Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
“Resuscitation Sequenced Intubation” for managing critically ill patients and the physiologically difficult airway has become an accepted term describing the process of intubation and transition to positive-pressure ventilation that poses significant risk to the patient in an at-risk cohort.
Just as less invasive airway management may be better suited for shockable rhythm cardiac arrests where early return of spontaneous circulation is more likely, there is evidence that for nonshockable rhythms a more advanced airway management such as an endotracheal tube (ETT) is associated with improved outcomes.
Elective tracheal intubation is indicated for patients requiring anesthesia for major surgery when controlled ventilation, resuscitation, airway access, patient positioning, and duration of surgery are factors in the overall airway plan.
Avoiding hypoxemia, hypocapnia, and hypotension, and early access to imaging and neurosurgical care are the priorities for managing patients with traumatic brain injury. While early airway, oxygenation and hemodynamic support for trauma may be needed, this does not necessarily mean prioritizing early intubation.
Tracheal intubation protects against aspiration of gastric contents in anesthetized patients; however, the use of a supraglottic airway (SGA) is not associated with an increased risk of pulmonary aspiration compared with an ETT.
In 1952, Macintosh wrote “Whatever laryngoscope is used, the principles of laryngoscopy remain the same. If these—namely correct head position and adequate anaesthesia—are ignored, no laryngoscope will give success. The secret of successful intubation lies with the anaesthetist, not with any particular laryngoscope. That good result can be obtained with many different patterns is obvious from the fact that these different types all have their own supporters”.
Tracheal intubation facilitates various types of respiratory therapy, including mechanical ventilation, 100% O 2 for CO poisoning, NO, surfactant, Heliox, and suctioning.
The risks of tracheal intubation are heightened when airway management is required away from the OR and when multiple tracheal intubation attempts are made.
The limiting factors for the safe application of tracheal intubation are the skill of the practitioner, the use of patient monitoring, and an understanding of the indications for tracheal intubation.
Tracheal intubation (TI) is the placement of an endotracheal tube (ETT) into the trachea as a conduit for ventilation or other lung therapy. The benefits of TI are listed in Box 20.1 . Historically, tracheal ventilation arose as a means of resuscitation via a tracheostomy and progressed with the development of the ETT, which protected of the lungs from aspiration. The eventual discovery of inhalation anesthesia facilitated surgical applications requiring a secure airway, controlled ventilation, and lung therapy. This chapter will review these primary indications for TI in the context of resuscitation, prehospital airway management, emergency medicine, intensive care, and anesthesiology. Nontechnical and technical aspects of TI will then be considered.
A patent airway via oral, nasal, or tracheal routes
Controlled ventilation with up to 100% oxygen
Ventilation with high airway pressure
Airway protection from aspiration
Removal of secretions
Lung isolation
Administration of medication including anesthetic gases
Records of TI date back more than a thousand years to when early experiments were conducted by a Persian physician, Avicenna, who intubated pigs. In 1543, Andreas Vesalius, a Belgian anatomist, performed TI by inserting a cane tube through a tracheostomy into the trachea of a pig. These landmark developments allowed controlled ventilation and laid the foundation for subsequent advances in resuscitation. TI for human resuscitation was first performed in 1754 by an English surgeon, Benjamin Pugh, who orally intubated an asphyxiated neonate with his “air pipe.” This was followed in 1788 by Charles Kite, another English surgeon, who reported the use of his curved metal cannula that he introduced blindly into the trachea of several near-drowning victims from the river Thames.
