins up to 3 mm in size . Because of its poor coefficient of absorption by hemoglobin, much higher fluences are required to produce transmural heating of blood vessels. As a consequence of the higher fluences and longer pulse widths, this wavelength has a narrow window of safety, with a significant potential for volumetric heating and collateral damage; in addition, it tends to be quite painful. Cooling is critical for epidermal protection and pain control, as well as to reduce the risk of scarring from nonspecific thermal injury. Nd:YAG lasers should be used with extra caution when treating vascular lesions.
Intense pulsed light (IPL) systems emit filtered polychromatic light with wavelengths ranging from visible to near infrared (500–1200 nm). Sophisticated filtering and pulsing systems prevent unwanted wavelengths from damaging the skin, and they have made this device more specific and quite versatile. Handpiece cooling is a useful feature present in some devices, and it can be employed to provide epidermal protection, while at the same time allowing greater fluences to reach deeper targets. IPL systems can be used to treat a number of conditions, including rosacea, PWS, hemangiomas, poikiloderma of Civatte and lentigines, as well as provide overall photorejuvenation.
Cold ultrasound gel or aloe vera gel should be applied as a supplementary technique in order to diffuse surface heat and to act as a “heat sink” away from the epidermis. The gel also reduces the refractive index between air and skin, thus allowing better penetration and absorption of light. In addition, it enhances gliding of the handpiece from one location to the next.
In spite of these measures, thermal injury to the epidermis can still occur, leading to blistering, scarring, and permanent pigmentary alterations. This is generally operator-dependent, with a greater risk when treating patients with a tan or darker skin phototypes ( Fig. 137.3 ). IPL is most commonly used for patients with phototypes I–III with chronic photodamage or for hair removal. For treatment of patients with more darkly pigmented skin, longer wavelength filters or lower fluences plus longer pulse widths can be used ( Fig. 137.4 ). Filters can also be used for other specific indications, e.g. treatment of vascular lesions.


The authors' preferred technique is to deliver multiple passes to a particular treatment area, with each subsequent pass oriented at a different angle. This allows for uniform, consistent coverage and prevents zebra-like pigmentary irregularities and skip areas. If double or triple pulses are utilized in any one area, adequate time for epidermal cooling should be allowed between passes. The observable endpoints of IPL treatment are darkening of lentigines (see Fig. 137.4B ) and either a disappearance or a darker blue appearance of telangiectasias.
As with any of these devices, the initial pulses should be assessed in terms of the tissue response. Potential problems that should be avoided are excessive blanching, bruising, and production of the Nikolsky sign or other signs of excessive non-selective heating. If cooling is being used, it should be assessed for efficacy. Additionally, care must be taken to avoid inadvertent photoepilation of eyebrows, and, in men, bearded skin.
Although patients most commonly present with telangiectasias and rosacea, one should also be familiar with the latest techniques available for the treatment of PWSs and hemangiomas. The target chromophore in vascular lesions is oxyhemoglobin, with absorption peaks at 418, 542 and 577 nm (see Fig. 136.3 ). While the primary target is hemoglobin, the structurally dynamic nature of the skin does not allow for simplistic “targeting”. Factors such as blood vessel depth, thickness, and skin phototype are also highly relevant considerations when treating vascular lesions.
An equally important consideration is the structures that the laser surgeon wishes to avoid, such as normal epidermal melanocytes, hair follicles, and the epidermis as a whole. Therefore, while the above wavelengths allow for maximal absorption, longer wavelengths are associated with less melanin absorption and deeper penetration. The most commonly used devices for the treatment of vascular lesions include IPL and the 532 nm KTP, 595 nm PDL, and 1064 nm Nd:YAG lasers. Other systems such as the 755 nm alexandrite and the 940 nm diode lasers also play an important role in the treatment of vascular lesions ( Table 137.1 ).
