Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
The use of laparoscopy in pediatric urology has evolved over the past 30 years. Beginning in the 1980s, with diagnostic laparoscopy for cryptorchidism, indications have expanded from straightforward laparoscopic procedures such as ligation of the spermatic vessels to extirpative procedures, with the first laparoscopic nephrectomy being reported in an adult patient in 1991. In 1995, Peters reported the first laparoscopic pyeloplasty in a child, and the era of reconstructive pediatric laparoscopic urology began.
While progress was slow in the last decade of the 20th century, the laparoscopic approach in pediatric urology has become increasing implemented in the first two decades of the 21st century with refinements in available technology and the use of robotic applications. Today, indications for the laparoscopic approach include the complete spectrum of pediatric urological anomalies of the upper and the lower urinary tracts. Some of these laparoscopic approaches are now considered to be the standard of care.
The laparoscopic transperitoneal approach offers a maximum working space (when compared with retroperitoneoscopy) and is suitable for all age and weight groups, ranging from the newborn to the adolescent patient.
Following informed consent, general anesthesia with muscle relaxation is administered. A urinary catheter is inserted to control urinary drainage and provide an empty bladder for improved working space and visualization. A single dose of a perioperative antibiotic is given.
The patient is placed supine on the operating table and the flank of the affected side may be slightly elevated with a gel pad or similar device. The screen is positioned on the side that will be operated on, and additional monitors are positioned as needed to facilitate the view for the assistant surgeon, scrub nurse, anesthetist, and so forth. To provide an ergonomic posture for the surgeon, the monitors can be tilted somewhat downward so that the surgeon’s view is directed downward as in an open operation. The surgeon is situated on the opposite side of the patient while the assistant surgeon driving the camera is standing or seated next to the surgeon, with both surgeons looking in the direction of the operating field. The scrub nurse is standing across the surgeon on the patient’s opposite side.
For access to the abdominal cavity, we prefer a cutdown technique at the inferior edge of the umbilicus. A 5- or 10-mm cannula is then inserted followed by introduction of an angled telescope. Following creation of the pneumoperitoneum, two 3- or 5-mm working ports are then inserted in the upper and lower abdomen on the affected side. In general, triangulation of the ports/instruments should be the goal with respect to the renal pelvis. To gain access to the affected kidney, Gerota’s fascia is opened via either a retro-colonic or a transmesocolic route.
Ureteropelvic junction obstruction (UPJO) is the most common cause of hydronephrosis in infants and children. Historically, the preferred approach for surgical management of this condition was an opened dismembered pyeloplasty through a retroperitoneal approach as described by Anderson and Hynes. Laparoscopic dismembered pyeloplasty offers improved visualization of the anatomy, accurate anastomotic suturing, and precise reconstruction of the UPJO with good functional results. Our feeling is that the laparoscopic transperitoneal dismembered pyeloplasty is now the optimum approach for surgical treatment of UPJO in children.
Indications for pyeloplasty include a differential renal function (DRF) on the affected side below 40%; a decrease in DRF documented on more than one examination, such as a renal scintigram or magnetic resonance imaging (MRI); relevant urodynamic obstruction on renal scintigram or MRI; recurrent urinary tract infection (UTI) and/or pyelonephritis; subjective patient complaints, such as flank pain; and special anatomic conditions such as horseshoe kidney with obstruction. The aim of any reconstructive pyeloplasty is to maintain the DRF and to improve urinary drainage. Preoperative workup includes ultrasound, diuretic renal scintigram, and/or MRI. At the same time, intravenous pyelogram is considered to be obsolete in today’s management of this condition and should be restricted to selected and complex patients.