TI is still considered to be the “gold standard” to maintain an airway and provide ventilation in most critically ill patients, but more recent evidence has called into question its prioritization during cardiopulmonary resuscitation (CPR), particularly in the out-of hospital (OH) setting. Previous observational literature involving large patient populations was limited by confounding factors where the airway procedure decision could not be controlled for. Two large prospective randomized trials comparing TI to supraglottic airway (SGA) placement in OH cardiac arrest and one comparing bag-mask ventilation (BMV) to TI favored a less invasive airway approach. Physiologically these findings have been explained by the importance of circulating oxygenated blood with uninterrupted high-quality chest compressions to increase coronary perfusion pressure and prioritizing defibrillation for shockable rhythms. This circulation first (“CAB” instead of “ABC”) approach emphasizes airway support interventions that are less likely to require any interruption to CPR. This approach is supported in part by literature demonstrating that patients with shockable rhythms managed without an advanced airway (MV) have had better outcomes than those managed with TI. Vigorous, often inadvertent positive-pressure ventilation (PPV) with high rates, pressures, and volumes associated with TI may have negative impact on cardiac arrest patients. Finally, it may be that the technical imperative of performing TI may be distracting from the other priorities in resuscitating a cardiac arrest victim.
Some have questioned the findings from these prospective studies on the basis of the low success rates for TI performed by nonphysician clinicians (paramedics). A recent large German registry dataset compared TI to SGA placement with physician providers using a matched analysis to address known confounders. The study demonstrated improved outcomes with TI during OH cardiac arrest. Additionally, just as less invasive airway management may be better suited for shockable rhythm cardiac arrests where early return of spontaneous circulation is more likely, there is evidence that for nonshockable rhythms a more advanced airway management such as TI is associated with improved outcomes. In a 2019 American Heart Association Focused Update on Advanced Cardiac Life Support, provider experience and training were addressed in the recommendations.
Early intubation for trauma patients in the prehospital setting has yielded mixed results, but for patients with severe injuries managed by skilled emergency medical service (EMS) providers, there appears to be a mortality benefit. , Much of the literature surrounding airway management for trauma has focused on care of patients with traumatic brain injury (TBI), whether in isolation or as part of a multisystem injury presentation. The most common reason to intubate patients with isolated TBI is for airway protection and/or predicted course (anticipated clinical deterioration). Given the fact that any hypocapnia, hypoxemia, or hypotension is associated with worse outcomes in this patient population, the risks of performing TI early, particularly in a less controlled environment, must be balanced against the benefits of securing the airway. The motto of “GCS [Glasgow Coma Scale] less than 8, intubate” is essentially invalidated and much too superficial to be used as decision guidance for a patient with TBI. Skilled provision of prehospital intubation for patients with TBI decreases mortality. This requires care, preparation, and performance of TI to avoid any physiologic derangements. , Avoiding hypoxemia, hypocapnia, and hypotension, and early access to imaging and neurosurgical care are the priorities for managing these patients. While early airway, oxygenation, and hemodynamic support for trauma may be needed, this does not necessarily mean prioritizing early intubation.
Resuscitation Sequenced Intubation for managing critically ill patients and the physiologically difficult airway has become an accepted term describing at-risk cohorts where the process of intubation and transition to PPV poses significant risk to the patient. The Society for Airway Management recently published consensus recommendations on the Evaluation and Management of the Physiologically Difficult Airway.
The best airway technique for resuscitation depends on the patient’s needs and clinical circumstances, the availability of appropriate equipment, and the skill of the rescuer. , Solutions to these problems involve training in airway management, appropriate selection of airway devices, and patient monitoring. Waveform capnography can supplement clinical assessment of tracheal tube placement during CPR and is the most specific and sensitive method of confirming and monitoring tracheal tube placement during CPR. However, it cannot reliably differentiate tracheal and endobronchial tube placement.
TI for resuscitation of the newborn is indicated if BMV has been prolonged or is ineffective, if chest compressions are to administer tracheal surfactant, or to manage a neonate with a congenital airway anomaly such as congenital diaphragmatic hernia or severe micrognathia. TI may also be indicated for tracheal obstruction as a result of neonatal meconium aspiration; however, routine intubation and suctioning of vigorous infants born through meconium liquor are not recommended. , Care and experience are required to avoid trauma and esophageal intubation.