| LASERS AND OTHER DEVICES USED FOR THE TREATMENT OF VASCULAR LESIONS | |||||
|---|---|---|---|---|---|
| Laser/device | Wavelength (nm) | Fluence (J/cm 2 ) | Pulse duration (ms) | Target structure | Applications |
| Skin-surface application | |||||
| Variable-pulsed KTP laser | 532 | Up to 240 | 1–100 | Telangiectasia, venulectasia | Facial telangiectasias, erythematotelangiectatic rosacea, cherry angiomas, leg telangiectasias, venous malformations |
| Pulsed dye laser | 585, 590, 595, 600 | Up to 40 | 0.45–40 | Telangiectasia | Port-wine stains, erythematotelangiectatic rosacea, facial and leg telangiectasias, cherry angiomas, spider angiomas, venous lakes, infantile hemangiomas, hypertrophic scars, striae rubrae, verrucae |
| Long-pulsed alexandrite laser | 755 | Up to 100 | 3–100 | Venulectasia, telangiectasia | Leg telangiectasias (“spider veins”), venous malformations, port wine stains |
| Diode laser | 800 | 10–100 | 5–400 | Venulectasia, telangiectasia | Leg venulectasias and telangiectasias (“spider veins”), blue reticular veins, venous malformations |
| Long-pulsed Nd:YAG laser | 1064 | 5–900 | 0.25–500 | Venulectasia, telangiectasia | Leg venulectasias and telangiectasias (“spider veins”), blue reticular veins, facial telangiectasias, venous lakes, venous malformations |
| Intense pulsed light | 400–1200 | 10–80 | 2–200 | Telangiectasia, venulectasia | Erythematotelangiectatic rosacea, leg telangiectasias (“spider veins”) |
| Endovascular application | |||||
| Diode lasers | 810, 940 | Varicose veins | Saphenous vein insufficiency | ||
| Nd:YAG laser | 1320 | Varicose veins | Saphenous vein insufficiency | ||
| Radiofrequency energy source | Radiofrequency | Varicose veins | Saphenous vein insufficiency | ||
Clinical improvement is best achieved by photothermal vascular damage . As the pulse width approximates or exceeds the thermal relaxation time of the target vessel, photothermal damage results. This induces intravascular thrombosis and subsequent collagenous fibrosis of the blood vessel wall and adjacent tissues . These changes result in an immediate purpuric reaction (see Fig. 137.2D ). Given the unwanted cosmetic appearance of the latter, which can last for 2 weeks, longer pulse widths (>6 ms) are often used, as they produce more gentle heating of the target vessel and avoid bruising altogether. However, some degree of intravascular thrombosis may be a prerequisite for clinical improvement and resolution of vascular lesions, as is the case in PWSs.
One of the first clinical applications of laser therapy was treatment of congenital vascular lesions, namely PWSs. PWSs are capillary malformations that involve primarily the mid to superficial dermis; they occur in up to 0.5% of newborns and initially present as faint, light pink patches. These vascular anomalies are cosmetically and psychologically problematic as they are frequently located on the face. Approximately 5–10% of patients with unilateral PWSs involving V1 have Sturge–Weber syndrome, with associated ocular and neurologic involvement. Both Sturge–Weber syndrome and non-syndromic PWSs have been associated with a somatic activating mutation in GNAQ . When located on the extremities, PWSs may be a sign of Klippel-Trenaunay or Parkes Weber syndrome, with associated tissue hypertrophy and deep vascular malformations (see Ch. 104 ).
Prior to laser therapy, PWSs were treated via destructive modalities such as cryosurgery, dermabrasion, and X-ray radiation. These therapies often resulted in disfiguring scars. An early and relatively successful treatment of PWSs utilized the continuous wave argon laser (488 and 514 nm). Despite the wavelength's relative specificity for its vascular target, this laser caused marked scarring in up to a third of patients . The latter was caused by nonspecific thermal injury due to the exposure time of the beam (~200 ms) being in dramatic excess of the thermal relaxation time of the PWS vessels (~1–10 ms) .
A therapeutic paradigm shift evolved with the concept of selective photothermolysis and the development of the PDL, which was specifically designed to treat PWSs. The first study, conducted by Tan et al. , demonstrated significant fading in all 35 patients (ages 3 months to 14 years) after an initial treatment and complete clearance after an average of 6.5 treatments. Most remarkably, the sequelae were minor, with some patients experiencing short-term hyperpigmentation and only two patients developing shallow depressed scarring. Although subsequent studies found significantly lower clearance rates, this initial study demonstrated a pattern of safety and efficacy of PDL for treatment of PWSs.