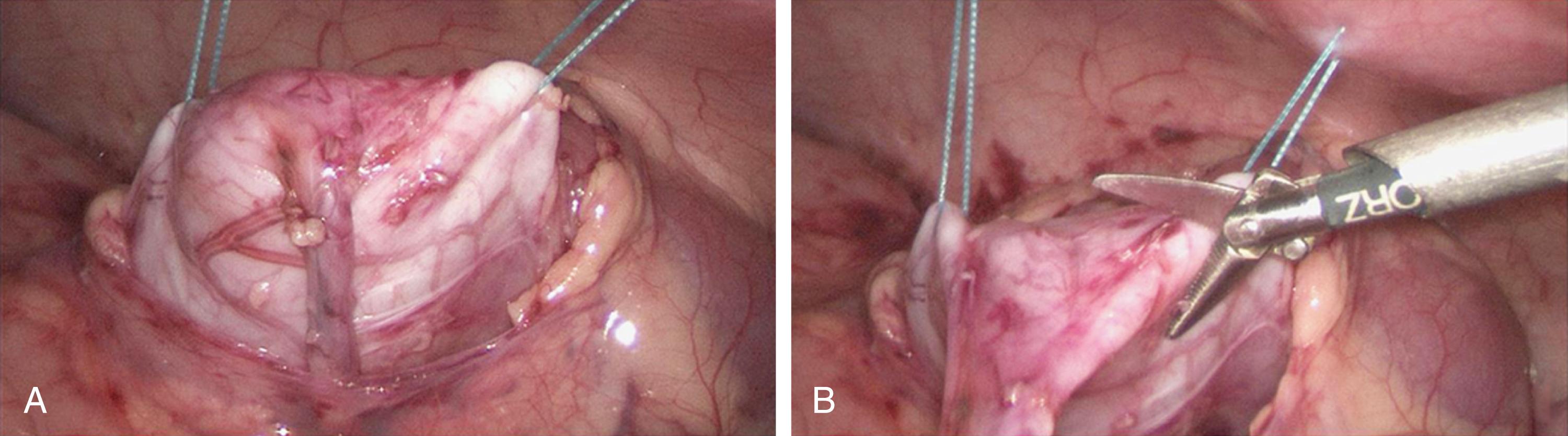
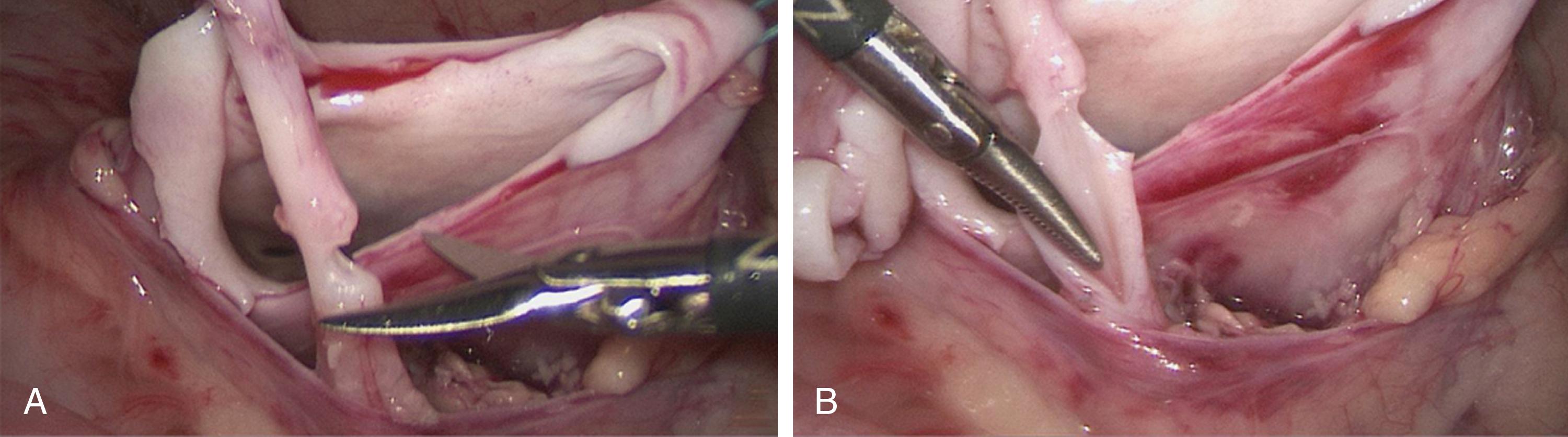
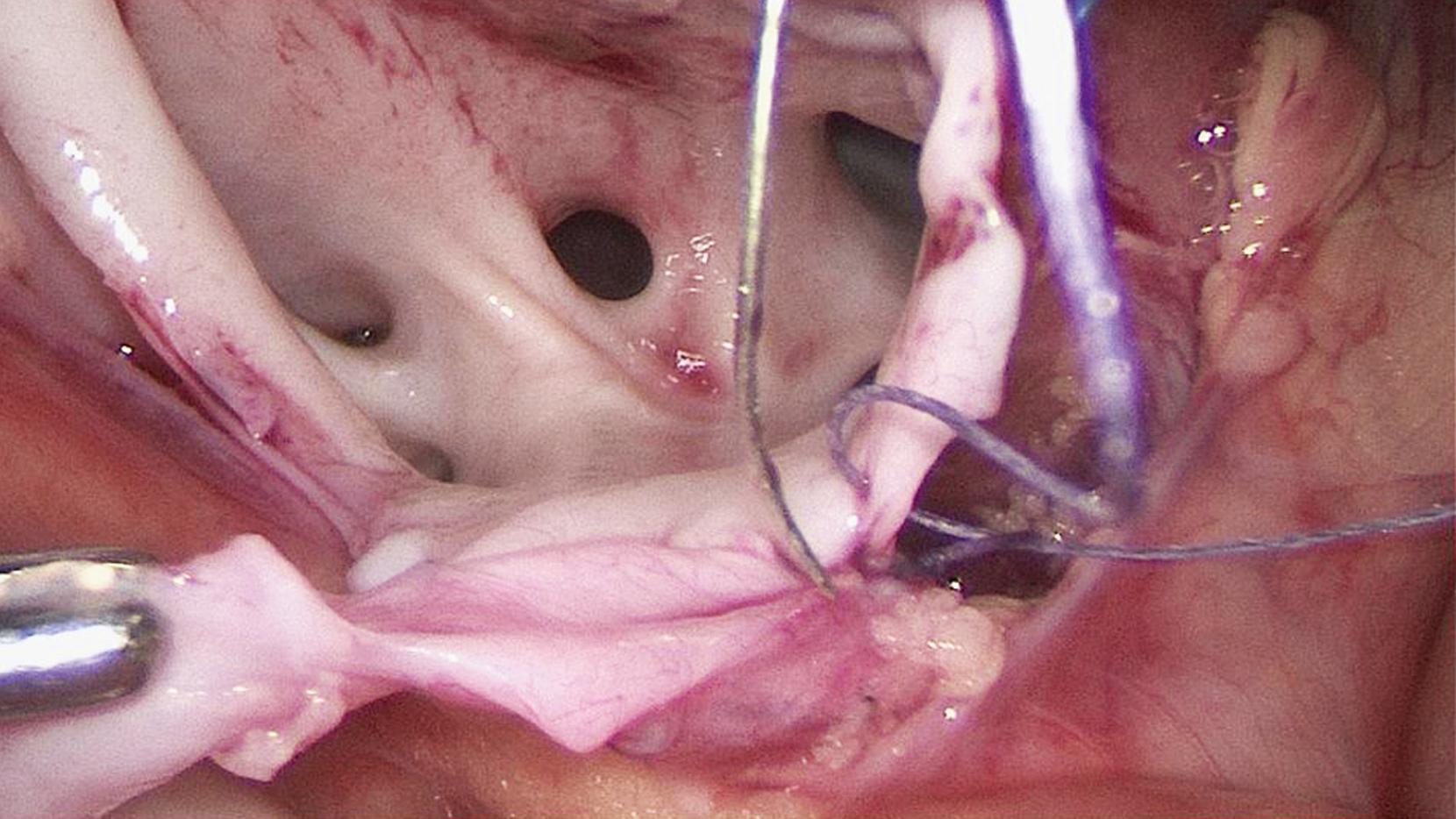
Following incision of Gerota’s fascia, blunt/sharp dissection is then utilized to expose the dilated renal pelvis. As soon as it becomes visible, an attempt is made to grasp the pelvis and then further dissect it, again using blunt and/or sharp technique with electrocautery, scissors, the ultrasonic scalpel, or a similar device. When the renal pelvis along with the UPJ has been sufficiently exposed, two transabdominal hitch sutures will help to further expose the dilated renal pelvis. These sutures should be placed with care, with one suture at the upper part of the renal pelvis, safely sparing the renal hilar vessels, and a second suture at the lower aspect of the renal pelvis lateral to the UPJ, so that the resection of the renal pelvis, along with the UPJ, can be carried out between these hitching sutures ( Fig. 28-1 ). After resection of the dilated renal pelvis, the ureter is incised well below the UPJ but not cut completely. It is then spatulated on its lateral aspect to provide a sufficient length of ureteral wall for achieving a wide side-to-side anastomosis ( Fig. 28-2 ). The idea behind leaving part of the renal pelvis, UPJ, and proximal ureter in place and not resecting them at this time is that this tissue may be used as a “handle” during the anastomotic suturing. Also, such an approach will avoid grabbing and injuring the ureteral tissue during the suturing.
