Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
The primary and most frequent indication for surgical treatment of intussusception is failure of radiologic reduction. If the condition of the patient allows, the reduction attempt should be repeated up to three times before surgical intervention is initiated. Enema reduction should be performed in all cases (unless free air is present) because, even in unsuccessful cases, a partial reduction of the intussusception may increase the success rate for operative reduction. The second indication for laparoscopic treatment is the presence of jejunoileal or ileoileal intussusceptions that do not resolve spontaneously.
Adequate preoperative resuscitation with intravenous fluids is important. Because of the possibility of bacterial translocation due to stasis and bowel wall ischemia, we administer a dose of preoperative prophylactic broad-spectrum antibiotics. Since most children who require operative treatment of intussusception present with bowel obstruction, rapid-sequence intubation with measures to avoid aspiration is also important.
In cases of bowel necrosis or perforation, the antibiotics are continued for 24 hours postoperatively. Based on our experience, laparoscopic management is feasible in almost all cases. Only patients who present with signs of peritonitis, sepsis, or a massively distended abdomen that precludes safe placement of trocars/cannulas or obtaining an adequate operative space may not be suitable candidates for the laparoscopic approach.
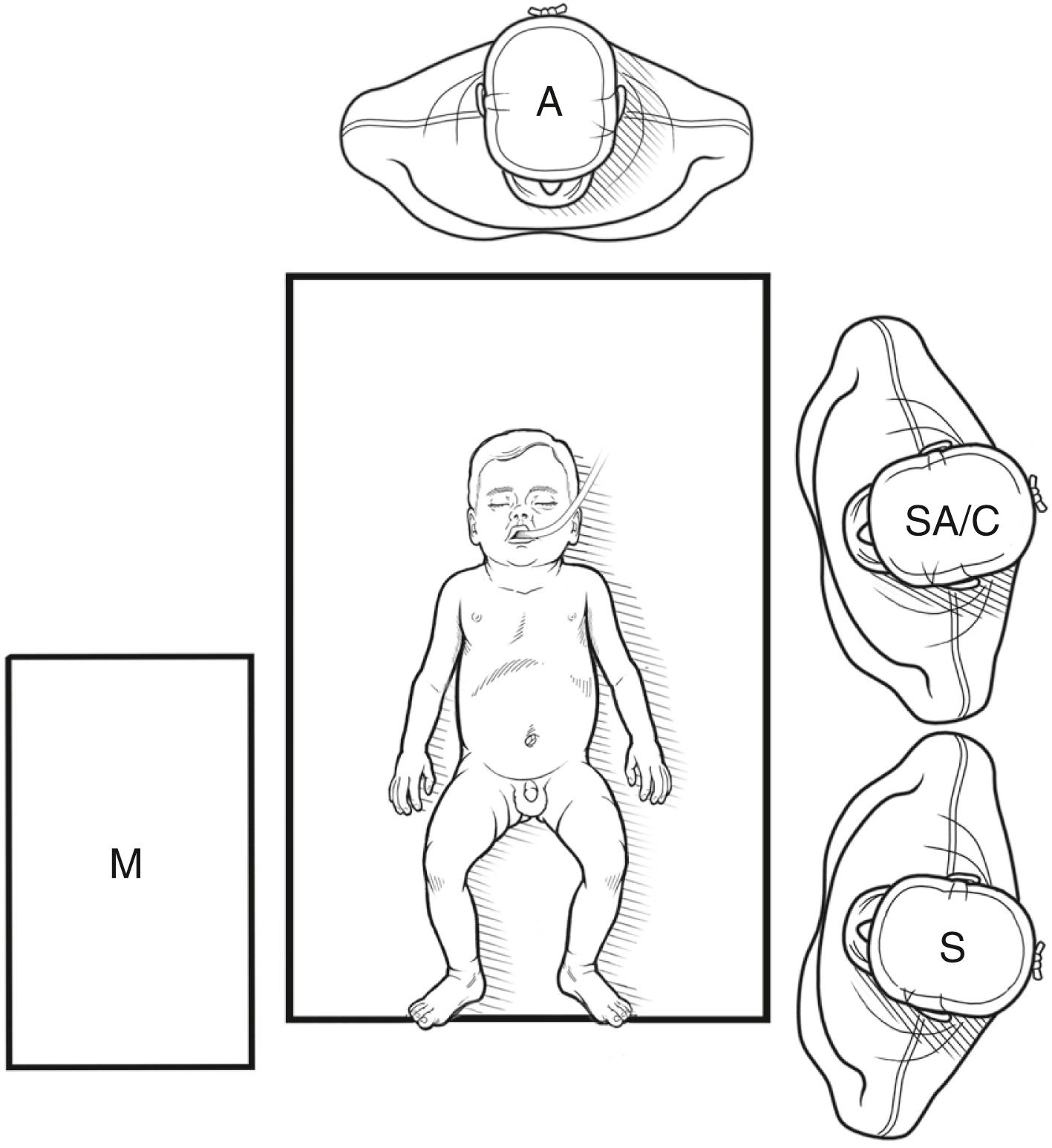
A nasogastric tube should be inserted to avoid vomiting and aspiration before initiating general anesthesia. As with most other laparoscopic operations, the patient is positioned supine. The position of the surgeon and the assistant are at the left of side of the patient, similar to the setup for appendectomy ( Fig. 9-1 ). The scrub nurse stands at the foot of the bed to the left of the assistant.
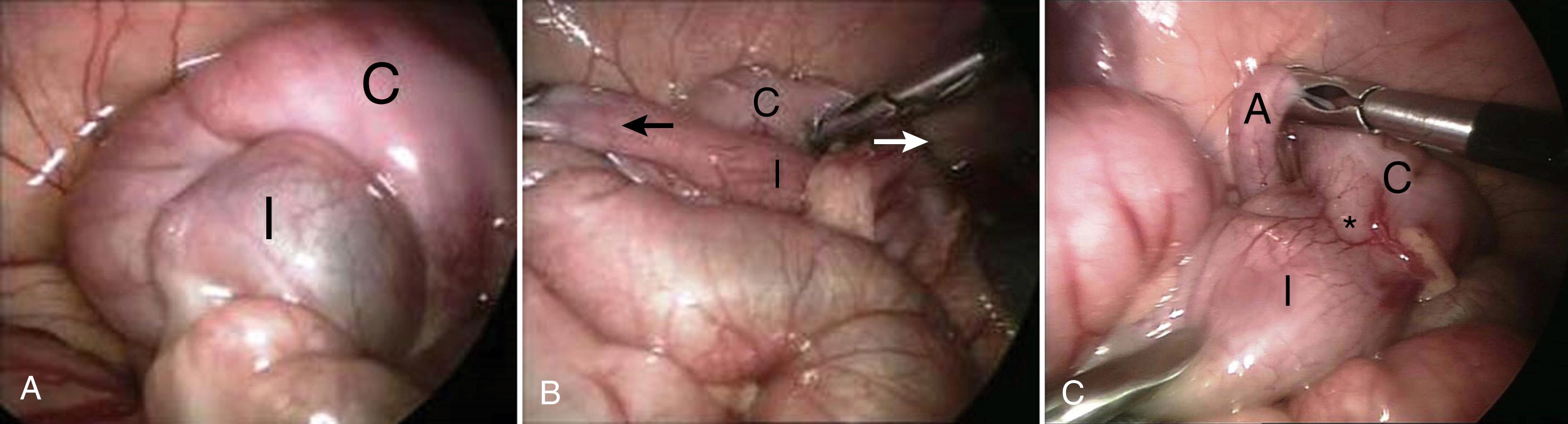
Traditionally, the three-port approach was performed ( Fig. 9-2 ). With this approach, the first cannula is inserted in the navel for the laparoscope and camera, and the abdomen is then inspected to identify the location and extent of the intussusception ( Fig. 9-3A ). The working ports are then introduced under vision in the suprapubic region and the epigastrium. These port positions are adapted to the patient’s findings. For example, if the intussusceptum has progressed to the hepatic flexure or beyond, it may be more ergonomic to place the cranial working port toward the left upper quadrant. Both 3-mm and 5-mm instruments can be used for the attempted reduction, but the larger instruments have the advantage that they provide a more generous purchase on the tissues, thereby causing less focal trauma and decreasing the risk of bowel injury. Using long 5-mm bowel graspers also allows for a laparoscopic retrograde milking of the intussusceptum (Hutchinson maneuver), emulating a technique that is often used in the open approach.
