Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Advances in endoscopic sinonasal surgical techniques and instrumentation have led to an expansion in the size and diversity of skull base lesions that are amenable to an entirely endoscopic resection. However, one of the requisites for successful removal of skull base lesions is the ability to repair the resultant defect, as failed reconstructions add significant morbidity.
The ideal endoscopic skull base repair has the following characteristics:
Technically feasible as part of an endoscopic procedure
Provides a reliable, robust, and long-term separation between the sinonasal and cranial cavities
Reconstructs the natural tissue barrier present in the anterior skull base
Minimally impacts normal sinonasal and cranial physiology
Obliterates dead space following tumor removal
Robust during adjuvant treatment
Flexible to accommodate skull base defects encountered immediately postresection
Skull base defects that are small in size, with low-flow intraoperative cerebrospinal fluid (CSF) leaks can be reconstructed with a wide variety of multilayered avascular free grafts or biosynthetic materials with high success rates and limited morbidity. However, free grafts have an unacceptably high risk of failure with larger defects for a number of reasons but primarily because the reconstructive bed is nonvascularized (i.e., air on one side and CSF on the other).
Larger skull base defects (>2–3 cm) and those that are associated with high-flow CSF leaks are best repaired with a multilayered closure technique using a vascularized flap. A high-flow leak is created when a CSF cistern is directly opened into the sinonasal cavity.
There is a wide variety of local and regional vascularized pedicle flaps that the surgeon can use to reconstruct skull base defects with the nasoseptal flap (NSF), first described in 2006, being the workhorse for endoscopic skull base repair.
When choosing the most appropriate reconstructive technique or flap, the surgeon needs to consider the anticipated location, size, and geometry of the bony and dural defects as well as high- versus low-flow CSF leak. Additionally, prior sinonasal surgery, previous or planned radiotherapy, and extent of tumor involvement may limit the available options and should be accounted for.
Endoscopic skull base reconstruction offers excellent success rates with low perioperative and postoperative morbidity. However, predictors of failure have not been entirely defined. There is evidence to suggest that radiotherapy, intraventricular tumor extension, and body habitus (predictive of increased intracranial pressure) may play a role in failed repairs whereas location and tumor histology seem less important. The most common points of failure of flap repairs are the dependent parts, presumably due to increased pressure, and the most superior parts due to the danger of flap migration or retraction.
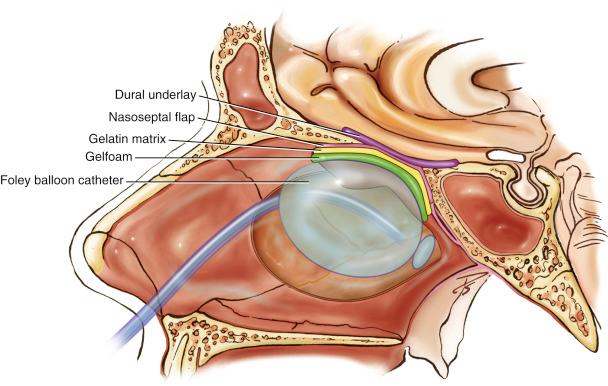
Both free and vascularized flap repairs use the theory of multilayered closure to provide a reliable barrier between the skull base and nasal cavity. Early CSF leak closure procedures included attempts at intracranial, but extradural, underlay reconstruction; this was subsequently found to be unnecessary. Underlay materials in multilayer reconstruction are placed subdurally. This forms the water-tight “bath plug” layer, and the pedicled flap is an onlay to provide vascularization.
The use of allografts has been associated with reasonably high rates of infection, and autologous bone/cartilage grafts have been associated with high rates of resorption.
The current philosophy at most major endoscopic skull base centers is to repair large, high-flow defects with one or more local vascularized flaps.
The focus of this chapter is on the posteriorly based NSF, as this is currently the mainstay of endoscopic skull base repair and adds very little sinonasal morbidity. Other methods of reconstruction in this chapter are described in the context of adjuncts or alternatives to the NSF when it is not available.
