Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
The first reported case of laparoscopic duodenal atresia repair was in 2001 by Bax et al and was followed by the first significant series in 2002 by Rothenberg. Since then, the operation has become much more common, although the majority of these operations are still performed via a laparotomy. This may be because of the small working space in the neonatal abdomen, the technical difficulty of performing the anastomosis laparoscopically, and the fact that many of these children have associated congenital (including cardiac) abnormalities. The metabolic, ventilatory, and hemodynamic consequences of CO 2 insufflation can be concerning for the operative team. When the child has incomplete duodenal obstruction, as is the case in duodenal stenosis, the patient may present later in life, making laparoscopic correction easier as the abdominal working space is larger. Moreover, there is less discrepancy between the diameter of the lumen of the proximal and distal duodenum. This chapter discusses the laparoscopic correction of duodenal atresia, duodenal web, and duodenal stenosis.
The diagnosis of complete duodenal obstruction is easy. There is usually polyhydramnios, and the dilated stomach and the dilated proximal duodenum are easily seen antenatally on ultrasound or postnatally on a plain abdominal radiograph, which shows the classic double bubble sign ( Fig. 6-1 ). If the proximal duodenum is not markedly dilated and air is seen distally, malrotation with volvulus should be immediately excluded by an upper gastrointestinal contrast study. Duodenal atresia and intestinal malrotation can coexist, and a high proportion of patients with intrinsic duodenal lesions have trisomy 21. Also, concomitant congenital abnormalities should be sought.

Before taking the child to the operating room, any electrolyte or acid–base disturbances should be corrected. In most cases, a single dose of a first-generation cephalosporin should be administered.
General anesthesia, in combination with local analgesia, is employed. A nasogastric (NG) tube is introduced to decompress the stomach and proximal dilated duodenum.
The child is placed at the lower end of the operating table so the surgeon can stand between the patient’s legs. Most infants can simply have their legs spread slightly or positioned in a frog-leg position if the surgeon prefers. The surgeon stands at the end of the table, slightly to the right, as the operation is triangulated to the patient’s right upper quadrant. The camera person can be on the surgeon’s left or right, depending on surgeon preference, with the scrub nurse on the other side. The main monitor should be situated just over the patient’s right shoulder ( Fig. 6-2A ). A second monitor can be placed on the right for the assistant to see.
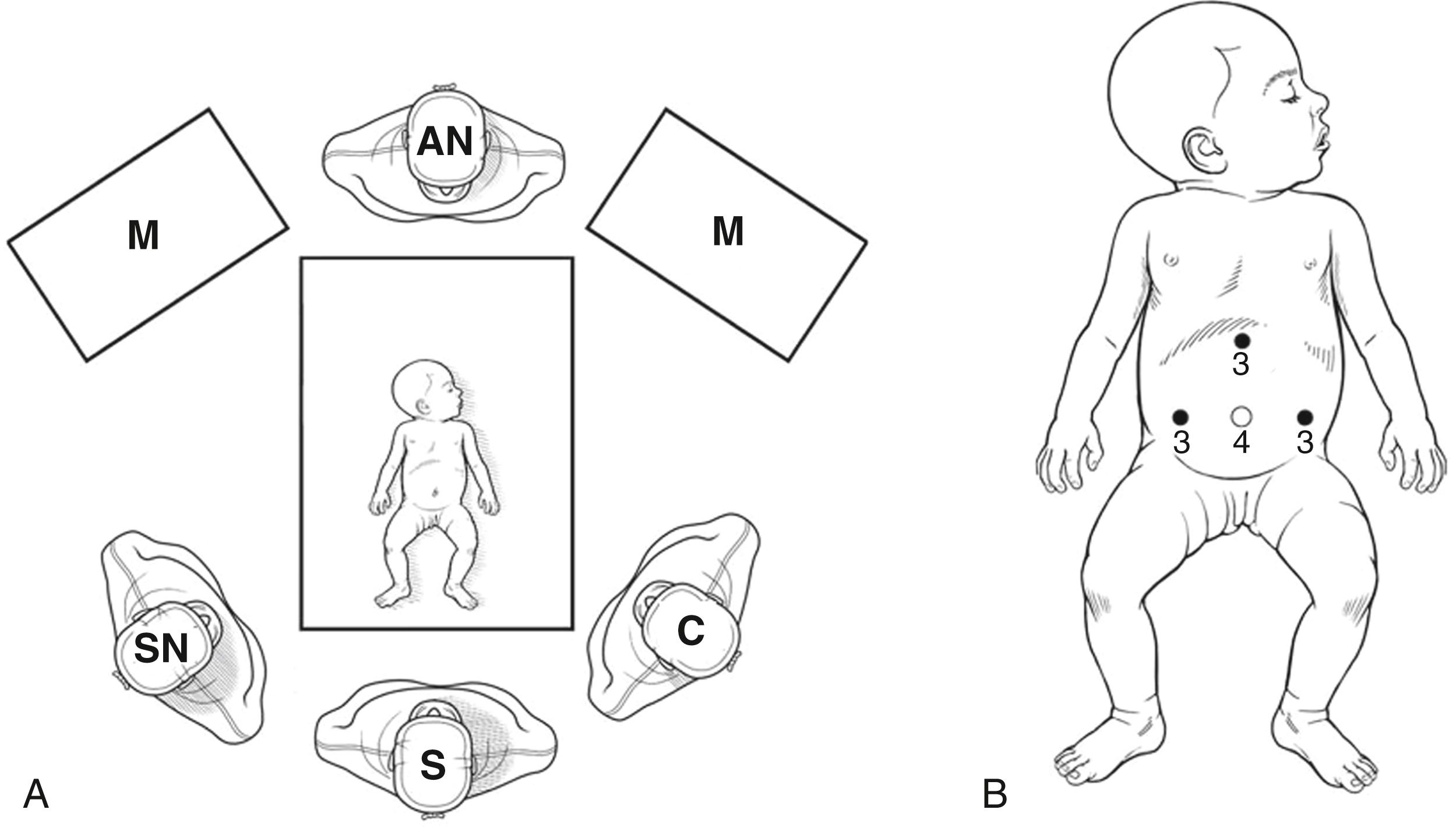
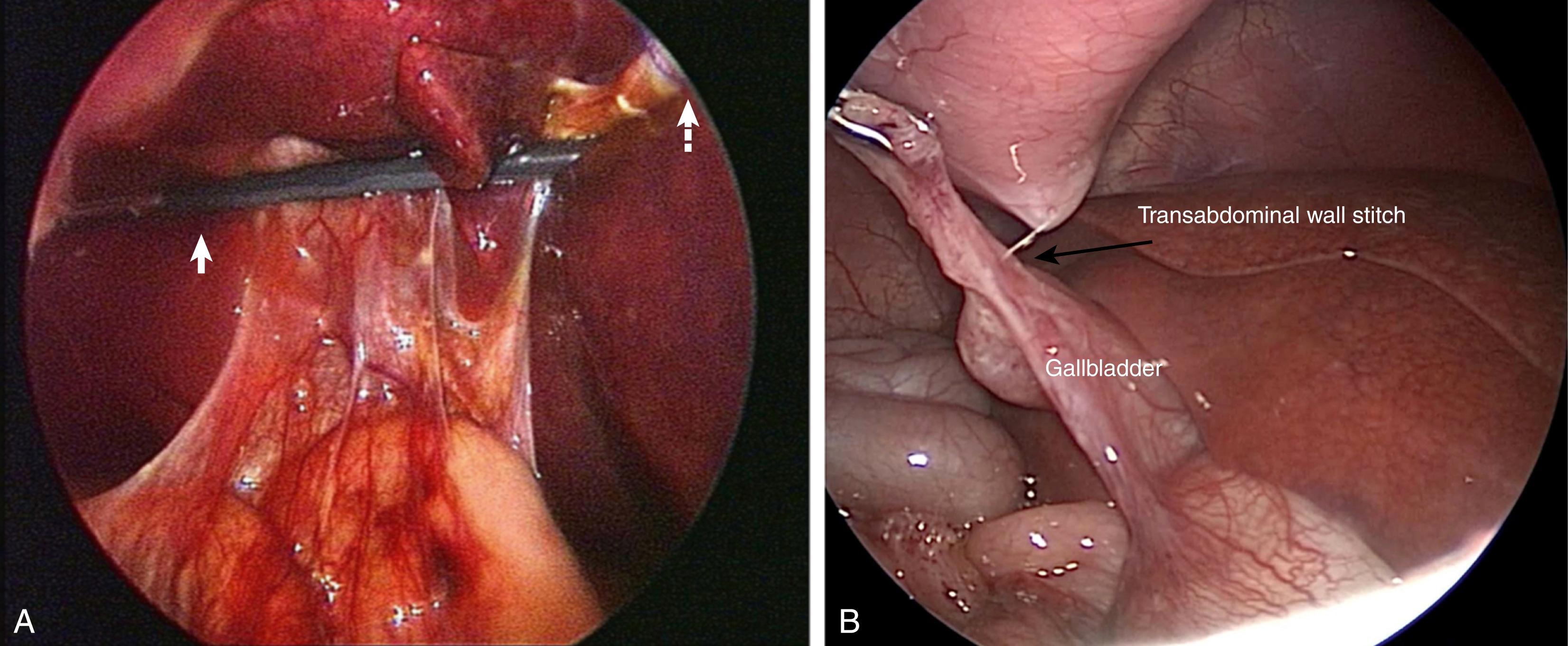