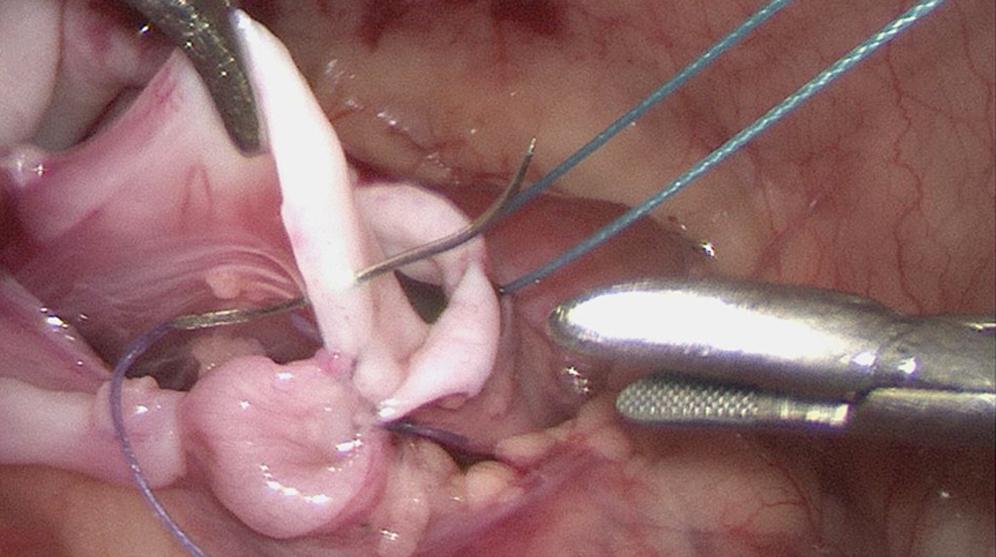
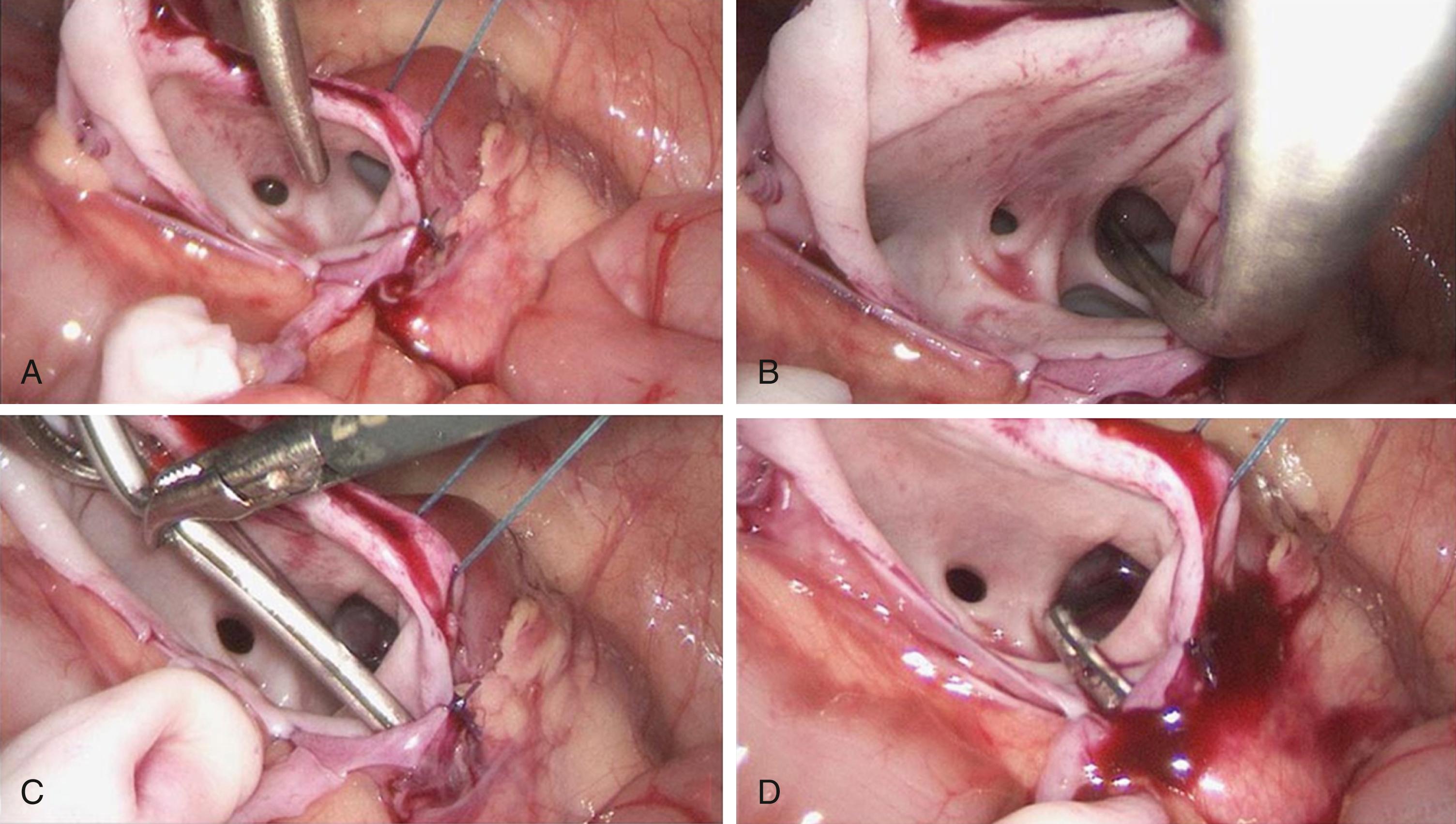
A side-to-side anastomosis is then performed starting with the back side ( Fig. 28-3 ). The anastomosis can be performed with either single interrupted sutures or running sutures. The single interrupted sutures will offer more safety in achieving a watertight anastomosis and may be more tissue sparing as well. On the other hand, the running suture will likely save operative time but requires constantly applying tension to the suture to avoid it coming loose, which could lead to an anastomotic leak. A 5-0 suture can be used as a running suture in all age groups. However, we prefer to use 6-0 braided suture in infants and 5-0 braided suture in older patients as interrupted sutures. An inverting suturing technique is recommended to avoid exposing any suturing material to the ureteral lumen as this might cause crystallization followed by bacterial colonization. After completing the back side of the anastomosis, the patency of the anastomosis should be checked before securing the front wall ( Fig. 28-4 ).