While the early PDLs emitted a 577 nm wavelength, the current PDL systems deliver 585 and 595 nm, allowing targeted delivery of laser energy deeper into the skin with increased efficacy. These longer wavelengths are less well absorbed by hemoglobin, but they penetrate deeper into the vascular malformation, inducing a more even heating of the PWS . Addition of epidermal cooling has allowed for the use of much higher fluences. Commonly used settings range from fluences of 4 to 15 J/cm 2 with pulse widths of 1.5–10 ms with a 7–12 mm spot size . Larger spot sizes are associated with deeper energy penetration, but the fluence should be moderated with increasing beam diameter in order to avoid thermal damage.
For both technical and psychological reasons, early treatment of PWSs is recommended. As compared to infantile hemangiomas, the dilated and ectatic vessels of PWS are not proliferative nor do they self-involute. Their total surface area becomes larger, in proportion to the growth of the child, and many become thicker (with soft tissue hypertrophy), darker in color, and deeper. As such, their treatment becomes clinically more challenging and often requires the use of lasers with longer wavelengths, along with higher fluences and longer pulse durations, in order to effectively treat the deeper and thicker vessels. Studies support this notion and have demonstrated that the extent of clearance is dependent on lesion size and depth . From a psychological standpoint, PWSs have been shown to impact social and cognitive development during childhood and can have lasting repercussions on adult social relationships . In addition, early treatment permits shorter treatment sessions (as the lesions are smaller), fewer sessions, and may allow resolution of the capillary malformation prior to the child developing memory of the treatment and its associated stressors. Lastly, laser treatment in children younger than 6 months of age has been demonstrated to be safe and effective .
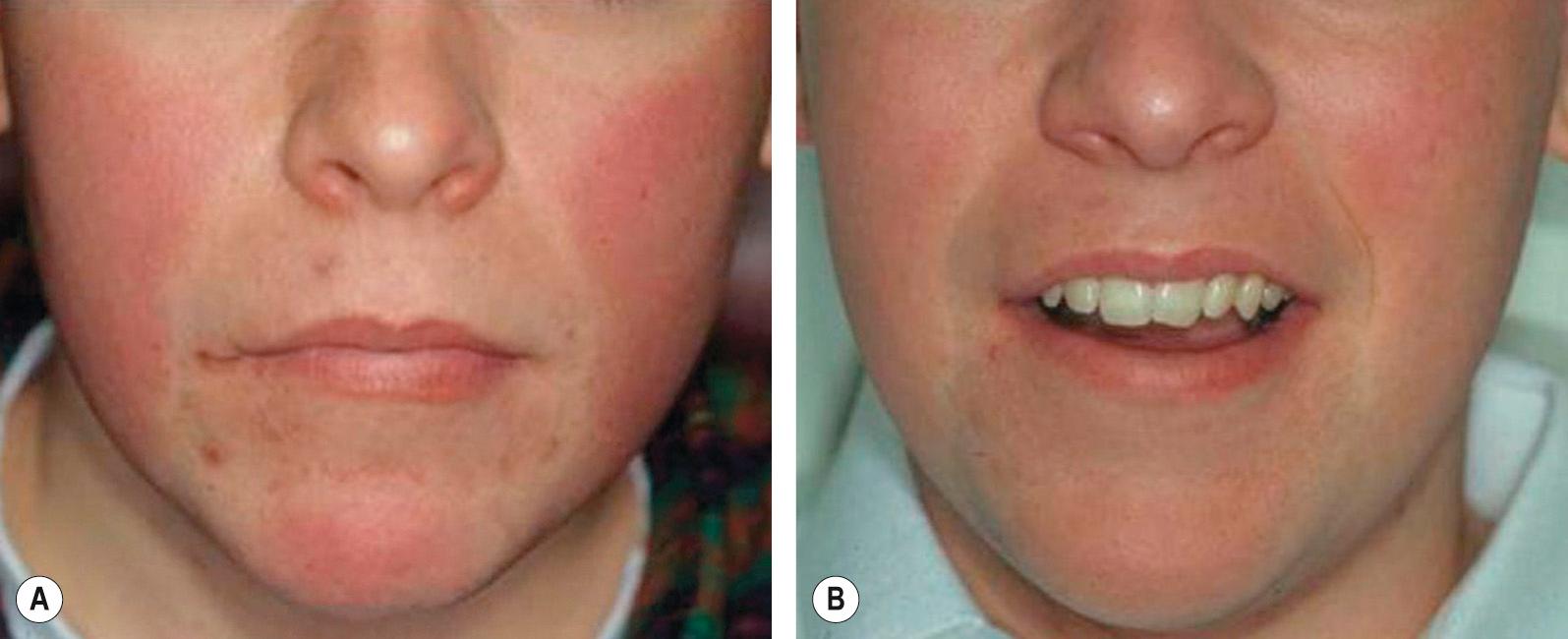
While 70% of PWSs will have good or very good improvement following treatment ( Fig. 137.5 ), a minority (<10%) will have very modest or no improvement. The degree of PWS clearance is dependent on several factors including the size of the lesion and its anatomic location . For example, centrally located facial lesions (i.e. medial cheeks, upper lip, and nose) require multiple sessions for improvement and tend to be more treatment-resistant as compared to lesions located in the periorbital region or on the forehead, lateral cheeks, or chin. Classically, treatment-resistant areas of PWSs, which may correspond to more deeply situated vessels, are distributed within the second branch of the trigeminal nerve (V2). Likewise, PWSs on distal extremities are more treatment-resistant and require a more aggressive approach. Although a remarkable response can be obtained after one laser treatment, treatment of PWSs typically requires multiple (10 or more) sessions.