The procedure is usually performed using three ports. However, a fourth port for retraction can be added if necessary. The camera port is placed through an infra-umbilical ring incision to avoid the umbilical vessels (see Chapter 1 for additional information). The abdomen can be inflated by a Veress needle or Hassan technique depending on surgeon preference. A 4-mm cannula is inserted and a short (20-cm) 4-mm, 30-degree telescope is used. This gives an excellent wide-angle view of the right upper abdomen. In larger patients, a 5-mm telescope can be used. A 3-mm port is inserted in the patient’s left midabdomen, just above the umbilicus, for the surgeon’s right hand and a 3-mm port or simply a 3-mm stab incision is made in the patient’s right midabdomen, at or just below the umbilicus. This allows the surgeon’s hands to be at 90 degrees when performing the duodenal anastomosis. Now a 5-mm stapler (Bolder Surgical, Louisville, CO) is being used to perform the anastomosis. If this is the case, then the 3-mm left midquadrant port is exchanged for a 5-mm port ( Fig. 6-2B ). All cannulas have a red rubber sleeve that can be sutured to the skin to prevent them from slipping. In neonates, 3-mm, 20-cm instruments are used. The inflating pressure is set to 10 to 12 mm Hg and the flow at 1 L/min in the neonate. Most infants, even those with cardiac anomalies, tolerate these pressures without difficulty. The liver can be pulled upward by inserting a transabdominal stitch around the falciform ligament ( Fig. 6-3A ). A stitch can also be placed near the dome of the gallbladder next to the liver to provide more retraction ( Fig. 6-3B ). It is rare to have to insert a liver retractor to gain adequate exposure, but, if necessary, this can be introduced in the subxiphoid area.