Emergency TI in the prehospital environment often occurs in unfavorable conditions on patients who can be critically ill with shock, cardiopulmonary arrest, multisystem trauma, TBI, airway trauma, or uncorrected respiratory failure. The benefit of prehospital intubation (PHI) remains controversial. Conflicting results and opinions in part are related to differences in prehospital provider team makeup. , , Outside North America, many prehospital systems use physician-only teams or a team of physician and nonphysician, usually a paramedic or nurse. Most physician prehospital programs are staffed by anesthesiologists and, to a lesser extent, emergency physicians. However, even within nonphysician-staffed prehospital programs, there is considerable variability in team makeup, using some combination of paramedics, nurses, and, in some jurisdictions, respiratory therapists. Most air transport services, in particular helicopter emergency medical services (HEMS), are staffed by specially trained critical care transport personnel consisting of either paramedics, nurses, physicians, or some combination thereof.
The natural history of most survivable illness or injury will be altered based on access to a high level of competent care. Most prehospital systems still consider TI the most definitive form of airway management; however, decision-making in the prehospital environment requires a risk-benefit analysis that must consider clinician skills, equipment access, availability of clinical practice guideline (CPG) support, and other resources, as well as the impact of transport delay. In most ground-based EMS systems in North America, direct laryngoscopy (DL) and intubation are within the scope of practice for a segment of advanced care paramedics; however, performance differences among agencies are quite variable. The decision to perform TI by EMS systems must be supported by training and ongoing experience. ,
While paramedics may be provided with excellent educational and simulation programming, access to operating room and emergency department educational opportunities on patients is increasingly difficult. , Rates of prehospital intubation are low at 5 to 8 per 1000. EMS calls resulting in many providers performing one or no intubations per year in part explain the low overall success rates in many programs. Additional procedural, equipment, and situational factors, such as having access only to non-RSI drugs, no access to video-assisted laryngoscopy (VAL), limited use of capnography, and the need to perform intubation in a difficult, often austere environment, play a significant role in determining airway management outcomes in the prehospital setting. Many European and Nordic countries use physicians as prehospital providers and have published results demonstrating significantly higher median first-pass intubation success rates for physicians compared to nonphysicians.
The 2016 Scandinavian Society of Anesthesiology and Intensive Care Medicine prehospital airway management guidelines and the more recent publication by the European HEMS & Air Ambulance Committee (EHAC) Medical Working Group on prehospital airway anesthesia are currently the only guidelines that include training recommendations for EMS providers. , The expectations of these primarily physician-based systems are that prehospital airway-management performance outcomes should be similar to those achieved in a hospital-based critical care environment (emergency department [ED], intensive care unit [ICU]). The authors of these publications work in regions where prehospital airway management is largely provided by physicians, and therefore expectations are high that care standards in the prehospital setting should be equivalent to that provided in a hospital with highly trained emergency/anesthesiology staff. While this may seem a reasonable expectation, existing staffing, logistical, and other system differences around the world make this goal difficult to achieve.
Prehospital care outcomes for critically ill patients are usually time dependent. Delivering prehospital care and airway management to critically ill patients, and then retrieving the patient for hospital care are both time-dependent phases of therapy. This time dependency may be related to both the outgoing and the incoming legs of the transport. The goal of resuscitation is to ensure adequate gas exchange and maintain end-organ perfusion. The technical imperative to get the tube in may not be a patient-centered approach, as an ETT simply provides a conduit for the primary airway management goal of improving and maintaining oxygenation and ventilation. Decisions around what can be done and what should be done in the prehospital setting will depend on the patient, the illness or injury, system factors (provider skill, scope of practice, equipment access), and geography that influences time to help and time to definitive care.