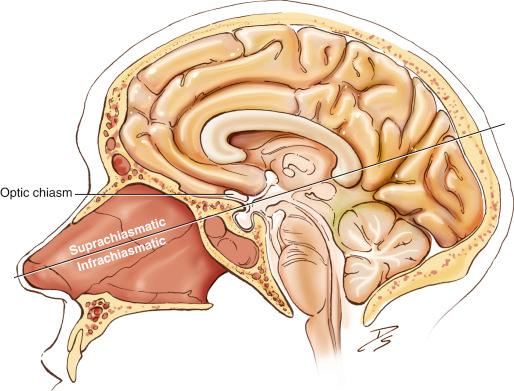
It is essential to assess the location of the lesion, to define which part of the skull base needs to be removed for access, and consequently what the extent of reconstruction is likely to be. These areas have been defined previously in relation to the sagittal or coronal extent of the lesion, as shown in Table 31.1 . However, much of this is academic, as it is the fixed neurovascular structures that determine the approach and resultant defect. The rule of “avoid crossing neurovascular planes” is equally true via an endoscopic route, as it is for open transcranial approaches. It is therefore important to define the lesion in the sagittal plane as either suprachiasmatic or infrachiasmatic ( Fig. 31.1 ). If the lesion extends lateral to the pterygoids in the coronal plane, the ipsilateral maxillary artery will likely be sacrificed. This will limit available pedicled flaps from the ipsilateral side (see Table 31.1 ).
| Sagittal Plane | Area | Coronal Plane | Flap Constraints |
|---|---|---|---|
| Transfrontal | 1 | Transorbital | Contralateral flap needed |
| Transcribriform | 2 | Petrous apex (medial transpetrous) | |
| Transplanum (suprasellar/subchiasmatic) Transsphenoidal (sellar/medial transcavernous) |
3 | Lateral transcavernous Transpterygoid Transpetrous (superior/inferior) |
|
| Transclival (posterior clinoid/midclivus/foramen magnum) Transodontoid |
4 | Transcondylar Parapharyngeal space |
Contralateral flap not needed |
Once the extent of skull base removal has been considered, an appropriate repair can be planned. Radiographic analysis shows that a pedicled NSF permits coverage of the entire anterior skull base area from the posterior table of the frontal sinus to the sella with a width from lamina papyracea to lamina papyracea or, alternatively, coverage of a full panclivectomy. An important clinical rule is that coverage of two contiguous skull base areas (e.g., sella and clivus, or cribriform plate and planum sphenoidale) is possible but not three. The units are clival, sella/planum, cribriform, and frontal (see Table 31.1 ).
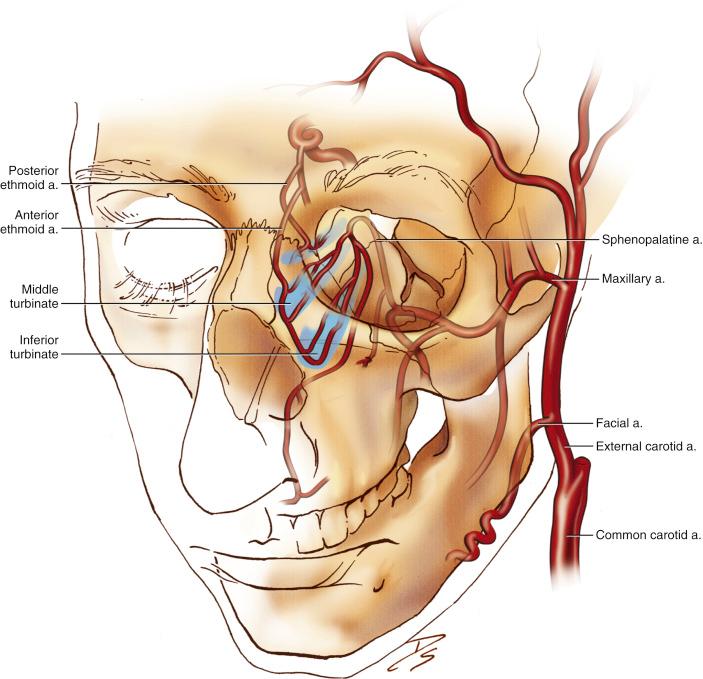
The rich arterial supply of the sinonasal cavity provides a variety of flaps for skull base reconstruction ( Fig. 31.2 ). Endonasal pedicled flaps with associated vasculature are listed in Table 31.2 . The maximum surface area of each flap is approximated and derived from existing literature.