Given that PWSs are composed of various-sized blood vessels, each with its own required treatment parameters, the PDL may prove inadequate in eliminating the entire capillary malformation. A poor response may be related to poor laser penetration, a mismatch of parameters to vessel size, inadequate vascular heating, or scarce or poor chromophore uptake . Given the limitations of the PDL, resistant components of PWSs may also be treated with the alexandrite laser or IPL.
Representing the most common tumor of infancy, hemangiomas have a predilection for the head and neck region (60%), followed by the trunk and the extremities. They are present in 1–2% of neonates and there is a higher incidence in premature infants. These tumors are classically absent or very small at birth, but then appear and/or grow rapidly within the first few weeks of life. Infantile hemangiomas may have both superficial and deep components, with the superficial portions appearing red and the deeper components appearing blue. They can be categorized as focal or segmental (see Ch. 103 ) . Their natural maturation involves a proliferative phase, a static phase, and an involutional phase. Although hemangiomas can regress leaving the affected skin with normal texture and color, many heal with hyper- or hypopigmentation and atrophy or fibrofatty change (see Fig. 103.9 ).
Treatment of infantile hemangiomas, if any, should be tailored to the specific lesion, with consideration of its location, size, proliferative rate, and whether it is likely to produce a functional or anatomic deficit. Complicated infantile hemangiomas require a multidisciplinary approach, involving dermatology, pediatrics, interventional radiology, otolaryngology, plastic surgery, and ophthalmology. Currently, oral propranolol is a mainstay of therapy for infantile hemangiomas that threaten vital functions, are potentially disfiguring, or have severe ulceration . Other therapeutic options include monitoring, topical timolol (for thin lesions), corticosteroids (topical, intralesional or systemic), laser therapy, and less often surgical excision.
Although the role of laser therapy in the treatment of infantile hemangiomas is still controversial , in some studies PDL has been shown to slow progression, decrease time to involution, and promote healing of ulcerated lesions . A retrospective study of 90 patients with infantile hemangiomas treated with PDL demonstrated a significant improvement in color and decrease in thickness in 81% and 64% of patients, respectively . Combining systemic β-blockers with laser therapy may lead to a more rapid response and enhanced resolution; for example, in one retrospective study of infants with segmental facial hemangiomas treated concurrently or sequentially (propranolol followed by PDL), there was more complete clearance over a shorter time period following concurrent or sequential therapy (3 and 6 months, respectively) compared to propranolol alone (almost 10 months) .
Epidermal protection is critical in the treatment of infantile hemangiomas. Ulceration, scarring, and pigmentary changes can occur if the epidermis is not adequately protected via cooling or if excessively high energies are employed.