Management of the airway in the ED is often a fine balance between urgency and risk. Like the prehospital setting, there are notable differences in who provides/supports airway management in EDs in various regions around the world. Emergency medicine is a relatively new but established specialty for which clinicians must balance disease prevalence , life-threatening acuity , and complexity in systems-based care. Airway management is a necessary, core skill for the specialty, and while the hands-on daily opportunities cannot be compared to those of anesthesiologists, existing registry data support this practice. In a systematic review of over 40,000 intubations from 10 countries over a 15-year period, the reported first-pass success (FPS) rate for ED intubations was 84%. The FPS concept has been challenged from a patient-outcome perspective. It has been demonstrated that as the number of ED intubation attempts increase, so does the incidence of adverse events. More recent data from the National Emergency Airway Registry (NEAR) have demonstrated improving FPS rates in the ED of over 90%. In a recent prospective randomized ED trial by Driver et al. comparing routine use of a bougie with a stylet/ETT combination, FPS in the routine bougie group was 98%. While routine use of the bougie clearly demonstrated benefit in this trial, these patients were managed by an experienced group of EPs performing RSIs using video-assisted DL and who were quite experienced with this approach. It has been suggested that improving results, such as those demonstrated in the Driver et al. study, may be less about the equipment and more about the bundle of optimized airway management care that delivered these high success rates. While some have questioned the benefit of routine use of bundled care and checklists for airway management, there is a growing body of literature supporting their use in the ED. ,
In the Fourth National Audit Project (NAP4) of the Royal College of Anaesthetists (UK) and the Difficult Airway Society (DAS), major airway management complications occurred significantly more often in the ED and ICU compared to the OR. For numerous reasons, airway management of critically ill patients, regardless of location, will be associated with more adverse events compared to the more controlled elective environment of the operating room. The term difficult airway (DA) has traditionally referred to anatomic and pathologic challenges surrounding face mask and supraglottic ventilation, laryngoscopy and intubation, and front of neck airway (cricothyrotomy). The incidence of difficulty defined as such in the ED is notably higher than what is reported in the OR. Other factors, however, play a major role in determining ED airway outcome, most important of which is to manage the physiologically difficult airway. , , The physiologically difficult airway encompasses a range of homeostatic disorders including but not limited to hypoxemia, shock, and metabolic acidosis, all of which often occur together in critically ill ED patients. Despite the fact that RSI is by far the most commonly performed procedure in EDs around the world and has no doubt been contributory to high FPS rates, the downstream potential morbidity and mortality costs have raised questions about the benefit of RSI for patients in whom physiologic compromise cannot be optimized. , , Emergent intubation may be indicated to ensure safe/good outcomes; however, meticulous attention must be paid to identifying and resuscitating these patients in the periintubation period. Performing an RSI might provide optimal laryngoscopy conditions for the provider, but loss of spontaneous ventilation may pose a significant risk in many critically ill patients. The challenge is that the traditional alternative to an RSI—the awake intubation (AI)—frequently will be limited by the patient’s limited ability to cooperate and by provider experience. Delayed Sequence Intubation (DSI) is a term that refers to pharmacologically facilitated periintubation resuscitation efforts prior to intubation. While it may suggest that an RSI will follow, this intervention may be a helpful bridge to help facilitate an awake approach with topical anesthesia using the technique of preference for the user (DL, VL, or Flexible scope intubation). And so the term difficult airway in the ED takes on an expanded definition beyond that described by the patient’s native anatomy or acquired pathology in the ED to include the patient’s physiology and ability to cooperate with an awake technique. Contrary to popular belief, the need to immediately manage an airway in the ED is relatively uncommon. Rapid, safe ED airway management requires skillful execution of laryngoscopy and intubation using a narrow range of devices in a resuscitated patient—a scope of practice that is well within the discipline of emergency medicine.
The most common indications for TI in the ICU are acute respiratory failure, shock, and neurologic disorders. TI is indicated for controlled ventilation in the presence of refractory hypoxemia, often in the presence of multiple organ failure. Predictors of hypoxemic respiratory failure are listed in Box 20.2.