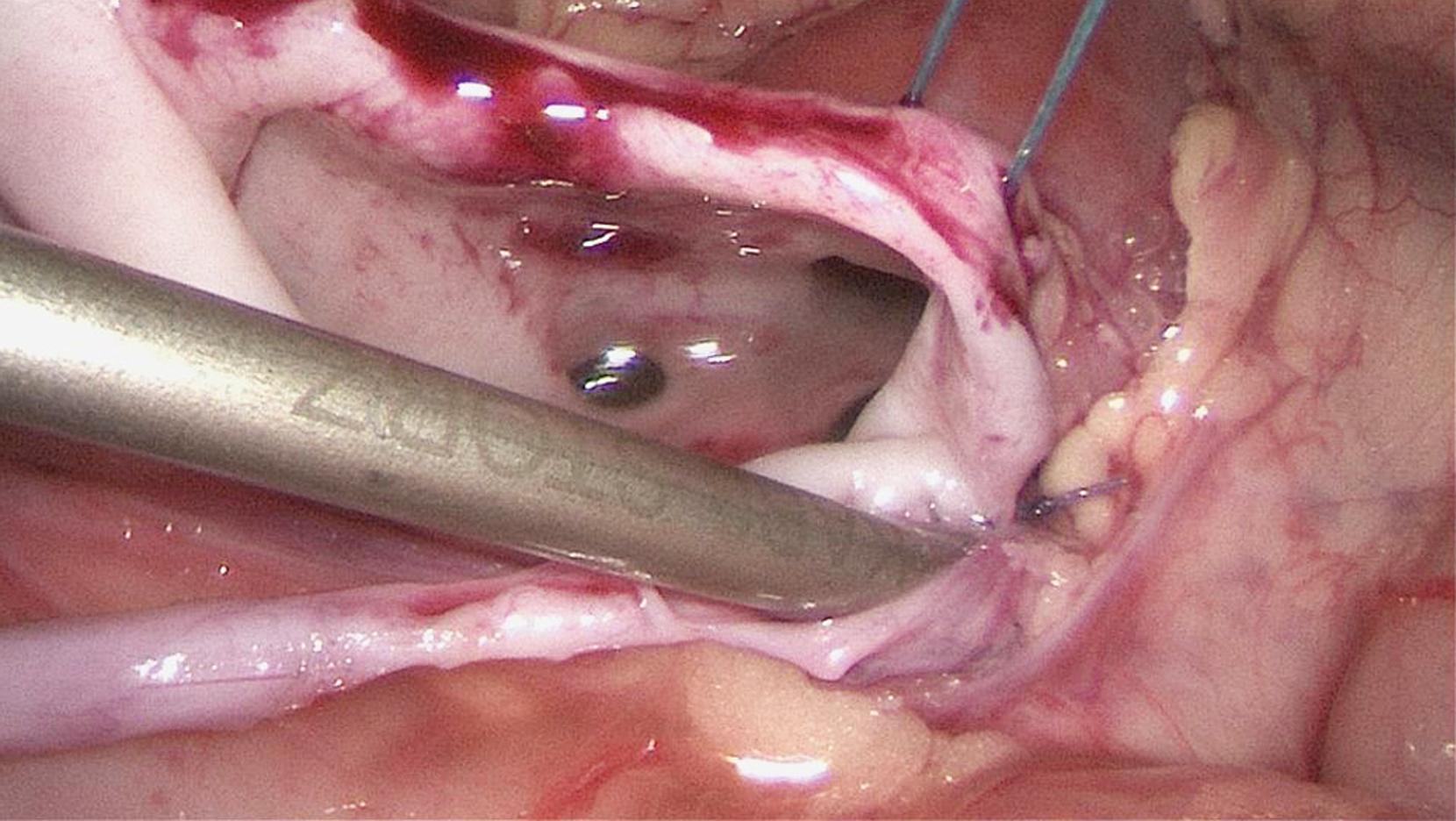
The anterior aspect of anastomosis is then completed ( Fig. 28-5 ). There is ongoing discussion whether to stent the anastomosis and, if so, what type of stent to use. We prefer using a transabdominal, transanastomotic stent. After creating the back wall of the anastomosis, a 6 to 8 Fr stent is introduced through the ventral abdominal wall using a curved, custom-made device. It is then brought into the open renal pelvis, through an identified calyx, and then punctured out through the renal parenchyma and the lateral abdominal wall. The other end of the catheter, which is extracorporeal, is then pulled into the abdominal cavity and threaded into the distal ureter ( Fig. 28-6 ). When ready, the stent is removed by pulling the it out of the patient and this does not require cystoscopy and a second general anesthesia for removal as is necessary if a double J stent technique is used. Following stent placement, the remaining open renal pelvis can be closed using a running suture or “Z-tie” single interrupted sutures ( Fig. 28-7 ). A wide side-to-side anastomosis with a newly created patent UPJ is thus created.