Patients frequently present with facial telangiectasias and they are most commonly associated with chronic photodamage and rosacea. However, telangiectasias also occur on the face and elsewhere in the setting of liver disease, autoimmune connective tissue disorders, surgical scars, and misuse of topical corticosteroids. Facial telangiectasias are typically located on the nose, cheeks and chin; they measure 0.1–1.0 mm in diameter and therefore are commonly treated with PDL, KTP laser, or IPL. When the PDL is used with short pulse durations, significant clearance can be achieved, albeit with significant bruising (see Fig. 137.2D ). Clearance of facial vessels can be achieved with non-purpuric fluences or treatments that employ fluences ranging from 6.5 to 8.5 J/cm 2 with longer pulse durations (6–20 ms) using 7–12 mm spot sizes. At these settings, multiple passes and/or pulse-stacking techniques are typically employed to improve efficacy. Additionally, multiple treatment sessions may be required . These techniques can be particularly beneficial for patients with recurring flushing and central facial erythema ( Fig. 137.6 ).
Treatment of telangiectasias with the KTP laser induces little or no bruising compared to the PDL (see Fig. 137.2 ), but edema can occur. Larger-caliber, darker, deeper facial vessels can be effectively treated with the Nd:YAG laser, particularly in dark-skinned patients. However, to compensate for the diminished absorption of 1064 nm light by hemoglobin (nearly 10-fold less compared with 595 nm light), an increased fluence is required, making vigorous cooling necessary both for epidermal protection and to reduce patient discomfort. Finally, IPL is commonly used for purpura-free treatment of facial telangiectasias utilizing a 550 or 560 nm cut-off filter. The treatment endpoint for telangiectasias is vessel spasm or the change of the vessel color to a more dusky appearance.
Poikiloderma of Civatte is a hallmark reflection of photodamage and involves the lateral aspects of the cheeks, neck and upper chest. While a prominent component is telangiectasias, there is also epidermal atrophy and actinic dyspigmentation. Comprehensive treatment requires consideration of each component. Options include IPL, PDL and KTP laser; newer devices such as the fractionated ablative and non-ablative lasers can also be used. When there is insufficient overlap of adjacent PDL pulses, a persistent “honeycomb-like” appearance may occur, with circles of improvement in color, texture and tone surrounded by a network of relatively untreated skin ( Fig. 137.7 ). This mottled look can require multiple treatments to eradicate.

Since IPL can favorably improve both dyspigmentation and telangiectasias, this system is perhaps more ideally suited to treat poikiloderma of Civatte. Several studies have reported 50–75% improvement in both the vascular component and the actinic dyspigmentation, with a low side-effect profile . The pertinent short-term side effects are transient erythema and intentional darkening of lentigines, which all disappear in about a week. Although “footprinting” is possible with IPL, it is far less common than with PDL, given the larger size of the crystal IPL handpiece. Additionally, use of a multiple-pass technique applied in different orientations tends to minimize this unintended “footprint” consequence.
“Spider veins” of the legs affect approximately 80% of men and women in the US . These telangiectasias and venulectasias are red and blue in color, measure 0.2 to 2 mm in diameter, and develop in dependent areas, predominantly the legs. While a number of spider veins appear independently of deeper vascular disorders, a surprisingly high percentage can be improved by treating deeper underlying venous disease. While the superficial venous system is located in the skin, subcutaneous tissue and superficial fascia, the deep venous system is located within underlying muscle, with the two plexuses interconnected by perforating veins (see Fig. 155.1 ) . Whether as a consequence of age, hormonal or genetic factors, or from trauma to the vessel wall, venous valvular incompetence produces increased hydrostatic pressure and ultimately vessel dilation (see Fig. 105.2 ).
Whereas facial telangiectasias are generally superficial, small in caliber, and have normal hydrostatic pressures, leg veins are larger in diameter, thicker in caliber, and are situated more deeply within the skin . Additionally, as in any treatment site, there is heterogeneity in the size, color, and caliber of ectasias. These properties make treatment of leg veins even more challenging. While sclerotherapy is still the first-line therapy for spider veins (see Ch. 155 ), laser treatment is a viable option in a minority of patients (see Table 137.1 ). The latter include those with needle phobias, telangiectatic matting, ankle veins, and lack of a favorable response to sclerotherapy . Also, laser therapy may be advisable in patients with a previous history of adverse reactions to sclerosing agents. The PDL and KTP laser can be used to treat small-caliber, pink and red blood vessels which are too fine to cannulate with sclerotherapy needles, e.g. the telangiectatic matting that can be a consequence of prior sclerotherapy.