No or minimal rise in the ratio of P a o 2 to F io 2 after 1 to 2 hours
Patients older than 40 years
High-acuity illness at admission (simplified acute physiology score >35) 170
Presence of ARDS (acute respiratory distress syndrome)
Community-acquired pneumonia with or without sepsis
Multiorgan failure
The decision to intubate is usually made on clinical grounds based on the prognosis for the patient’s condition. Clinical signs (see Box 20.3 ) or evolving deterioration in objective criteria may support this decision.
1.Look of anxietyFrowning2.Signs of sympathetic overactivityDilated pupils, forehead sweat3.DyspneaDecreased talking4.Use of accessory musclesHolds head off pillow5.Mouth opens during inspirationLicking of dry lips6.Self-PEEPPursed lips, expiratory grunting, groaning7.Cyanosed lips8.Restlessness and fidgeting9.Apathy and coma
PEEP , Positive end-expiratory pressure.
Urgent intubation in the ICU may be required immediately for apnea, airway obstruction, reintubation, or cardiopulmonary arrest. If the patient is unconscious, without airway reflexes, or paralyzed, TI can proceed without pharmacologic support.
RSI, the gold standard technique commonly used in the ED, may not be as applicable for the unstable ICU patient. Preoxygenation of the patient with limited respiratory reserve is compromised by decreased functional residual capacity (FRC) and increased dead space. Commonly used induction agents can adversely affect the unstable patient. In these situations, a non-RSI technique with sedation and local anesthetic might be used.
Noninvasive ventilation techniques have become increasingly popular over the past 20 years with clear indications and a range of masks and interfaces. Indications include patients with cardiogenic pulmonary edema and exacerbations of chronic obstructive pulmonary disease (COPD). Noninvasive ventilation is contraindicated for respiratory arrest or patients who are unable to be mask ventilated. Relative contraindications for noninvasive ventilation that favor TI are listed in Box 20.4 .
Medically unstable