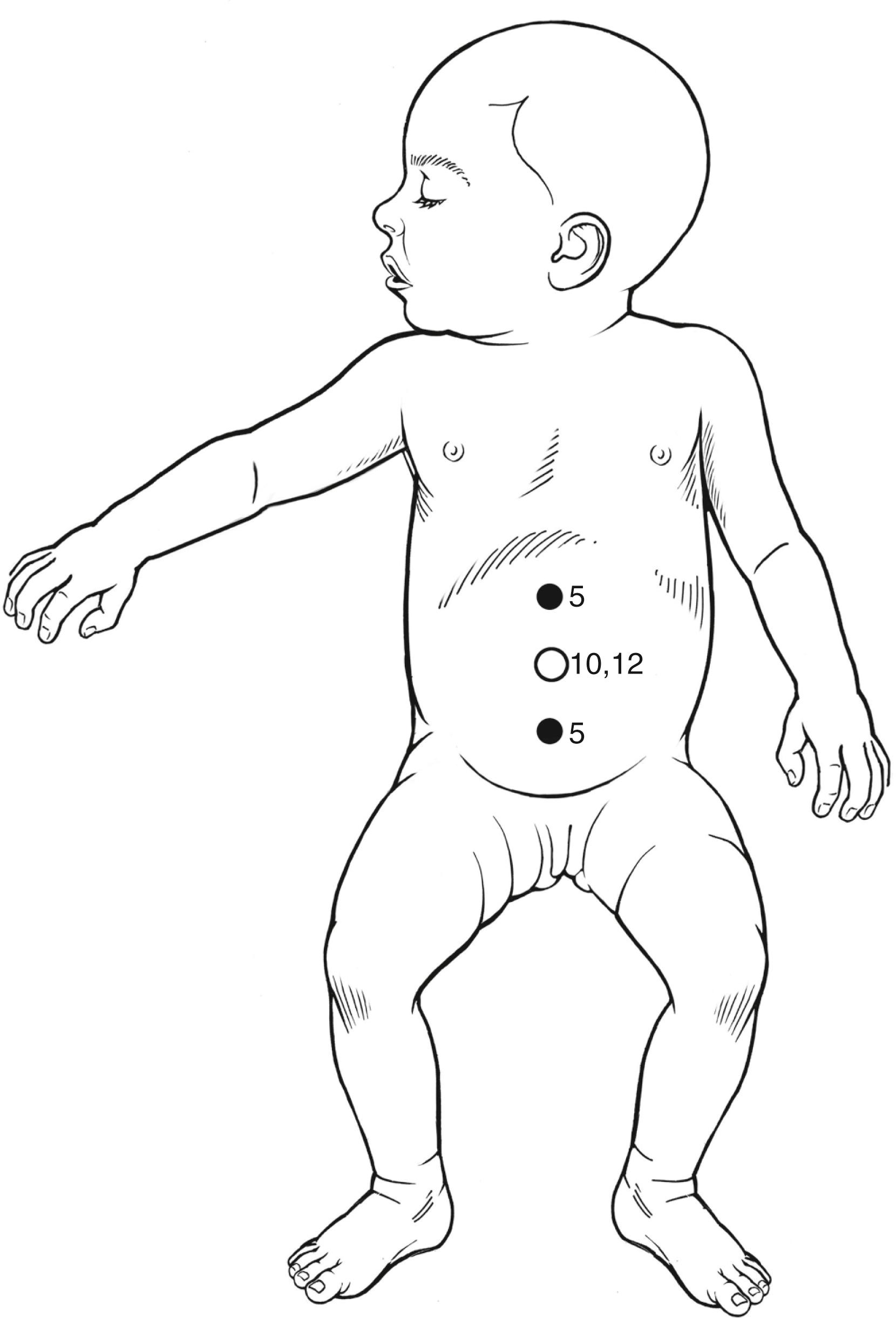
An alternative to the conventional, triangulated multiport laparoscopy is the single-incision technique, which has become the current standard in our department. We place a proprietary single-incision port into a 1.5- to 2-cm vertical incision in the umbilicus via an open entry technique. Most intussusceptions can be identified and managed through this access site alone. If the attempted reduction is difficult, additional ports can and should be added proactively to aid in the reduction. In general, only atraumatic graspers should be used.