The target chromophore for leg veins is hemoglobin. While the 532 nm KTP laser, 585–595 nm PDL, and IPL are well absorbed by this target, the more limited depth of penetration does not allow for consistent treatment of vessels >1 mm in width located at depths >1.0 mm . The results with IPL devices are inconsistent, unpredictable, and vary depending on the selected parameters. Furthermore, these devices have more unfavorable side effects compared to sclerotherapy. Brown discoloration following PDL occurs in 20–40% of patients and can persist for 3 months or longer. This side effect may be related to hemosiderin deposits from red cell extravasation. Many laser surgeons (including the authors) have used the long-pulsed Nd:YAG laser for the treatment of larger, deeper leg veins. While there is no doubt that some leg veins can be cleared, the pain, postinflammatory hyperpigmentation, and potential for scarring have many clinicians avoiding this device for this indication.
Given that leg veins are heterogeneous in their color, size, caliber and depth, and that many result from venous valvular incompetence, duplex ultrasonography can assist in determining the most appropriate treatment strategy. Combination therapy using endovenous lasers, ambulatory phlebectomy, and sclerotherapy may represent the best approach for long-term, successful treatment of lower extremity ectasias (see Ch. 155 ). Synergistic improvement has been demonstrated when these treatments were used in combination .
Verruca vulgaris is caused by the human papillomavirus, which induces epidermal hyperplasia and neovascularization in affected skin. The use of lasers is said to be based on the principle of targeting their vascular component, which is evident histologically as dilated blood vessels within the dermal papillae. Early on, successful treatment was reported with the copper vapor laser, presumably by its inducing vascular coagulation of these reactive vessels . Use of the PDL has been shown to induce intravascular thrombosis and vessel wall necrosis in patients with verrucae . However, the nonspecific heat effect from lasers is likely the main mechanism underlying wart clearance with laser therapy. “Laserthermia” of warts, particularly with the Nd:YAG laser, has produced clearance in 75% of patients . The mechanism may involve coagulation of epidermal proteins and blood vessels, with stimulation of a reactive inflammatory response. Although a similar tissue response is likely caused by carbon dioxide ablation of verrucae, response rates have been more variable, ranging from 30% to 80% . Most notably, scarring and onychodystrophy can result from treatment of periungual verrucae with such ablative laser therapies .
Currently, the PDL is the most commonly used laser for the treatment of recalcitrant verrucae. A notable lack of bleeding and scarring makes this laser a favorable choice. Given the limited penetration of the PDL, hyperkeratotic portions of the wart are first pared down. If bleeding occurs, hemostasis should be achieved, being careful to avoid application of flammable topical agents to the treatment area. Then, the lesions are treated until a dusky gray color is seen. However, rather high fluences are utilized, making this treatment quite painful, especially on the fingers. Depending upon the pain tolerance of the patient, digital nerve blocks may be needed. This procedure can be repeated every 2–4 weeks until clinical resolution.
Clearance rates vary from 20% to 95%, and this range has been attributed to the variability (between studies) in the number and frequency of treatments as well as applied fluences. Despite these data, absolute benefit of the PDL over “conventional therapy” (consisting of cryotherapy and cantharidin) was not established in a prospective randomized trial. In fact, the two arms of the trial were similar in the percentage of patients with complete verruca clearance and the number of treatments needed for complete responses . While laser therapy for verrucae is not exclusively beneficial, it does supplement the dermatologist's armamentarium in the treatment of these recalcitrant lesions.
Pyogenic granulomas (PGs) are idiopathic, abruptly appearing, vascular neoplasms that tend to grow rapidly and bleed easily. Over half of these lesions recur after electrocoagulation, presumably because such desiccative treatments fail to ablate the deeper vascular components . Both the argon and CO 2 lasers have been used to treat these neoplasms. More specific targeting of the vascular nature of PGs has been attempted with the PDL, whether used directly on the lesion or in combination with glass slide diascopy to blanch out superficial components. Higher success rates may be achieved with antecedent removal of the papular component (by shave or electrodesiccation techniques) prior to PDL targeting of the more deeply situated vessels. While shave removal followed by desiccation is still the first-line treatment for most patients, less scarring is noted with the PDL, when used either with modest fluences (1.5 ms pulses) without cooling or multiple stacked pulses (5–10 ms) with cooling .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here