Agitated and uncooperative
Unable to protect the airway
Impaired swallow
Excessive secretions that are not being adequately managed
Multiple organ failure (i.e., two or more)
Recent upper airway or upper gastrointestinal surgery
Failed noninvasive ventilation
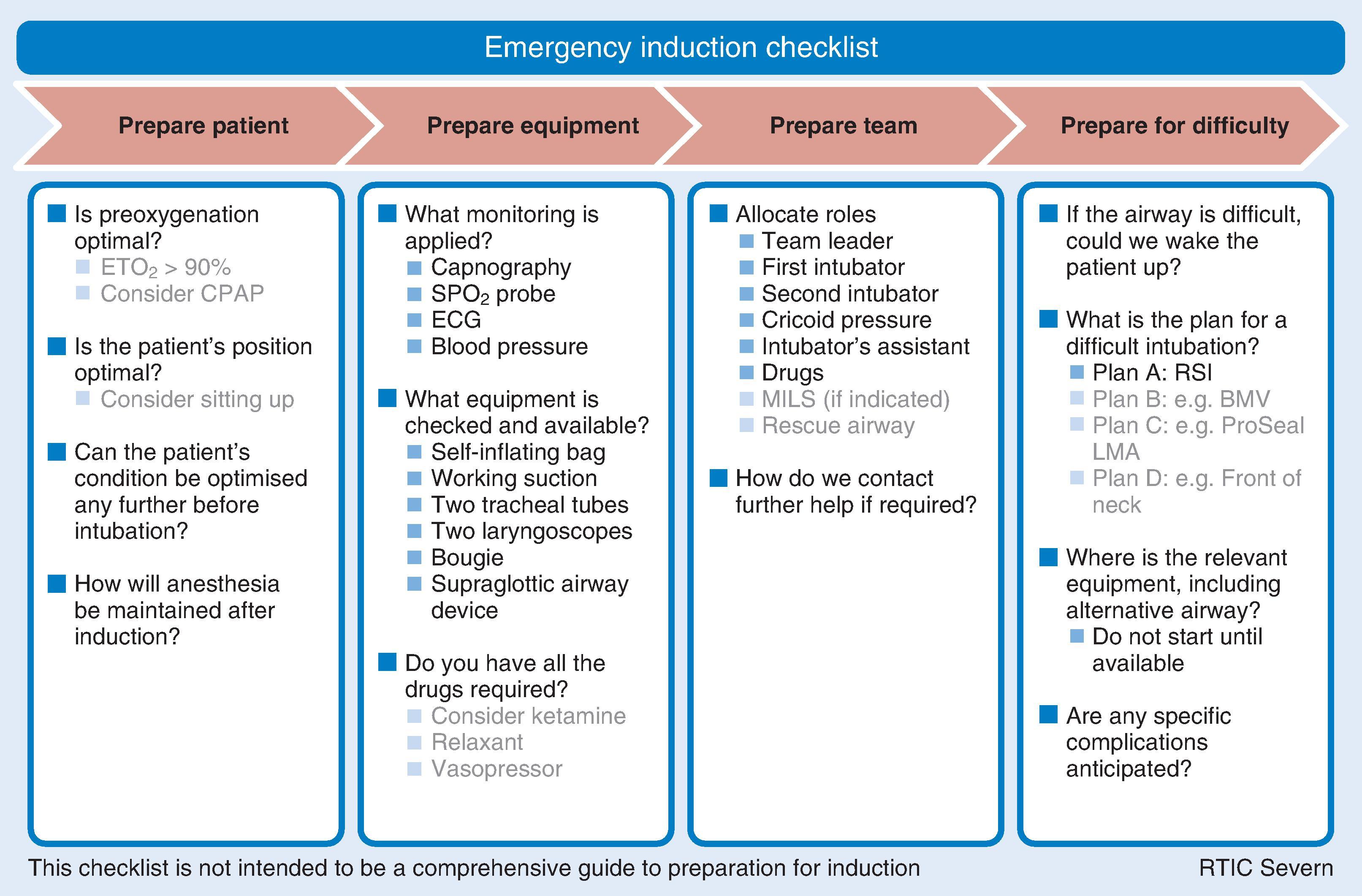
In the NAP4 of the Royal College of Anaesthetists and the Difficult Airway Society (DAS), 184 patients suffered major complications from airway management (death, brain damage, emergency surgical airway, unanticipated ICU admission, and prolonged ICU stay). Of that number, 36 occurred in the ICU. Although less than 20% of the total number of reported cases occurred in the ICU, more than 60% of the ICU cases resulted in death or brain damage compared with 14% in anesthesia. Assessors found a lower standard of airway management in the ICU than in both anesthesia and emergency medicine. The authors recommended the use of an intubation checklist to help prepare the patient, equipment, drugs, and the team before TI. An example of such a checklist appears in Fig. 20.1 . The use of capnography for intubation in all critically ill patients was also recommended. The incidence of airway mishaps in the ICU involving TI is relatively low. In a study of 5046 ICU intubated patients, the airway accident rate was 0.7%. Accidents were less common with ETTs than with tracheostomies. Self-extubation is the most common ETT accident, with rates of up to 16%. With strict clinical monitoring and in-service education this rate can reduce to 0.3%. Following unplanned extubation, reintubation rates ranged from 14% to 65%. In a prospective multicenter cohort observational study, the incidence of difficult intubation for obese patients in the ICU was found to be twice as high as a cohort of obese patients intubated in the OR (16.3% vs 8.2%, p < 0.01), and severe life-threatening complications related to intubation occurred 20 times more often in the ICU. A standard program of ETT management, including effective fixation techniques, can reduce unplanned extubation rates.