| Flap | Type | Blood Supply | Midline Range of Coverage | Approximate Maximum Area (cm 2 ) | Comments |
| Local | |||||
| Nasoseptal | Local mucosal | Septal branch of sphenopalatine artery | Transcribriform to transclival | 25.1 | Mainstay of reconstruction, wide durable flap with long pedicle |
| Contralateral transposition septal | Local mucosal | Ethmoidal arteries | Transfrontal and transcribriform | NA. Likely similar to nasoseptal flap | Short pedicle, risk of persistent perforation |
| Inferior turbinate | Local mucosal | Inferior turbinate branch of sphenopalatine artery | Transplanum to transodontoid | 2.4 | Long and narrow flap, anterior reach limited |
| Nasal floor | Local mucosal | Branches of the sphenopalatine artery and the Woodruff plexus | Transplanum to transodontoid | NA | Technically challenging, short pedicle |
| Middle turbinate | Local mucosal | Middle turbinate branch of sphenopalatine artery | Transplanum to transsellar | 5.6 | Technically challenging, very variable dimensions depending on middle turbinate size |
| Hard palate mucosa | Regional mucosal | Descending palatine artery | Transplanum to transclival | 15.25 | Long pedicle, risk of oroantral fistula |
| Regional | |||||
| Pericranial (fascial) | Regional fascial | Supraorbital and supratrochlear arteries | Transfrontal to transclival | 293 | Requires Lothrop procedure to enable flap transposition |
| Temporoparietal (fascial) | Regional fascial | Anterior branch of superficial temporal artery | Transfrontal to transodontoid | 238 | Large area, takes time to raise, danger to frontal branch of facial nerve |
| Facial buccinator | Regional myomucosal | Buccal branch of facial artery | Transcribriform to transplanum | 18.75 | Risk of epiphora |
Obtain a detailed history of previous nasal procedures. Prior resection of bone and/or cartilage from the nasal septum or turbinates may make flap harvest more challenging. Prior sphenoid surgery may have compromised the septal branch of the sphenopalatine artery; earlier turbinate surgery may also influence flap options.
Carefully note previous systemic or intranasal treatments, especially chemoradiotherapy, which may affect postoperative healing. Consider whether postoperative radiotherapy is likely to be needed, as this will affect the choice of repair.
Undertake a detailed endoscopic examination of the patient’s nasal cavity and note any of the following:
Evidence of any previous sinonasal surgery, particularly a wide sphenoidotomy
Loss of turbinate or septal tissue
The presence, location, and extent of any septal deviation
If there has been previous sinonasal surgery, conduct a pedicle assessment, as provided in Table 31.3 .
| Pedicle | May Be Unavailable Due To | Flaps Excluded If Injured | Flap Alternative |
|---|---|---|---|
| Septal branch of sphenopalatine artery | Extensive tumor involvement Sphenoid surgery Posterior septectomy Tumor/surgery in pteryopalatine fossa Sphenopalatine artery ligation |
Posterior septal flap | Contralateral nasoseptal flap Regional flap Turbinate flap for small or posterior cranial fossa defects |
| Inferior turbinate branch of sphenopalatine artery | Inferior turbinate surgery/tumor Sphenopalatine artery ligation |
Inferior turbinate flap | Contralateral nasoseptal flap Regional flap |
| Descending palatine branch | Surgery/tumor in pterygopalatine fossa Surgery/tumor in infratemporal fossa Cleft palate |
Palatal flap | Regional flap |
| Internal maxillary artery | Surgery/tumor in infratemporal fossa | Posterior septal flap Inferior turbinate flap Nasal floor flap Middle turbinate flap |
Contralateral nasoseptal flap Regional flap |
Check that endoscopic visualization of the potential defect is going to be possible; this is imperative to permit full closure. It will be necessary to perform a modified endoscopic Lothrop procedure (MELP) if complete resection of the anterior skull base is required.
The general preoperative health status of the patient is important to consider since comorbid diseases may complicate the patient’s recovery. For example, increased body habitus may be associated with increased CSF pressure and obstructive sleep apnea may be more challenging to manage without the use of positive pressure ventilation.
Note the potential geometry of the skull base defect that will result after resection. Angles of the skull base surface make placing a graft more difficult and require longer flaps to achieve full coverage and closure. Asian nasal cavities may not have the equivalent septal mucosal flap area available for harvest as compared to the noses of whites.
Lesions that may involve repair of the posterior table of the frontal sinus will require a MELP, and lateral frontal sinus floor repair beyond the midpoint of the orbit will require an external approach or orbital transposition.
In younger patients being considered for nasoseptal flap repair, assess the cranium-to-face ratio to ensure that the nasoseptal flap will cover the defect created. The pedicled nasoseptal flap may not be a reliable option for patients under 14 years old.
If a middle turbinate flap is being considered, note the anatomy and size of the middle turbinate. At least 4 cm middle turbinate length is required for the flap to reach the sella.
Note whether the arachnoid cisterns, or occasionally ventricles, are likely to be opened. This may influence the need for vascularized repair regardless of the dural defect size, as a high-flow CSF leak will be created.
0-degree nasal endoscope
Monopolar needle-tip electrocautery with the tip bent at 45 degrees provides accurate flap incisions with good hemostasis.