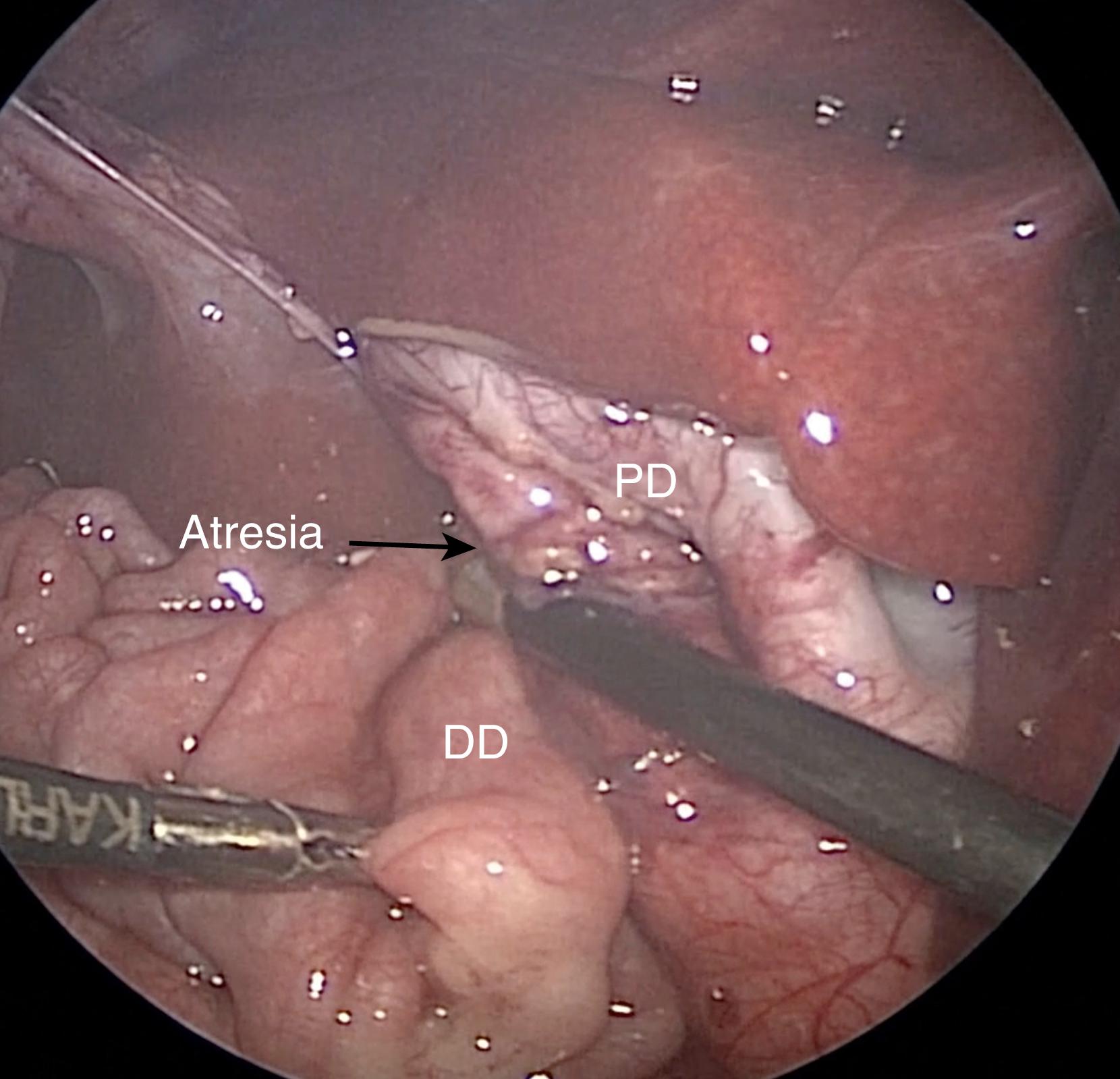
The dilated upper duodenum is easily visualized and is mobilized from any adhesions or Ladd bands. The 3-mm vessel sealer (Bolder Surgical, Louisville, CO) is perfect for performing this portion of the procedure. If unavailable, a 3-mm hook cautery can be used. Next, the smaller distal duodenal segment is identified and mobilized enough to allow a tension-free anastomosis ( Fig. 6-4 ). If necessary, the right colon can be mobilized out of the way. Frequently there is an associated malrotation and a formal Ladd procedure is performed prior to creating the duodenal anastomosis (see Chapter 7 ). Once the anatomy is clearly defined, the enterotomies are made. A transverse duodenotomy is made in the proximal, dilated duodenum and a vertical or longitudinal duodenotomy is made in the distal segment. In most cases, these enterotomies are performed sharply to avoid heat injury to the bowel. A side-to-side anastomosis is then created.