In addition to mechanical ventilation, TI facilitates other types of respiratory therapies. Patients with moderate to severe carbon monoxide poisoning can benefit from 100% oxygen. This concentration of oxygen in normobaric conditions is most reliably achieved through an ETT. Other therapy through an ETT includes synthetic surfactant for premature newborns with established respiratory distress syndrome (RDS). Nitric oxide (NO) is administered to adults, infants, and neonates receiving mechanical ventilation to treat acute lung injury, acute respiratory distress syndrome (ARDS), and RDS. Heliox is a blend of oxygen and helium gas used to improve gas flow to patients with airway narrowing such as in asthma. On the other hand, use of the ETT as a route for emergency drug administration during CPR is no longer recommended because of unpredictable plasma concentrations and the reliability of the intraosseous route.
Clearing secretions by suctioning through the ETT is important to maintain ventilation by avoiding atelectasis and consolidation. Suctioning is associated with several complications such as hypoxemia, cardiovascular instability, elevated intracranial pressure, atelectasis, infection, and trauma to the airway. Evidence-based recommendations for tracheal suctioning of adult intubated intensive-care patients are listed in Box 20.5 .
Suction no longer than 15 seconds.
Perform continuous rather than intermittent suctioning.
Avoid saline lavage.
Provide hyperoxygenation before and after suctioning.
Provide hyperinflation combined with hyperoxygenation routinely.
Always use an aseptic technique.
Use either closed or open suction systems.
It is reasonable to expect that with advances in device technology and updated practice guidelines, combined with progress in medical education techniques, outcomes from management of the difficult or failed intubation should improve over time. Unfortunately, the results from the latest 2000 to 2012 Anesthesia Closed Claims Project database do not demonstrate that the severity of claims against anesthesiologists were reduced. It was found that patients were more sick than in the previous survey in 1993 to 1999, more difficult TI occurred in nonperioperative locations, there were a higher proportion of deaths than in the previous survey, and a delay occurred in over one-third of patients requiring an emergency surgical airway. There is still an obvious need to improve procedural skill and the response to TI in anesthesia. Conversely, there is some evidence that difficulty with TI may have decreased over time.
Significant improvements to the design of the ETT have been historically precipitated by evolving surgical techniques. Upper airway surgery performed in the early 19th century led to an increase in postoperative pneumonia caused by aspiration of surgical debris. In 1878, William Macewen first used an ETT in anesthesia for a patient with a tumor of the base of the tongue. Macewen was also concerned with preventing aspiration and in 1880 developed a metal ETT with a sponge collar that he introduced blindly through the mouth for TI. In 1888, O’Dwyer designed a curved metal cannula with a conical end to provide a laryngeal seal. This device helped raise intratracheal pressure to avoid pulmonary collapse during thoracic surgery. In 1895, Alfred Kirstein performed awake DL with the “autoscope.” This primitive instrument was the precursor of other laryngoscopes developed by Jackson and others, aiding the utilization of the ETT. World War I precipitated a demand for plastic surgery of the head and neck, which led to oral and nasal ETT designs with pharyngeal or tracheal cuffs by Rowbotham and Magill. Anesthetic management for thoracic surgery led to the next advance in ETT design with the introduction of the first endobronchial tubes in 1932 by Gale and Waters. By this time, the technique of TI was established, prompting the statement by Macintosh that “the ability to pass an ETT under direct vision was the hallmark of the successful anaesthetist.”
TI is now used extensively in modern anesthesia for elective and emergency indications both as a primary and rescue airway. Patient characteristics and surgical indications will often dictate the appropriateness of an ETT. Elective TI is indicated for patients requiring anesthesia for major surgery when controlled ventilation, resuscitation, airway access, patient positioning and duration of surgery are factors in the overall airway plan. Specialized ventilation tubes are used for specific indications. Examples include thoracic surgery requiring lung isolation, laryngeal surgery requiring microlaryngoscopy or laser treatment, and nasal intubation for limited mouth opening, oral surgery, and maxillofacial surgery. TI may occur when the primary surgical plan changes. An example is conversion of a diagnostic procedure, such as a bronchoscopy to a lung resection. Occasionally, complications arise during a simple anesthetic, necessitating TI during resuscitation, such as major hemorrhage, anaphylaxis, or malignant hyperthermia. Safe airway management should always include a plan B for failed mask or SGA ventilation. Conversion of the airway to TI may occur as plan B following inadequate mask or SGA ventilation. Impossible mask ventilation in anesthesia has an incidence of 0.15% and is associated with neck radiation changes, male gender, sleep apnea, Mallampati class III or IV, and the presence of a beard. In a study by Kheterpal of 53,041 operations that included an attempt at mask ventilation, 77 patients proved impossible to ventilate (0.15%). Of those 77 patients, 19 (25%) were also difficult to intubate, but 15 of those patients were intubated. Ultimately 74 of the 77 impossible mask ventilation cases were intubated, reinforcing the value of TI for failed ventilation.