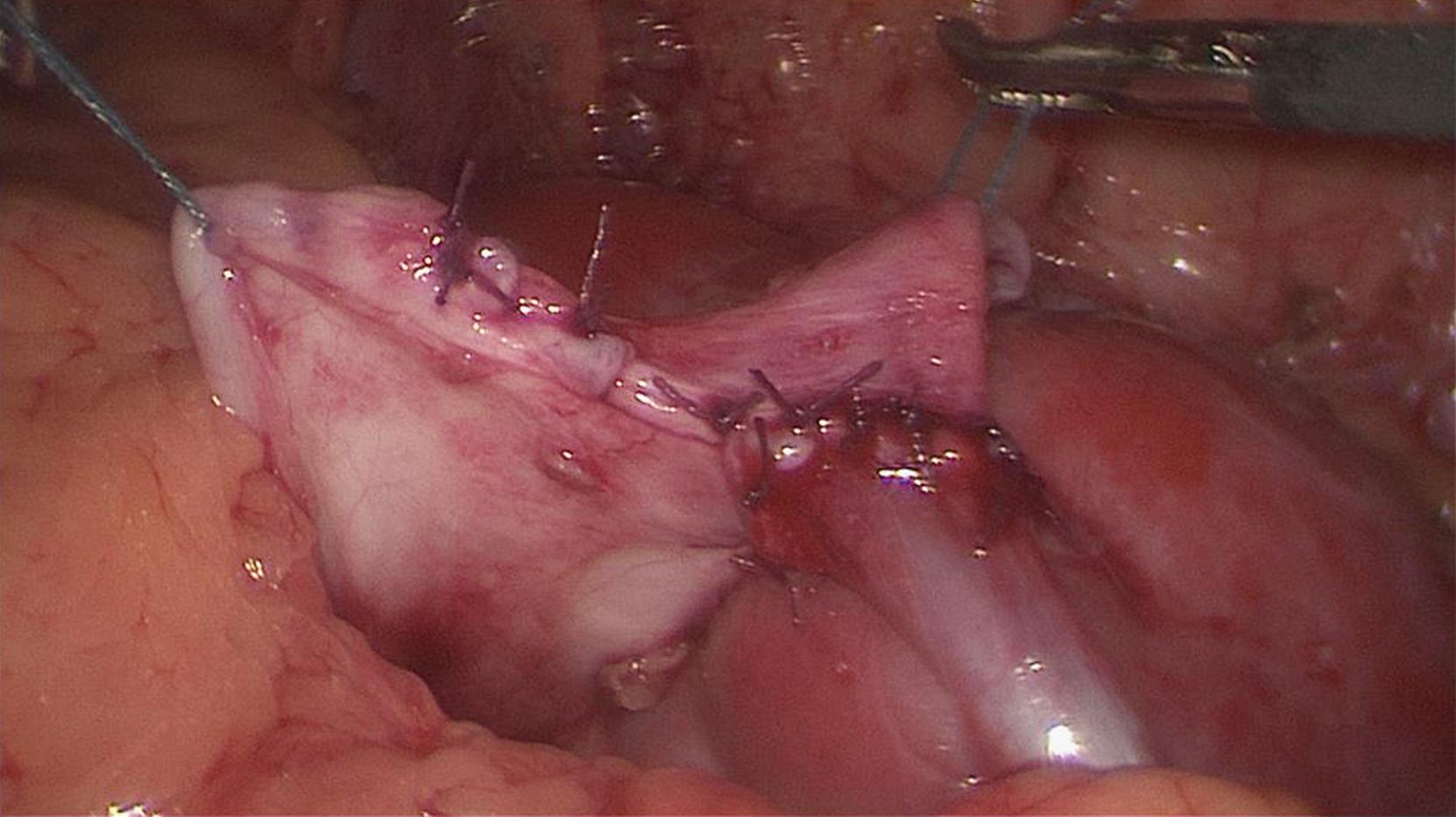
In addition, this type of stenting allows retrograde irrigation intraoperatively to evaluate the security of the anastomosis. Options for stenting include double J stents, percutaneous nephrostomy stents, and other options. The hitching sutures are now removed, the kidney is repositioned, and the mobilized bowel is returned to its original position. Additional drainage is not usually needed. The resected specimen and UPJ are removed from the abdomen along with the working ports.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here