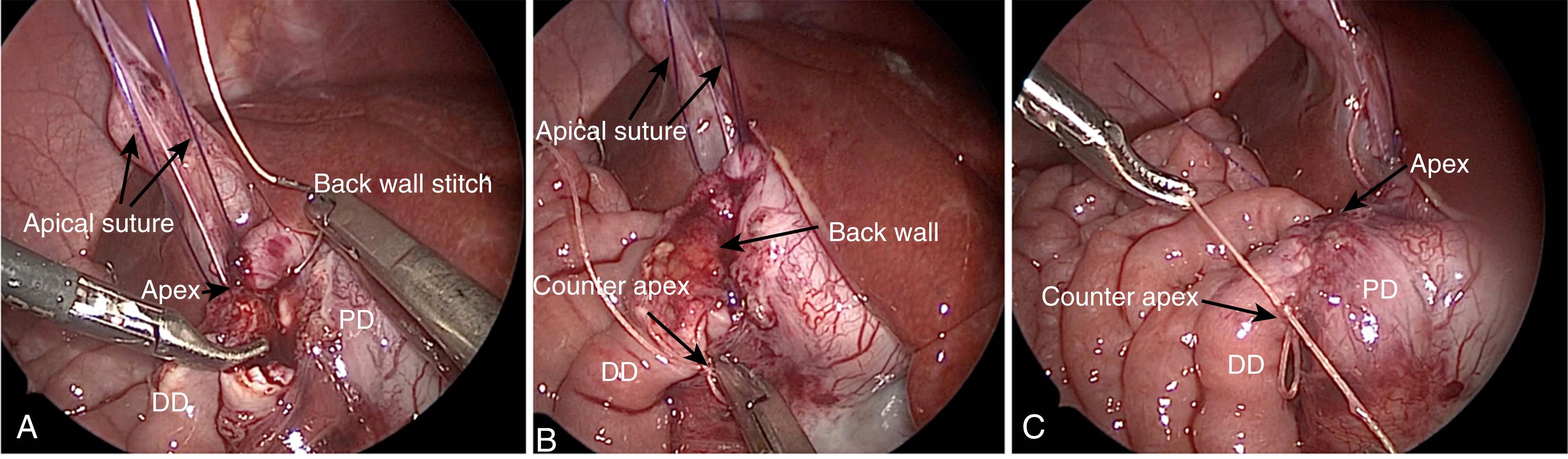
The anastomosis is greatly facilitated by placing a 4-0 transabdominal wall suture in the right upper quadrant through the lateral end on the proximal duodenal incision and the cephalad end of the distal enterotomy. This aligns the two enterotomies and retracts the liver out of the way. The back wall can then be run with a 4-0 or 5-0 Vicryl (Ethicon, Cincinnati, OH) suture on an RB or TF needle, depending on the size of the baby (interrupted sutures can be used if the surgeon prefers) ( Fig. 6-5A ). The suture is started intraluminally and then exteriorized at the bottom of the anastomosis and tied to itself ( Fig. 6-5B ). The front wall is then run with a second suture ( Fig. 6-5C ). A separate stitch can be placed at the end of the anastomosis and used to align the distal ends (and also to tie the running suture to) if the surgeon is uncomfortable tying the running suture to itself. A diamond-shaped anastomosis can be performed if the surgeon prefers but is a bit more technically difficult, and current data shows there is no advantage in terms of time to feeds. If desired, anastomotic patency can be checked by asking the anesthesiologist to insufflate 50 mL of air into the stomach. By doing so, a second membranous duodenal obstruction can be excluded as well.
Although common in the open procedure, tapering of the proximal duodenum is no longer considered necessary as bowel function seems to return quite rapidly following the laparoscopic approach.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here