The American Society of Anesthesiologists (ASA) “Practice Guidelines for Management of the Difficult Airway” recommends AI for the patient with a known DA. This usually involves TI with a flexible intubation scope (FIS), but other techniques have been described, including retrograde AI, submental AI, AI through an intubating laryngeal mask, awake lightwand, and awake videolaryngoscopy (VL). The outcome of each technique is a secure airway with an ETT.
TI is regarded as the gold standard for protection against aspiration of gastric contents in anesthetized patients ; however, evaluation of the cuff seal is important because of the risk of microaspiration of oropharyngeal contents past the cuff. This particularly applies to high-pressure low-volume cuffs. Evidence evaluating the relative risk of an ETT or SGA for pulmonary aspiration is limited. An analysis of the relative risk in 65,712 procedures found that the use of a laryngeal mask airway was not associated with an increased risk of pulmonary aspiration compared with an ETT.
Before undertaking the technical aspects of TI, consider why, where, how, when , and by whom airway management should be performed. Airway management practice guidelines offer useful advice to inform these decisions. , (See Chapter 11 concerning practice guidelines.) Serious morbidity and mortality can occur when important decisions are overlooked. Poor judgment was the second most common causal and contributory factor (59%) to that after patient factors (77%) in NAP4.
The NAP4 study found that difficult or delayed intubation, failed intubation, and cannot intubate, cannot ventilate (CICV) situations accounted for 39% of events during anesthesia, and CICV accounts for 25% of all anesthesia-related deaths. Obsession with intubation and ignoring other options, such as waking the patient up, has been a fixation error in many cases with adverse outcomes. Having a clear understanding of the indications for TI, devising an airway plan, establishing when and where to proceed, using the technique with the best chance of success, and assembling the necessary skill, equipment, and support are all important requirements for safe TI.
It is wise to spend time preparing for TI. The first attempt at TI has the highest success rate, and diminishing return occurs with each subsequent attempt. Limitations on the number of intubation attempts are recommended by all recent airway management guidelines. , Therefore, it makes sense to make your first attempt be your best attempt. This requires preemptive planning to intubate under optimal conditions.
Practice guidelines recommend the presence of a storage unit containing specialized equipment to manage a DA. , Details of the storage unit and equipment to manage a DA have been reviewed. It is recommended that equipment to manage an emergency airway should be immediately available at all sites where airways are managed. Safety principles for intubation equipment are based on standardization, redundancy, and a culture of safety. Avoid excessive clutter and unnecessary duplication in the airway cart (standardization). This principle promotes familiarization with equipment across an organization and aids teaching and learning. Redundancy ensures the safety of backup in the event of failure (e.g., spare laryngoscopes, a range of sizes, alternative designs such as Macintosh, Miller, McCoy, videolaryngoscope). A culture of safety includes education, checklists, updating of equipment, sterilization, and backup plans. Equipment must comply with performance standards and should be checked regularly to ensure that it is fit for purpose. A list of appropriate equipment for performing TI appears in Box 20.6 .
Oxygen (O 2 ) source
Ventilation bag or anesthesia circuit (for positive-pressure ventilation)
Appropriately sized face mask
Appropriately sized oropharyngeal and nasopharyngeal airways
Tongue blade
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here