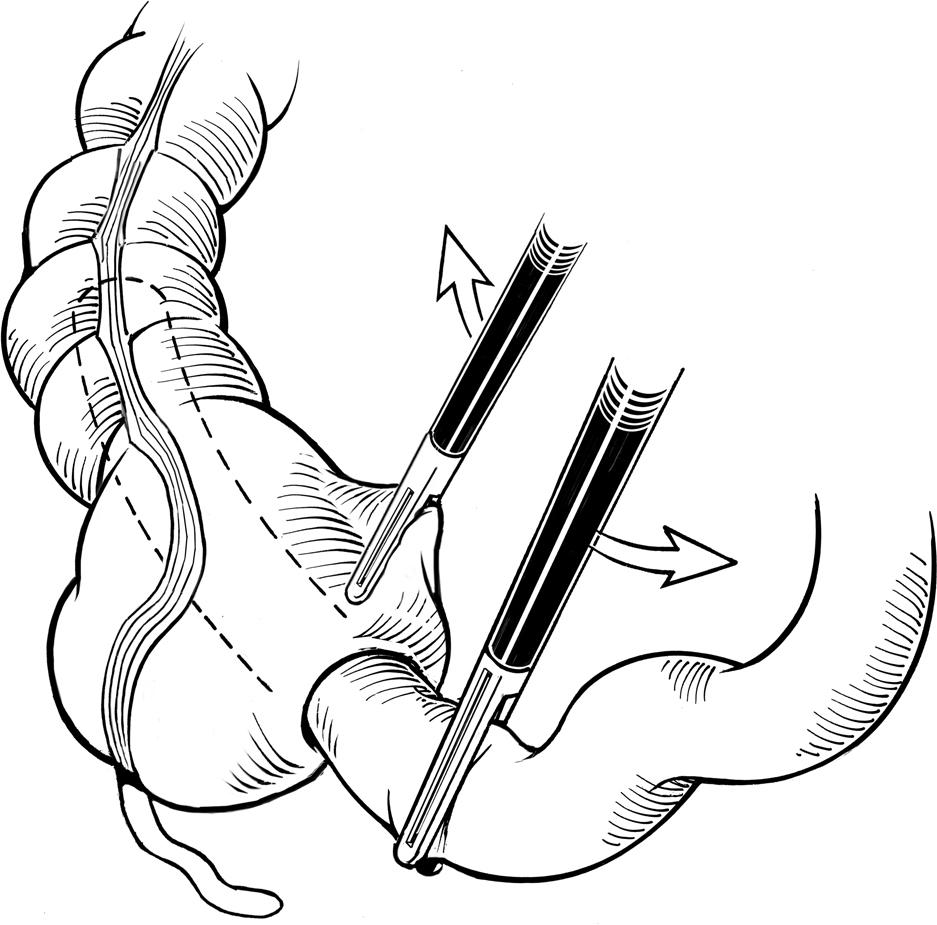
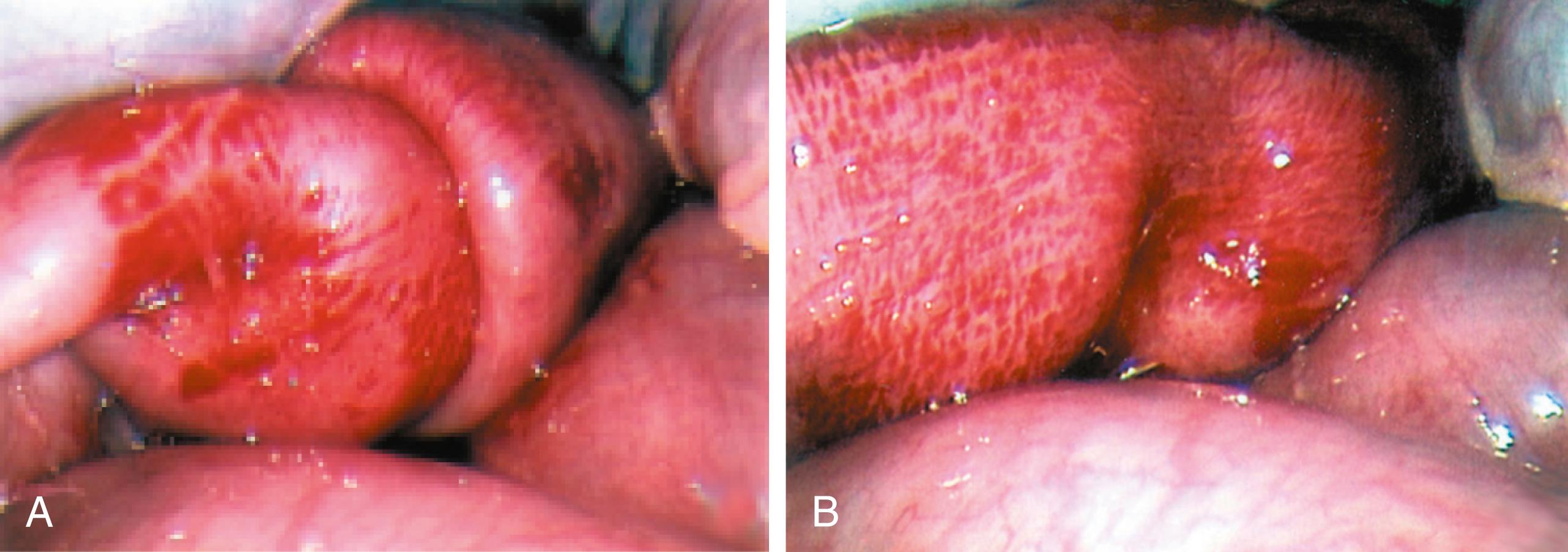
Regardless of the approach utilized, and in contrast to established opinion that distraction should be avoided in laparoscopic reduction of intussusceptions, our experience corroborates other reports that a combination of gentle continuous traction can be used safely if certain caveats are observed: First, continuous traction along the axis of the intussusception is facilitated by gently grasping a large portion of the intussuscepted small bowel with the surgeon’s left hand. The second grasper in the surgeon’s right hand is then to “roll” the proximal edges of the intussuscipiens distally over the intussusceptum ( Figs. 9-3B and 9-4 ). Alternatively, a large, long, blunt bowel grasper can be used to gently “squeeze” the distal end of the intussusceptum proximally through the bowel wall in a modified Hutchinson maneuver. The important point is that gentle continuous traction with the left hand is maintained at all times so that the edema can gradually subside and ground is not lost due to reintussusception of already reduced bowel. The procedure is continued until the entire intussuscepted bowel is reduced ( Figs. 9-3C and 9-5 ).
Traditionally, an appendectomy has been performed, especially with the open operation. In contrast, we inspect the appendix and leave it in situ if it looks macroscopically normal. If in doubt, a laparoscopic appendectomy can be performed.
If laparoscopic reduction cannot be achieved in a reasonable time period (20 to 30 minutes) or a complicated intussusception is suspected ( Fig. 9-6A ), conversion to an open technique is indicated. The risk of conversion is elevated in the presence of a lead point, and therefore the reduced/resected bowel should be inspected carefully in such cases.