Bipolar electrocautery for accurate control of troublesome hemorrhage
Blunt dissection instruments, such as a Cottle elevator, for raising the flap over a wide plane
FESS micro-scissors for fine adjustment of the flap dimensions
Ball-tip probe for fine nontraumatic manipulation of the flap
Small curette for fine nontraumatic manipulation of the flap
Curved olive-tip suction without suction attached for placing the underlay graft material and manipulating the flap
Straight and angled cutting forceps (large and small) for fine adjustment of the flap dimensions
Straight and angled grabbing forceps for fine flap adjustment
Materials
Underlay graft
Artifical dura mater substitutes: DuraGen, TissuDura, DuraMatrix
Autologous option: Fascia (usually tensor fascia lata) and fat (abdominal or left inguinal)
Silastic sheeting for coverage of mucosal donor sites and exposed bone
Gelfoam dissolvable packing, which helps to support and hold the graft or flap in place
Surgiflo gelatin hemostatic matrix
NasoPore dissolvable packing, which is more easily removed postoperatively
Foley balloon catheter (16 g, 30 mL) for support of dissolvable dressings
Raising any pedicled flap should occur early in the procedure. This helps to ensure that the vascular supply to the flap remains intact and provides for a speedy reconstruction once the lesion has been removed.
Any pedicled mucosal flap used should be “oversized” for the defect concerned, as flap length is lost in contouring the flap to the skull base defect. More length is needed for a defect involving skull base angles, and many nasal flaps may need to be raised as far anteriorly as the mucocutaneous junction. Additionally, making sure that the pedicle is raised will allow for more mobility and greater coverage.
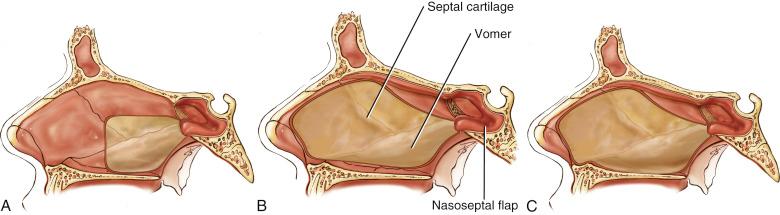
There are only three versions of NSF harvest currently in use ( Fig. 31.3 ). If the defect is sella and planum only, the flap is raised to the level of the middle turbinate head. The posterior septum and contralateral mucosa are sacrificed. If further coverage of ethmoid, clivus, or rostral skull base is required, the full mucoperiosteum is removed and the contralateral mucosa is brought forward to cover the ipsilateral septal donor site. If more surface area is required, the nasal floor is included in the flap.
The flap pedicle may itself cause functional problems in the nose, and it may be necessary to skeletonize the pedicle fully to ensure minimal mucosal trapping postoperatively. If problems still occur, it may be possible to divide the pedicle, although this is inadvisable less than 6 months after the repair has taken place.
Constant awareness of the location of the flap must be maintained throughout the procedure to avoid injury to the vascular pedicle. The flap should be stored in the ipsilateral maxillary sinus or nasopharynx for protection during the resection. Gelfoam may be placed on the exposed periosteum of the pedicle as further protection. If suctioning is required during the placement of the grafts, the use of a neurosurgical patty will avoid displacement of the grafts.
Special intracranial extradural layers are unnecessary and add nothing to the security of the repair. Underlay materials in a multilayer reconstruction are subdural. This forms the water-tight “bath plug” layer, and the mucosal flap is an onlay flap to provide vascularization ( Fig. 31.4 ).
Avoid burying functional mucosa under any graft or flap to prevent mucocele formation.
If the vascularized flap does not cover the entire defect, free mucosal grafts can be used to supplement coverage. It is important to place the vascularized graft at the site that is most likely to leak, such as the most dependent aspect, and the center of the defect where there is no vascular supply.
Tight packing at the end of the procedure should be avoided to maintain the vascular supply to any pedicled graft.
When placing the Foley catheter, it is important to recognize that its role is to support and stabilize the absorbable packing rather than to hold up the grafts. Therefore, do not overfill the balloon, as this may inadvertently cause a CSF leak by displacing the grafts intracranially.
Securing the Foley catheter is an important step in the operation. It must be secure enough that it will not become displaced posteriorly and cause inadvertent airway obstruction. However, it is imperative to not secure it in a manner that puts pressure on the nasal ala, which will lead to necrosis and subsequent notching.
The routine use of perioperative lumbar drains is not supported and may cause unnecessary morbidity. CSF diversion may be considered in selected instances, such as when there is suspected or known intracranial hypertension or in the management of small, early postoperative CSF leaks.
Preoperatively, decide on the preferred flap design to be used for repair of the skull base defect.
A mixture of 1% ropivacaine with 1:100,000 epinephrine is infiltrated into the area in which the flap will be raised. Topical 1:2000 epinephrine is used for hemostasis throughout the case.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here