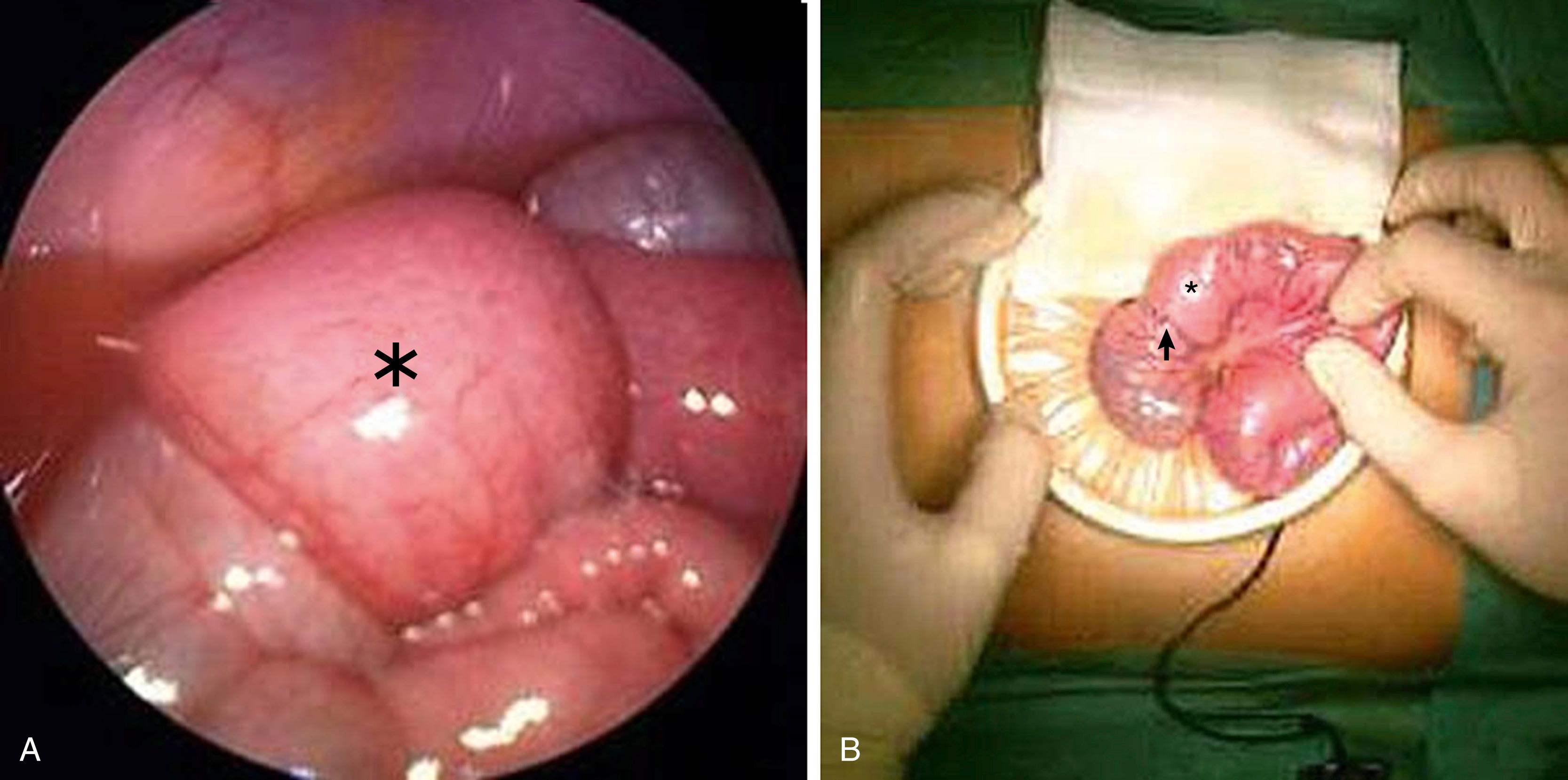
Conversion to the open technique has been traditionally performed by making an additional right lower quadrant horizontal incision that allows direct access to the cecum and ascending colon. An alternative approach is to gain access through the umbilical incision that is enlarged in the craniocaudal direction as much as is necessary to deliver the mass after it has been mobilized laparoscopically ( Fig. 9-6B ). To exteriorize the intussuscepted bowel, it is helpful to first mobilize the right colon medially by laparoscopic division of the colonic attachments along the white line of Toldt.
Since the resection of an intussusception implies the removal of a substantial length of bowel, it is prudent to attempt an open manual reduction before any bowel is resected laparoscopically. Open manual reduction allows for more tactile feedback when using the Hutchinson maneuver and allows the surgeon to feel for possible lead points. A standard, primary end-to-end or a stapled side-to-side anastomosis is performed if bowel resection is needed. The resected mass should be sent for histopathologic analysis to evaluate for a pathologic or malignant lead point. Iliopexy has not been shown to reduce the rate of recurrences and therefore is not necessary.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here